Abstract
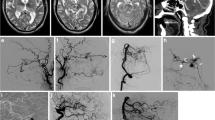
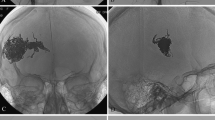
Ethylene-vinyl alcohol copolymer (Onyx) has been proposed as a suitable alternative embolic agent in the management of craniofacial arteriovenous malformations (CFAVM). Short-term efficacy studies have demonstrated promising results with good nidus penetration on post-treatment angiography. This article reports the histopathologic findings of direct vascular recanalization with Onyx at the time of surgical resection. A retrospective review of eight patients who underwent Onyx embolization followed by surgical excision for CFAVM was performed. The surgical specimens were evaluated for the presence of recanalized blood vessels in the embolic cast material and inflammatory changes. A total of 8 patients (mean age 31 years, range 15–57 years) underwent 25 CFAVM embolization and 16 surgical specimens were taken. The time period between initial Onyx embolization and surgery ranged from 12 months to 108 months. Onyx was identified in all of the 16 specimens at the time of resection. Recanalization was identified in 12 of the 16 specimens (75%). Chronic inflammatory changes were present in 13 of the 16 specimens (81.25%) ranging from mild (8) and moderate (4) to severe (1). Giant cells were present in 15 of the 16 specimens (93.75%). Staged Onyx embolization has been reported as clinically efficacious in the management of CFAVM with permanent occlusive properties. Recanalization was commonly seen in this patient cohort as early as 12 months after initial endovascular treatment. Further studies are needed to confirm these findings to evaluate the permanence of Onyx as single agent management for CFAVM.
Zusammenfassung
Ethylen-Vinylalkohol-Copolymer (Onyx) wurde als geeigneter alternativer Wirkstoff für die Embolisation zur Behandlung kraniofaszialer arteriovenöser Malformationen (CFAVM) eingeführt. Kurzzeitstudien zur Wirksamkeit haben vielversprechende Ergebnisse mit guter Niduspenetration in der Angiographie nach der Behandlung gezeigt. Dieser Beitrag berichtet über die histopathologischen Befunde der direkten vaskulären Rekanalisation mit Onyx zum Zeitpunkt der chirurgischen Resektion. Ein retrospektives Review von 8 Patienten, die sich einer Embolisation mit Onyx gefolgt von einer chirurgischen Exzision aufgrund CFAVM unterzogen, wurde durchgeführt. Die während der Operation entnommenen Proben wurden auf das Vorliegen rekanalisierter Blutgefäße im embolischen Cast-Material und entzündliche Veränderungen untersucht. Insgesamt 8 Patienten (mittleres Alter: 31 Jahre, Range: 15–57 Jahre) unterzogen sich 25 CFAVM-Embolisationen, und 16 chirurgische Proben wurden entnommen. Der Zeitraum zwischen der ersten Onyx-Embolisation und der Operation lag zwischen 12 und 108 Monaten. In allen 16 Proben wurde Onyx zum Zeitpunkt der Resektion identifiziert. Eine Rekanalisation wurde in 12 von 16 Proben (75 %) festgestellt. Chronische entzündliche Veränderungen lagen in 13 von 16 Proben (81,25 %) vor und reichten von mild (8) und moderat (4) bis hin zu schwer (1). Riesenzellen lagen in 15 von 16 Proben vor (93,75 %) vor. Die stufenweise Onyx-Embolisation wurde als klinisch wirksam in der Behandlung von CFAVM mit permanenten okklusiven Eigenschaften angegeben. Eine Rekanalisation wurde in dieser Patientenkohorte häufig schon 12 Monate nach der ersten endovaskulären Behandlung festgestellt. Weitere Studien sind notwendig, um diese Ergebnisse zu bestätigen und die langfristige Wirkung von Onyx als Einzelwirkstoff zur Behandlung von CFAVM zu beurteilen.






Similar content being viewed by others
References
Aburniya T, Sasaguri T, Taba Y, Miwa Y, Miyagi M (2002) Shear stress induces expression of vascular Endothelia growth factor Flk-1/KDR through the CT-rich sp1 binding site. Arterioscler Thromb Vasc Biol 22(6):907–913
Arat A, Cil BE, Vargel I, Turkbey B, Canyigit M, Peynircioglu B, Arat YO (2007) Embolization of high-flow craniofacial vascular malformations with onyx. Ajnr Am J Neuroradiol 7:1409–1414
Avwioro G (2011) Histochemical uses of Haematoxylin—A review. Int J Pharmacol Clinc Sci 1:24–34
Blanco R, Gerhardt H (2013) VEGF and Notch in Tip and stalk cell selection. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a006569
Buell TJ, Ding D, Starke RM, Crowley W, Liu KC (2014) Embolization-induced Angiogenesis in cerebral Arteriovenous malformations. J Clin Neurosci 21:1866–1871
Chen Y, Pawlikowska L, Yao JS et al (2006) Interleukin-6 Involvement in Brain Arteriovenous Malformations. Ann Neurol 59:72–80
Chen Y, Zhu W, Bollen AW et al (2008) Evidence of inflammatory cell involvement in brain Arteriovenous malformations. Neurosurgery 62(6):1340–1650
Dabus G, Linfante I, Benenati J et al (2016) Interventional management of high-flow craniofacial vascular malformations: a database analysis and review of literature. J Neurointervent Surg 0:1–5
Danese S, Dejana E, Fiocchi C (2007) Immune regulation by Microvascular Endothelial cells: directing innate and adaptive immunity, coagulation, and inflammation. J Immunol 178:6017–6022
Dee D, Grzybicki D, Dobbs M et al (2000) Interleukin-6 promotes Vasculogenesis of murine brain Microvessel Endothelial cells. Cytokine 12(6):655–665
Fearson JA (2010) Discussion: Extracranial Arteriovenous malformations: natural progression and recurrence after treatment. Plast Reconstru Surg 125(4):1195–1196
Jahan R, Murayma Y, Gobin PY, Duckwilder GR, Vinters HV, Vinuela F (2001) Embolization of Arteriovenous malformations with onyx: Clinicopathological experience in 23 patients. Neurosurgery 48(5):984–997
Kohout MP, Hansen M, Pribaz JJ, Mullikwen JB (1998) Arteriovenous malformations of the head and neck: natural history and management. Plast Reconstr Surg 102(3):643–654
Li A, Dubey S, Varney ML, Dave BJ, Signh RK (2003) IL-8 directly enhanced Endothelial cell survival, proliferation, and matrix Metalloproteinases production and regulated Angiogenesis. J Immunol 170:3369–3376
Lin X, Chen D, Jin Y et al (2014) Angioarchitecture of Extracranial Arteriovenous malformations: a vascular casting study. Ann Plast Surg 73:43–48
Liu AS, Mulliken JM, Zurakowski D, Fishman SJ, Greene AK (2010) Extracranial arteriovenous malformations: natural progression and recurrence after treatment. Plast Reconstru Surg 125(4):1185–1194
Lu L, Bischoff J, Mulliken JB, Bielenberg DR, Fishman SJ, Greene AK (2011) Progression of Arteriovenous malformation: possible role of Vasculogenesis. Plast Reconstr Surg 128(4):260–269
Murayama Y, Vinuela F, Ulhoa A, Akiba Y, Duckwilder GR, Gobin YP, Vinters HV, Greff RJ (1998) Nonadhesive liquid embolic agent for cerebral Arteriovenous malformations: preliminary Histopathological studies in swine Rete mirabile. Neurosurgery 43(5):1164–1175
Onyx Liquid Embolic System: [Instructions for use]. (Revised 2013) EV3 Neurovascular.
Richter GT, Suen JY (2011) Pediatric extracranial arteriovenous malformations. Curr Opin Otolaryngol Head Neck Surg 19:455–461
Richter TG, Friedman AB (2012) Hemangiomas and vascular malformations: current theory and management. Int J Pediatr. https://doi.org/10.1155/2012/645678
Santiago-Delpin EA (2004) The Endothelium and early immune activation: new perspective and interactions. Transplant Proc 36:1709–1713
Thiex R, Wu I, Mulliken JB, Greene AK, Rahbar R, Orbach DB (2011) Safety and clinical efficacy of onyx for embolization of Extracranial head and neck vascular anomalies. Ajnr Am J Neuroradiol 32(6):1082–1086
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Hoss, B. Hollowoa, C.-Y. Fan, B. Fogel and M. Meek declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hoss, M., Hollowoa, B., Fan, CY. et al. Histopathologic analysis of craniofacial arteriovenous malformations following Onyx embolization. Gefässchirurgie 23, 507–512 (2018). https://doi.org/10.1007/s00772-018-0459-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00772-018-0459-8