Abstract
Purpose
We reported our experience in the surgical treatment of a relatively large cohort of patients with occipital lobe epilepsy (OLE). We also carried out a systematic review of the literature on OLE.
Methods
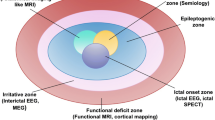
Thirty-five consecutive patients who underwent occipital resection for epilepsy were included. Diagnoses were made following presurgical evaluations, including magnetic resonance imaging (MRI), fluorodeoxyglucose-positron emission tomography (FDG-PET), scalp video-electroencephalogram (EEG) monitoring, and intracranial EEG monitoring. At last follow-up, seizure outcome was classified using the Engel classification scheme.
Results
Twenty-five of 35 patients experienced/had experienced ≥1 type of aura before the seizure. Invasive recordings were used to define the epileptogenic area in 30 of 35 patients (85.7 %). All patients underwent occipital lesionectomies or topectomies. Histopathology revealed: cortical dysplasias, gliosis, dysembryoplastic neuroepithelial tumor, ganglioglioma, and tuberous sclerosis. After a mean follow-up of 44 months, 25 patients (71.4 %) were seizure free (Engel class I), 3 (8.6 %) rarely had seizures (Engel class II), 5 (14.3 %) improved more than 75 % (Engel class III), and 2 (5.7 %) had no significant improvement (Engel class IV). Preoperatively, 12 of 33 patients (36.4 %) had visual field deficits. Postoperatively, 25 patients (75.8 %) had new or aggravated visual field deficits.
Conclusions
The management of OLE has been aided greatly by the availability of high-resolution diagnosis. Postoperative visual field deficits occur in a significant proportion of patients. Comprehensive intracranial EEG coverage of all occipital surfaces helps to define the epileptogenic area and preserve visual function, especially in cases of focal cortical dysplasia undetectable by MRI.


Similar content being viewed by others
References
Anonymity (1991) American Electroencephalographic Society guidelines for standard electrode position nomenclature. J Clin Neurophysiol 8:200–202
Awad IA, Rosenfeld J, Ahl J, Hahn JF, Luders H (1991) Intractable epilepsy and structural lesions of the brain: mapping, resection strategies, and seizure outcome. Epilepsia 32:179–186
Aykut-Bingol C, Bronen RA, Kim JH, Spencer DD, Spencer SS (1998) Surgical outcome in occipital lobe epilepsy: implications for pathophysiology. Ann Neurol 44:60–69
Bidzinski J, Bacia T, Ruzikowski E (1992) The results of the surgical treatment of occipital lobe epilepsy. Acta Neurochir (Wien) 114:128–130
Bien CG, Benninger FO, Urbach H, Schramm J, Kurthen M, Elger CE (2000) Localizing value of epileptic visual auras. Brain 123(Pt 2):244–253
Binder DK, Steinhauser C (2006) Functional changes in astroglial cells in epilepsy. Glia 54:358–368
Binder DK, Von Lehe M, Kral T, Bien CG, Urbach H, Schramm J, Clusmann H (2008) Surgical treatment of occipital lobe epilepsy. J Neurosurg 109:57–69
Blume WT, Whiting SE, Girvin JP (1991) Epilepsy surgery in the posterior cortex. Ann Neurol 29:638–645
Boesebeck F, Schulz R, May T, Ebner A (2002) Lateralizing semiology predicts the seizure outcome after epilepsy surgery in the posterior cortex. Brain 125:2320–2331
Caicoya AG, Macarron J, Albisua J, Serratosa JM (2007) Tailored resections in occipital lobe epilepsy surgery guided by monitoring with subdural electrodes: characteristics and outcome. Epilepsy Res 77:1–10
Carne RP, O’Brien TJ, Kilpatrick CJ, MacGregor LR, Hicks RJ, Murphy MA, Bowden SC, Kaye AH, Cook MJ (2004) MRI-negative PET-positive temporal lobe epilepsy: a distinct surgically remediable syndrome. Brain 127:2276–2285
Clusmann H, Kral T, Schramm J (2006) Present practice and perspective of evaluation and surgery for temporal lobe epilepsy. Zentralbl Neurochir 67:165–182
Conturo TE, Lori NF, Cull TS, Akbudak E, Snyder AZ, Shimony JS, McKinstry RC, Burton H, Raichle ME (1999) Tracking neuronal fiber pathways in the living human brain. Proc Natl Acad Sci USA 96:10422–10427
Dalmagro CL, Bianchin MM, Velasco TR, Alexandre V Jr, Walz R, Terra-Bustamante VC, Inuzuka LM, Wichert-Ana L, Araujo D Jr, Serafini LN, Carlotti CG Jr, Assirati JA Jr, Machado HR, Santos AC, Sakamoto AC (2005) Clinical features of patients with posterior cortex epilepsies and predictors of surgical outcome. Epilepsia 46:1442–1449
Engel J (1993) Surgical treatment of the epilepsies. Raven Press New, York
Foldvary-Schaefer N (2006) Symptomatic focal epilepsies. In: Wyllie E (ed) The treatment of epilepsy: principles and practice. Lippincott Williams & Wilkins, Philadelphia, pp 467–474
Guerreiro MM, Quesney LF, Salanova V, Snipes GJ (2003) Continuous electrocorticogram epileptiform discharges due to brain gliosis. J Clin Neurophysiol 20:239–242
Hua K, Zhang J, Wakana S, Jiang H, Li X, Reich DS, Calabresi PA, Pekar JJ, van Zijl PC, Mori S (2008) Tract probability maps in stereotaxic spaces: analyses of white matter anatomy and tract-specific quantification. NeuroImage 39:336–347
Ibrahim GM, Fallah A, Albert GW, Withers T, Otsubo H, Ochi A, Akiyama T, Donner EJ, Weiss S, Snead OC 3rd, Drake JM, Rutka JT (2012) Occipital lobe epilepsy in children: characterization, evaluation and surgical outcomes. Epilepsy Res 99:335–345
Jobst BC, Williamson PD, Thadani VM, Gilbert KL, Holmes GL, Morse RP, Darcey TM, Duhaime AC, Bujarski KA, Roberts DW (2010) Intractable occipital lobe epilepsy: clinical characteristics and surgical treatment. Epilepsia 51:2334–2337
Kaido T, Hoshida T, Taoka T, Sakaki T (2004) Retinotopy with coordinates of lateral occipital cortex in humans. J Neurosurg 101:114–118
Kim SK, Lee DS, Lee SK, Kim YK, Kang KW, Chung CK, Chung JK, Lee MC (2001) Diagnostic performance of [18F]FDG-PET and ictal [99mTc]-HMPAO SPECT in occipital lobe epilepsy. Epilepsia 42:1531–1540
Kivelev J, Koskela E, Setala K, Niemela M, Hernesniemi J (2012) Long-term visual outcome after microsurgical removal of occipital lobe cavernomas. J Neurosurg 117:295–301
Kral T, Clusmann H, Blumcke I, Fimmers R, Ostertun B, Kurthen M, Schramm J (2003) Outcome of epilepsy surgery in focal cortical dysplasia. J Neurol Neurosurg Psychiatry 74:183–188
Kral T, Clusmann H, Urbach J, Schramm J, Elger CE, Kurthen M, Grunwald T (2002) Preoperative evaluation for epilepsy surgery (Bonn Algorithm). Zentralbl Neurochir 63:106–110
Kun Lee S, Young Lee S, Kim DW, Soo Lee D, Chung CK (2005) Occipital lobe epilepsy: clinical characteristics, surgical outcome, and role of diagnostic modalities. Epilepsia 46:688–695
Kuzniecky R (1998) Symptomatic occipital lobe epilepsy. Epilepsia 39(Suppl 4):S24–S31
Kuzniecky R, Gilliam F, Morawetz R, Faught E, Palmer C, Black L (1997) Occipital lobe developmental malformations and epilepsy: clinical spectrum, treatment, and outcome. Epilepsia 38:175–181
Lee SK, Lee SY, Kim KK, Hong KS, Lee DS, Chung CK (2005) Surgical outcome and prognostic factors of cryptogenic neocortical epilepsy. Ann Neurol 58:525–532
Ludwig BI, Marsan CA (1975) Clinical ictal patterns in epileptic patients with occipital electroencephalographic foci. Neurology 25:463–471
O’Brien TJ, Newton MR, Cook MJ, Berlangieri SU, Kilpatrick C, Morris K, Berkovic SF (1997) Hippocampal atrophy is not a major determinant of regional hypometabolism in temporal lobe epilepsy. Epilepsia 38:74–80
Palmini A, Andermann F, Dubeau F, Gloor P, Olivier A, Quesney LF, Salanova V (1993) Occipitotemporal epilepsies: evaluation of selected patients requiring depth electrodes studies and rationale for surgical approaches. Epilepsia 34:84–96
Palmini A, Najm I, Avanzini G, Babb T, Guerrini R, Foldvary-Schaefer N, Jackson G, Luders HO, Prayson R, Spreafico R, Vinters HV (2004) Terminology and classification of the cortical dysplasias. Neurology 62:S2–S8
Salanova V, Andermann F, Olivier A, Rasmussen T, Quesney LF (1992) Occipital lobe epilepsy: electroclinical manifestations, electrocorticography, cortical stimulation and outcome in 42 patients treated between 1930 and 1991. Surgery of occipital lobe epilepsy. Brain 115(Pt 6):1655–1680
Sereno MI, Dale AM, Reppas JB, Kwong KK, Belliveau JW, Brady TJ, Rosen BR, Tootell RB (1995) Borders of multiple visual areas in humans revealed by functional magnetic resonance imaging. Science 268:889–893
Sturm JW, Newton MR, Chinvarun Y, Berlangieri SU, Berkovic SF (2000) Ictal SPECT and interictal PET in the localization of occipital lobe epilepsy. Epilepsia 41:463–466
Sveinbjornsdottir S, Duncan JS (1993) Parietal and occipital lobe epilepsy: a review. Epilepsia 34:493–521
Tandon N, Alexopoulos AV, Warbel A, Najm IM, Bingaman WE (2009) Occipital epilepsy: spatial categorization and surgical management. J Neurosurg 110:306–318
Tassi L, Colombo N, Garbelli R, Francione S, Lo Russo G, Mai R, Cardinale F, Cossu M, Ferrario A, Galli C, Bramerio M, Citterio A, Spreafico R (2002) Focal cortical dysplasia: neuropathological subtypes, EEG, neuroimaging and surgical outcome. Brain 125:1719–1732
Urbach H, Binder D, von Lehe M, Podlogar M, Bien CG, Becker A, Schramm J, Kral T, Clusmann H (2007) Correlation of MRI and histopathology in epileptogenic parietal and occipital lobe lesions. Seizure 16:608–614
Usui N, Mihara T, Baba K, Matsuda K, Tottori T, Umeoka S, Kondo A, Nakamura F, Terada K, Usui K, Inoue Y (2011) Versive seizures in occipital lobe epilepsy: lateralizing value and pathophysiology. Epilepsy Res 97:157–161
Williamson PD, Thadani VM, Darcey TM, Spencer DD, Spencer SS, Mattson RH (1992) Occipital lobe epilepsy: clinical characteristics, seizure spread patterns, and results of surgery. Ann Neurol 31:3–13
Yun CH, Lee SK, Lee SY, Kim KK, Jeong SW, Chung CK (2006) Prognostic factors in neocortical epilepsy surgery: multivariate analysis. Epilepsia 47:574–579
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, PF., Jia, YZ., Lin, Q. et al. Intractable occipital lobe epilepsy: clinical characteristics, surgical treatment, and a systematic review of the literature. Acta Neurochir 157, 63–75 (2015). https://doi.org/10.1007/s00701-014-2217-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2217-3