Abstract
Background
To review the outcome after endoscopic third ventriculostomy (ETV) for symptomatic, persistent hydrocephalus in three patients with perimesencephalic angiographically negative subarachnoid hemorrhage (PNH) who were dependent on an external ventricular drain (EVD).
Methods
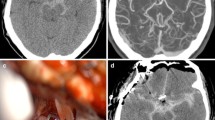
All patients initially presented with severe headache, nuchal rigidity, confusion and lethargy (Hunt-Hess Grade II or III), and persistent, EVD-dependent hydrocephalus. Cranial CT images in each revealed acute hydrocephalus and perimesencephalic hemorrhage pattern with a heavy clot burden (Fisher grade 3). A 3D-CT angiogram on admission and two four-vessel cerebral angiograms failed to demonstrate a bleeding source. All three patients failed trial EVD clamping, with clinical deterioration and elevated intracranial pressure (ICP). ETV was performed with a 0-degree endoscope in a 4.6-mm irrigating sheath using an endoscopic-coring/“cookie-cut” technique. An EVD was left in place for postoperative ICP monitoring but was clamped.
Results
ETV was accomplished in all patients. In one case, a tiny basilar tip aneurysm was seen during the endoscopic procedure. Intraoperatively, the prepontine cistern revealed dense, degraded blood products. Postprocedure ICP measurements were reduced to normal range. Clinical improvement, normal ICP readings, and/or radiographic evidence of resolution of hydrocephalus allowed uneventful removal of the EVD within 36–48 h post-ETV in all patients. All remained headache-free, with a normal neurological examination, during a follow-up period of 10, 11, and 12 months, respectively.
Conclusion
To our knowledge, this is the first report of ETV for PNH with hydrocephalus and the first report of a basilar tip microaneurysm seen intraoperatively during ETV. ETV is a viable treatment option for refractory hydrocephalus secondary to a perimesencephalic pattern of subarachnoid hemorrhage (SAH). Its early application can avoid placement of a ventriculoperitoneal shunt, curtail the extended use of an EVD, and reduce the associated infection risks. Despite thorough angiographic investigation for an aneurysmal cause of SAH, a “microaneurysm” of the basilar artery was found at ETV. No complication or rebleeding was encountered.


Similar content being viewed by others
Abbreviations
- CSF:
-
cerebrospinal fluid
- CT:
-
computed tomographic
- ETV:
-
endoscopic third ventriculostomy
- EVD:
-
external ventricular drain
- ICP:
-
intracranial pressure
- PNH:
-
perimesencephalic angiographically negative subarachnoid hemorrhage
- SAH:
-
subarachnoid hemorrhage
- VP:
-
ventriculoperitoneal
References
Alen JF, Lagares A, Lobato RD, Gomez PA, Rivas JJ, Ramos A (2003) Comparison between perimesencephalic nonaneurysmal subarachnoid hemorrhage and subarachnoid hemorrhage caused by posterior circulation aneurysms. J Neurosurg 98:529–535
Brilstra EH, Hop JW, Rinkel GJ (1997) Quality of life after perimesencephalic haemorrhage. J Neurol Neurosurg Psychiatry 63:382–384
Duong H, Melancon D, Tampieri D, Ethier R (1996) The negative angiogram in subarachnoid haemorrhage. Neuroradiology 38:15–19
Fukuhara T, Shimizu T, Namba Y (2009) Limited efficacy of endoscopic third ventriculostomy for hydrocephalus following aneurysmal subarachnoid hemorrhage. Neurol Med Chir (Tokyo) 49:449–455
Gangemi M, Maiuri F, Colella G, Magro F, Seneca V, de Divitiis E (2007) Is endoscopic third ventriculostomy an internal shunt alone? Minim Invasive Neurosurg 50:47–50
Grand W, Leonardo J (2011) Endoscopic third ventriculostomy in adults: A technique for dealing with the neural (opaque) floor. J Neurosurg 114:446–453
Greebe P, Rinkel GJ (2007) Life expectancy after perimesencephalic subarachnoid hemorrhage. Stroke 38:1222–1224
Hailong F, Guangfu H, Haibin T, Hong P, Yong C, Weidong L, Dongdong Z (2008) Endoscopic third ventriculostomy in the management of communicating hydrocephalus: a preliminary study. J Neurosurg 109:923–930
Hoefnagel D, Dammers R, Ter Laak-Poort MP, Avezaat CJ (2008) Risk factors for infections related to external ventricular drainage. Acta Neurochir (Wien) 150:209–214
Ildan F, Tuna M, Erman T, Gocer AI, Cetinalp E (2002) Prognosis and prognostic factors in nonaneurysmal perimesencephalic hemorrhage: a follow-up study in 29 patients. Surg Neurol 57:160–166
Jafar JJ, Weiner HL (1993) Surgery for angiographically occult cerebral aneurysms. J Neurosurg 79:674–679
Kang DH, Park J, Lee SH, Park SH, Kim YS, Hamm IS (2009) Does non-perimesencephalic type non-aneurysmal subarachnoid hemorrhage have a benign prognosis? J Clin Neurosci 16:904–908
Kokkinis C, Vlychou M, Zavras GM, Hadjigeorgiou GM, Papadimitriou A, Fezoulidis IV (2008) The role of 3D-computed tomography angiography (3D-CTA) in investigation of spontaneous subarachnoid haemorrhage: comparison with digital subtraction angiography (DSA) and surgical findings. Br J Neurosurg 22:71–78
Lagares A, Gomez PA, Lobato RD, Alen JF, Alday R, Campollo J, Gonzalez P, de la Lama A, Palomino JC, Miranda P (2002) Idiopathic subarachnoid hemorrhage; comparison of different bleeding patterns and long-term outcome. Neurocirugia (Astur) 13:110–119
Liliequist B (1959) The subarachnoid cisterns. An anatomic and roentgenologic study. Acta Radiol Suppl 185:1–108
Martinez-Manas R, Ibanez G, Macho J, Gaston F, Ferrer E (2002) A study of 234 patients with subarachnoid hemorrhage of aneurysmic and cryptogenic origin. Neurocirugia (Astur) 13:181–195
Meier U, Zeilinger FS, Schonherr B (2000) Endoscopic ventriculostomy versus shunt operation in normal pressure hydrocephalus: diagnostics and indication. Acta Neurochir Suppl 76:563–566
Muller-Forell W, Welschehold S, Kohler J, Schicketanz KH (2002) Subarachnoid hemorrhage without aneurysm. Radiologe 42:871–879
Oertel JM, Mondorf Y, Baldauf J, Schroeder HW, Gaab MR (2009) Endoscopic third ventriculostomy for obstructive hydrocephalus due to intracranial hemorrhage with intraventricular extension. J Neurosurg 111:1119–1126
Oertel JM, Mondorf Y, Gaab MR (2009) Endoscopic third ventriculostomy in obstructive hydrocephalus due to giant basilar artery aneurysm. J Neurosurg 110:14–18
Park EH, Dombrowski S, Luciano M, Zurakowski D, Madsen JR (2010) Alterations of pulsation absorber characteristics in experimental hydrocephalus. J Neurosurg Pediatr 6:159–170
Park SQ, Kwon OK, Kim SH, Oh CW, Han MH (2009) Pre-mesencephalic subarachnoid hemorrhage: rupture of tiny aneurysms of the basilar artery perforator. Acta Neurochir (Wien) 151:1639–1646
Rammos S, Klopfenstein J, Augspurger L, Wang H, Wagenbach A, Poston J, Lanzino G (2008) Conversion of external ventricular drains to ventriculoperitoneal shunts after aneurysmal subarachnoid hemorrhage: effects of site and protein/red blood cell counts on shunt infection and malfunction. J Neurosurg 109:1001–1004
Rinkel GJ, Wijdicks EF, Hasan D, Kienstra GE, Franke CL, Hageman LM, Vermeulen M, van Gijn J (1991) Outcome in patients with subarachnoid haemorrhage and negative angiography according to pattern of haemorrhage on computed tomography. Lancet 338:964–968
Rinkel GJ, Wijdicks EF, Vermeulen M, Hasan D, Brouwers PJ, van Gijn J (1991) The clinical course of perimesencephalic nonaneurysmal subarachnoid hemorrhage. Ann Neurol 29:463–468
Rinkel GJ, Wijdicks EF, Vermeulen M, Tans JT, Hasan D, van Gijn J (1992) Acute hydrocephalus in nonaneurysmal perimesencephalic hemorrhage: evidence of CSF block at the tentorial hiatus. Neurology 42:1805–1807
Saliou G, Baledent O, Lehmann P, Paradot G, Gondry-Jouet C, Bouzerar R, Devisme G, Theaudin M, Deramond H, Le Gars D, Meyer ME, Vallee JN (2009) Acute CSF changes in the mesencephalon aqueduct after subarachnoid hemorrhage as measured by PC-MRI. J Neuroradiol 36:41–47
Schievink WI, Wijdicks EF (2000) Origin of pretruncal nonaneurysmal subarachnoid hemorrhage: ruptured vein, perforating artery, or intramural hematoma? Mayo Clin Proc 75:1169–1173
Schievink WI, Wijdicks EF, Piepgras DG, Nichols DA, Ebersold MJ (1994) Perimesencephalic subarachnoid hemorrhage. Additional perspectives from four cases. Stroke 25:1507–1511
Siomin V, Cinalli G, Grotenhuis A, Golash A, Oi S, Kothbauer K, Weiner H, Roth J, Beni-Adani L, Pierre-Kahn A, Takahashi Y, Mallucci C, Abbott R, Wisoff J, Constantini S (2002) Endoscopic third ventriculostomy in patients with cerebrospinal fluid infection and/or hemorrhage. J Neurosurg 97:519–524
Stachura K, Libionka W, Moskala M (2008) Neuroendoscopic third ventriculostomy in the management of noncommunicating hydrocephalus secondary to giant basilar artery bifurcation aneurysm—case report and review of literature. Neurol Neurochir Pol 42:255–262
Tatter SB, Crowell RM, Ogilvy CS (1995) Aneurysmal and microaneurysmal "angiogram-negative" subarachnoid hemorrhage. Neurosurgery 37:48–55
Whiting J, Reavey-Cantwell J, Velat G, Fautheree G, Firment C, Lewis S, Hoh B (2009) Clinical course of nontraumatic, nonaneurysmal subarachnoid hemorrhage: a single-institution experience. Neurosurg Focus 26:E21
Acknowledgements
The authors thank Paul H. Dressel, BFA, for preparation of the illustrations and Debra J. Zimmer, AAS CMA-A, for editorial assistance.
Funding of/support for this study
None
Conflicts of interest
None.
Disclosure
Aesculap has provided educational grants to support the annual brain endoscopy courses held in Buffalo, NY, for which Dr. Grand and Dr. Leonardo are the course director and co-director, respectively. Dr. Snyder has received research support from Toshiba. Dr. Chamczuk reports no relationships.
Author contributions to the study and manuscript preparation include the following:
Conception and design: Grand. Acquisition of data: Grand, Chamczuk, Leonardo. Analysis and interpretation of data: Grand, Leonardo, Snyder. Drafting the manuscript: Grand, Chamczuk. Critically revising the article: all authors. Reviewing the final version of the manuscript and approving it for submission: all authors. Study supervision: Grand.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The authors present a three case series with literature review of treating perimesencephalic non-aneurysmal subarachnoid hemorrhage-associated hydrocephalus with endoscopic third ventriculostomy (ETV).
Patients with non-aneurysmal perimesencephalic subarachnoid hemorrhage (NPMSAH) represent approximately 5% of subarachnoid hemorrhages. Although the development of hydrocephalus is uncommon, it is rare that permanent CSF diversion is required (i.e., VPS). The authors demonstrate the feasibility of performing an endoscopic third ventriculostomy to treat these patients. ETV is a well-accepted technique for treating obstructive hydrocephalus, commonly due to aqueductal stenosis. Intuitively, the role of ETV in treating communicating hydrocephalus is less obvious; however, it has been used successfully. The exact reason, as the authors allude to, is poorly understood.
The results cannot be disputed. The patients clearly had hydrocephalus, with elevated intracranial pressures. After failing to remove the EVD, the patients underwent an ETV. The ventricular size and intracranial pressures responded favorably, and the patients were spared the placement of a VPS. Although follow-up is short, ≈1 year, the patients have done well, and no evidence of hydrocephalus exists. It is of interest whether the ETV has remained patent. I commend the authors for their contribution.
Michael W. Weaver
Christopher M. Loftus
Philadelphia, PA
Financial relationships and/or potential conflicts of interest are as follows: Aesculap has provided educational grants to support the annual brain endoscopy courses held in Buffalo New York, for which Dr. Grand and Dr. Leonardo are the course director and co-director respectively. Dr. Snyder has received research support from Toshiba. Dr. Chamczuk has no financial relationships to disclose.
Previous presentation
Presented partially in abstract form at The Neurosurgical Society of America meeting at Pebble Beach, California, October 14, 2010
Rights and permissions
About this article
Cite this article
Grand, W., Chamczuk, A.J., Leonardo, J. et al. Endoscopic third ventriculostomy for hydrocephalus after perimesencephalic subarachnoid hemorrhage: initial experience in three patients. Acta Neurochir 153, 2049–2056 (2011). https://doi.org/10.1007/s00701-011-1106-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1106-2