Abstract
Background
Topical intra-articular tranexamic acid (IA-TXA) has been proven to be safe and effective in reducing postoperative blood loss after primary total knee arthroplasty (TKA). The objective of this study was to investigate the efficacy of high dose (3 g) compared with low dose (500 mg) of IA-TXA in postoperative blood loss after primary TKA.
Methods
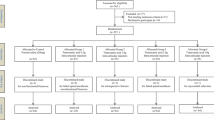
A double-blind randomized controlled trial was conducted in 80 patients who had undergone primary TKA. The patients were divided into two groups according to intra-articular TXA doses: high-dose group (3 g IA-TXA) and low-dose group (500 mg IA-TXA). The drug was injected into the joint capsule after fascial closure without suction drainage. The primary outcomes were maximum hemoglobin drop (g/dL) and calculated total blood loss (mL). Postoperative blood transfusions, thromboembolic events and functional outcomes were also recorded.
Results
The mean maximum hemoglobin drop was 1.3 g/dL lower in 3 g IA-TXA group compared to the 500 mg IA-TXA group [1.7 vs 3.0 g/dL, 95% confidence interval (CI) 0.9–1.7 g/dL, P < 0.001]. The 3 g IA-TXA group had 370 mL less calculated total blood loss compared to the 500 mg IA-TXA group (551 vs 921 mL, 95% CI 252–489 mL, P < 0.001). One patient in the 500 mg IA-TXA group required transfusion, while no patient in the 3 g IA-TXA group received transfusion (P = 0.31). Any thromboembolic event was not found, and functional outcome was similar between the two groups.
Conclusions
Application of high-dose, 3 g topical IA-TXA was 43% more effective in reducing postoperative blood loss compared with low dose of 500 mg in primary TKA. Optimal doses in between the above two doses may be a worthwhile further investigation.


Similar content being viewed by others
References
Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB (1999) An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am 81(1):2–10
Morais S, Ortega-Andreu M, Rodriguez-Merchan EC, Padilla-Eguiluz NG, Perez-Chrzanowska H, Figueredo-Zalve R, Gomez-Barrena E (2014) Blood transfusion after primary total knee arthroplasty can be significantly minimised through a multimodal blood-loss prevention approach. Int Orthop 38(2):347–354. https://doi.org/10.1007/s00264-013-2188-7
Tan J, Chen H, Liu Q, Chen C, Huang W (2013) A meta-analysis of the effectiveness and safety of using tranexamic acid in primary unilateral total knee arthroplasty. J Surg Res 184(2):880–887. https://doi.org/10.1016/j.jss.2013.03.099
Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM (2014) A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J 96-b(8):1005–1015. https://doi.org/10.1302/0301-620x.96b8.33745
Shin YS, Yoon JR, Lee HN, Park SH, Lee DH (2017) Intravenous versus topical tranexamic acid administration in primary total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 25(11):3585–3595. https://doi.org/10.1007/s00167-016-4235-6
Patel JN, Spanyer JM, Smith LS, Huang J, Yakkanti MR, Malkani AL (2014) Comparison of intravenous versus topical tranexamic acid in total knee arthroplasty: a prospective randomized study. J Arthroplasty 29(8):1528–1531. https://doi.org/10.1016/j.arth.2014.03.011
Wang H, Shen B, Zeng Y (2014) Comparison of topical versus intravenous tranexamic acid in primary total knee arthroplasty: a meta-analysis of randomized controlled and prospective cohort trials. Knee 21(6):987–993. https://doi.org/10.1016/j.knee.2014.09.010
Cao G, Huang Q, Huang Z, Zhang S, Luo Z, Lei Y, Zhou Z, Pei F (2018) The efficacy and safety of multiple-dose oral tranexamic acid on blood loss following total hip arthroplasty: a randomized controlled trial. Int Orthop. https://doi.org/10.1007/s00264-018-3925-8
Zhao H, Xiang M, Xia Y, Shi X, Pei FX, Kang P (2018) Efficacy of oral tranexamic acid on blood loss in primary total hip arthroplasty using a direct anterior approach: a prospective randomized controlled trial. Int Orthop. https://doi.org/10.1007/s00264-018-3846-6
Wong J, Abrishami A, El Beheiry H, Mahomed NN, Roderick Davey J, Gandhi R, Syed KA, Muhammad Ovais Hasan S, De Silva Y, Chung F (2010) Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am 92(15):2503–2513. https://doi.org/10.2106/jbjs.i.01518
Panteli M, Papakostidis C, Dahabreh Z, Giannoudis PV (2013) Topical tranexamic acid in total knee replacement: a systematic review and meta-analysis. Knee 20(5):300–309. https://doi.org/10.1016/j.knee.2013.05.014
Konig G, Hamlin BR, Waters JH (2013) Topical tranexamic acid reduces blood loss and transfusion rates in total hip and total knee arthroplasty. J Arthroplasty 28(9):1473–1476. https://doi.org/10.1016/j.arth.2013.06.011
Sa-Ngasoongsong P, Wongsak S, Chanplakorn P, Woratanarat P, Wechmongkolgorn S, Wibulpolprasert B, Mulpruek P, Kawinwonggowit V (2013) Efficacy of low-dose intra-articular tranexamic acid in total knee replacement; a prospective triple-blinded randomized controlled trial. BMC Musculoskelet Disord 14:340. https://doi.org/10.1186/1471-2474-14-340
Roy SP, Tanki UF, Dutta A, Jain SK, Nagi ON (2012) Efficacy of intra-articular tranexamic acid in blood loss reduction following primary unilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(12):2494–2501. https://doi.org/10.1007/s00167-012-1942-5
Aryal MR, Pandit A, Ghimire S, Pathak R, Karmacharya P, Poudel DR, Shamoun FE (2015) Thromboprophylaxis with apixaban and the risk of pulmonary embolism in patients undergoing knee replacement surgery. J Community Hosp Intern Med Perspect 5(4):27889. https://doi.org/10.3402/jchimp.v5.27889
American Society of Anesthesiologists Task Force on Perioperative Blood T, Adjuvant T (2006) Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology 105(1):198–208
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224–232
Good L, Peterson E, Lisander B (2003) Tranexamic acid decreases external blood loss but not hidden blood loss in total knee replacement. Br J Anaesth 90(5):596–599
Gao FQ, Li ZJ, Zhang K, Sun W, Zhang H (2015) Four Methods for Calculating Blood-loss after Total Knee Arthroplasty. Chin Med J (Engl) 128(21):2856–2860. https://doi.org/10.4103/0366-6999.168041
Kuptniratsaikul V, Rattanachaiyanont M (2007) Validation of a modified Thai version of the Western Ontario and McMaster (WOMAC) osteoarthritis index for knee osteoarthritis. Clin Rheumatol 26(10):1641–1645. https://doi.org/10.1007/s10067-007-0560-y
Wang S, Gao X, An Y (2017) Topical versus intravenous tranexamic acid in total knee arthroplasty: a meta-analysis of randomized controlled trials. Int Orthop 41(4):739–748. https://doi.org/10.1007/s00264-016-3296-y
Lei Y, Xie J, Xu B, Xie X, Huang Q, Pei F (2017) The efficacy and safety of multiple-dose intravenous tranexamic acid on blood loss following total knee arthroplasty: a randomized controlled trial. Int Orthop 41(10):2053–2059. https://doi.org/10.1007/s00264-017-3519-x
Zeng Y, Si H, Li C, Wu Y, Shen B (2018) Effect of knee flexion position and combined application of tranexamic acid on blood loss following primary total knee arthroplasty: a prospective randomized controlled trial. Int Orthop 42(3):529–535. https://doi.org/10.1007/s00264-018-3808-z
Prakash J, Seon JK, Park YJ, Jin C, Song EK (2017) A randomized control trial to evaluate the effectiveness of intravenous, intra-articular and topical wash regimes of tranexamic acid in primary total knee arthroplasty. J Orthop Surg (Hong Kong) 25(1):2309499017693529. https://doi.org/10.1177/2309499017693529
Sarzaeem MM, Razi M, Kazemian G, Moghaddam ME, Rasi AM, Karimi M (2014) Comparing efficacy of three methods of tranexamic acid administration in reducing hemoglobin drop following total knee arthroplasty. J Arthroplasty 29(8):1521–1524. https://doi.org/10.1016/j.arth.2014.02.031
Serrano Mateo L, Goudarz Mehdikhani K, Caceres L, Lee YY, Gonzalez Della Valle A (2016) Topical tranexamic acid may improve early functional outcomes of primary total knee arthroplasty. J Arthroplasty 31(7):1449–1452. https://doi.org/10.1016/j.arth.2016.01.009
Grosso MJ, Trofa DP, Danoff JR, Hickernell TR, Murtaugh T, Lakra A, Geller JA (2018) Tranexamic acid increases early perioperative functional outcomes after total knee arthroplasty. Arthroplasty Today 4(1):74–77. https://doi.org/10.1016/j.artd.2017.05.009
Rong GX, Shen CL, Gui BJ, Yin H, Tang Z (2017) Comparison of tranexamic acid pharmacokinetics after intra-articular and intravenous administration in rabbits. Pak J Pharm Sci 30(4):1309–1316
Fillingham YA, Ramkumar DB, Jevsevar DS, Yates AJ, Shores P, Mullen K, Bini SA, Clarke HD, Schemitsch E, Johnson RL, Memtsoudis SG, Sayeed SA, Sah AP, Della Valle CJ (2018) The safety of tranexamic acid in total joint arthroplasty: a direct meta-analysis. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.03.031
Acknowledgements
We thank professor Norman Hangnail for reviewing the article and language help. We also thank all participants for providing the data used in this study.
Funding
This study was funded by Thammasat University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest. All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tammachote, N., Raphiphan, R. & Kanitnate, S. High-dose (3 g) topical tranexamic acid has higher potency in reducing blood loss after total knee arthroplasty compared with low dose (500 mg): a double‐blind randomized controlled trial. Eur J Orthop Surg Traumatol 29, 1729–1735 (2019). https://doi.org/10.1007/s00590-019-02515-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02515-2