Abstract
Objective
To raise the diagnostic criteria, classification and treatment strategy of dynamic sagittal imbalance (DSI).
Methods
One hundred thirty-three adult spinal deformity (ASD) patients with stooping and back pain after walking were retrospectively analyzed. Based on the radiographic parameters and Oswestry Disability Index (ODI) scores, the diagnostic criteria of DSI were raised. DSI patients received nonoperative treatment and (or) surgery. Radiographic parameters and health-related quality of life (HRQOL) outcomes would be measured and compared between prewalk and postwalk and among each subgroup.
Results
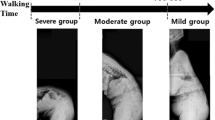
One hundred thirty-three ASD patients with stooping and back pain after walking were enrolled in our study. The quantitative diagnostic criteria was prewalk SVA < 40 mm and postwalk SVA-prewalk SVA ≥ 20 mm after 10-min walk. Based on the quantitative diagnostic criteria of DSI raised by our team, DSI patients could be classified into three groups: 20 mm ≤ ΔSVA < 60 mm (mild, 31.0%), 60 mm ≤ ΔSVA < 100 mm (moderate, 42.1%) and ΔSVA ≥ 100 mm (severe, 27.0%). After nonoperative treatment, the ΔSVA in mild and moderate group was prominently decreased (P < 0.001) with the significant improvement of HRQOL outcomes (P < 0.001), while there was no significant change in ΔSVA and clinical outcomes in group C (P > 0.05). Patients who received the operative treatment showed prominent improvement in ΔSVA and clinical outcomes (P < 0.001).
Conclusion
Our study proposed a quantitative diagnostic criteria and novel classification of DSI. Nonoperative treatment is effective for most DSI patients with ΔSVA < 100 mm, while the majority of DSI patients with ΔSVA ≥ 100 mm need operative intervention.








Similar content being viewed by others
References
Bailey JF, Matthew RP, Seko S, Curran P, Chu L, Berven SH, Deviren V, Burch S, Lotz JC (2019) ISSLS PRIZE IN BIOENGINEERING SCIENCE 2019: biomechanical changes in dynamic sagittal balance and lower limb compensatory strategies following realignment surgery in adult spinal deformity patients. Eur Spine J 28:905–913. https://doi.org/10.1007/s00586-019-05925-2
Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, Schwab FJ, Lafage V (2019) Adult spinal deformity. Lancet 394:160–172. https://doi.org/10.1016/S0140-6736(19)31125-0
Youssef JA, Orndorff DO, Patty CA, Scott MA, Price HL, Hamlin LF, Williams TL, Uribe JS, Deviren V (2013) Current status of adult spinal deformity. Global Spine J 3:51–62. https://doi.org/10.1055/s-0032-1326950
Ploumis A, Simpson AK, Cha TD, Herzog JP, Wood KB (2015) Coronal spinal balance in adult spine deformity patients with long spinal fusions: a minimum 2- to 5-year follow-up study. J Spinal Disord Tech 28:341–347. https://doi.org/10.1097/BSD.0b013e3182aab2ff
Ailon T, Smith JS, Shaffrey CI, Lenke LG, Brodke D, Harrop JS, Fehlings M, Ames CP (2015) Degenerative spinal deformity. Neurosurgery 77(Suppl 4):S75–91. https://doi.org/10.1227/NEU.0000000000000938
Angevine PD, Bray D, Cloney M, Malone H (2019) Uncertainty in the relationship between sagittal alignment and patient-reported outcomes. Neurosurgery. https://doi.org/10.1093/neuros/nyz228
McDowell MM, Tempel ZJ, Gandhoke GS, Khattar NK, Hamilton DK, Kanter AS, Okonkwo DO (2017) Evolution of sagittal imbalance following corrective surgery for sagittal plane deformity. Neurosurgery 81:129–134. https://doi.org/10.1093/neuros/nyx145
Katsu M, Ohba T, Ebata S, Oba H, Koyama K, Haro H (2019) Potential role of paraspinal musculature in the maintenance of spinopelvic alignment in patients with adult spinal deformities. Clin Spine Surg. https://doi.org/10.1097/BSD.0000000000000862
Yagi M, Hosogane N, Watanabe K, Asazuma T, Matsumoto M, Keio Spine Research G (2016) The paravertebral muscle and psoas for the maintenance of global spinal alignment in patient with degenerative lumbar scoliosis. Spine J 16:451–458. https://doi.org/10.1016/j.spinee.2015.07.001
Bess S, Schwab F, Lafage V, Shaffrey CI, Ames CP (2013) Classifications for adult spinal deformity and use of the Scoliosis Research Society-Schwab Adult Spinal Deformity Classification. Neurosurg Clin N Am 24:185–193. https://doi.org/10.1016/j.nec.2012.12.008
Shiba Y, Taneichi H, Inami S, Moridaira H, Takeuchi D, Nohara Y (2016) Dynamic global sagittal alignment evaluated by three-dimensional gait analysis in patients with degenerative lumbar kyphoscoliosis. Eur Spine J 25:2572–2579. https://doi.org/10.1007/s00586-016-4648-4
Lee CS, Lee CK, Kim YT, Hong YM, Yoo JH (2001) Dynamic sagittal imbalance of the spine in degenerative flat back: significance of pelvic tilt in surgical treatment. Spine (Phila Pa 1976) 26:2029–2035. https://doi.org/10.1097/00007632-200109150-00017
Bae J, Theologis AA, Jang JS, Lee SH, Deviren V (2017) Impact of fatigue on maintenance of upright posture: dynamic assessment of sagittal spinal deformity parameters after walking 10 minutes. Spine (Phila Pa 1976) 42:733–739. https://doi.org/10.1097/BRS.0000000000001898
Smith JS, Lafage V, Shaffrey CI, Schwab F, Lafage R, Hostin R, O'Brien M, Boachie-Adjei O, Akbarnia BA, Mundis GM, Errico T, Kim HJ, Protopsaltis TS, Hamilton DK, Scheer JK, Sciubba D, Ailon T, Fu KM, Kelly MP, Zebala L, Line B, Klineberg E, Gupta M, Deviren V, Hart R, Burton D, Bess S, Ames CP, International Spine Study G (2016) Outcomes of operative and nonoperative treatment for adult spinal deformity: a prospective, multicenter, propensity-matched cohort assessment with minimum 2-year follow-up. Neurosurgery 78:851–861. https://doi.org/10.1227/NEU.0000000000001116
Arima H, Yamato Y, Hasegawa T, Kobayashi S, Yoshida G, Yasuda T, Banno T, Oe S, Mihara Y, Togawa D, Matsuyama Y (2017) Extensive corrective fixation surgeries for adult spinal deformity improve posture and lower extremity kinematics during gait. Spine (Phila Pa 1976) 42:1456–1463
Engsberg JR, Bridwell KH, Wagner JM, Uhrich ML, Blanke K, Lenke LG (2003) Gait changes as the result of deformity reconstruction surgery in a group of adults with lumbar scoliosis. Spine (Phila Pa 1976) 28:1836–1843. https://doi.org/10.1097/00007632-200308150-00012 (discussion 1844)
Slobodyanyuk K, Poorman CE, Smith JS, Protopsaltis TS, Hostin R, Bess S, Mundis GM, Jr., Schwab FJ, Lafage V, International Spine Study G (2014) Clinical improvement through nonoperative treatment of adult spinal deformity: who is likely to benefit? Neurosurg Focus 36:E2. https://doi.org/10.3171/2014.3.FOCUS1426
Acaroglu E, Yavuz AC, Guler UO, Yuksel S, Yavuz Y, Domingo-Sabat M, Pellise F, Alanay A, Perez Grueso FS, Kleinstuck F, Obeid I, European Spine Study G (2016) A decision analysis to identify the ideal treatment for adult spinal deformity: is surgery better than non-surgical treatment in improving health-related quality of life and decreasing the disease burden? Eur Spine J 25:2390–2400. https://doi.org/10.1007/s00586-016-4413-8
Tonosu J, Takeshita K, Hara N, Matsudaira K, Kato S, Masuda K, Chikuda H (2012) The normative score and the cut-off value of the oswestry disability index (ODI). Eur Spine J 21:1596–1602. https://doi.org/10.1007/s00586-012-2173-7
Moal B, Lafage V, Smith JS, Ames CP, Mundis G, Terran JS, Klineberg E, Hart R, Boachie-Adjei O, Bess S, Skalli W, Schwab F, International Spine Study G (2015) Clinical improvement through surgery for adult spinal deformity: what can be expected and who is likely to benefit most? Spine Deform 3:566–574. https://doi.org/10.1016/j.jspd.2015.04.004
Parker SL, Mendenhall SK, Shau D, Adogwa O, Cheng JS, Anderson WN, Devin CJ, McGirt MJ (2012) Determination of minimum clinically important difference in pain, disability, and quality of life after extension of fusion for adjacent-segment disease. J Neurosurg Spine 16:61–67. https://doi.org/10.3171/2011.8.SPINE1194
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 34:E599–606. https://doi.org/10.1097/BRS.0b013e3181aad219
Schwab F, Farcy JP, Bridwell K, Berven S, Glassman S, Harrast J, Horton W (2006) A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976) 31:2109–2114. https://doi.org/10.1097/01.brs.0000231725.38943.ab
Schwab F, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35:2224–2231. https://doi.org/10.1097/BRS.0b013e3181ee6bd4
Barrey C, Roussouly P, Le Huec JC, D'Acunzi G, Perrin G (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22(Suppl 6):S834–841. https://doi.org/10.1007/s00586-013-3030-z
Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V (2015) Sagittal alignment of the spine: What do you need to know? Clin Neurol Neurosurg 139:295–301. https://doi.org/10.1016/j.clineuro.2015.10.024
Shahidi B, Parra CL, Berry DB, Hubbard JC, Gombatto S, Zlomislic V, Allen RT, Hughes-Austin J, Garfin S, Ward SR (2017) Contribution of lumbar spine pathology and age to paraspinal muscle size and fatty infiltration. Spine (Phila Pa 1976) 42:616–623. https://doi.org/10.1097/BRS.0000000000001848
Banno T, Yamato Y, Hasegawa T, Kobayashi S, Togawa D, Oe S, Mihara Y, Kurosu K, Yamamoto N, Matsuyama Y (2017) Assessment of the cross-sectional areas of the psoas major and multifidus muscles in patients with adult spinal deformity: a case-control study. Clin Spine Surg 30:E968–E973. https://doi.org/10.1097/BSD.0000000000000480
Jun HS, Kim JH, Ahn JH, Chang IB, Song JH, Kim TH, Park MS, Chan Kim Y, Kim SW, Oh JK, Yoon DH (2016) The effect of lumbar spinal muscle on spinal sagittal alignment: evaluating muscle quantity and quality. Neurosurgery 79:847–855. https://doi.org/10.1227/NEU.0000000000001269
Banno T, Arima H, Hasegawa T, Yamato Y, Togawa D, Yoshida G, Yasuda T, Oe S, Mihara Y, Ushirozako H, Matsuyama Y (2019) The effect of paravertebral muscle on the maintenance of upright posture in patients with adult spinal deformity. Spine Deform 7:125–131. https://doi.org/10.1016/j.jspd.2018.06.008
Shafaq N, Suzuki A, Matsumura A, Terai H, Toyoda H, Yasuda H, Ibrahim M, Nakamura H (2012) Asymmetric degeneration of paravertebral muscles in patients with degenerative lumbar scoliosis. Spine (Phila Pa 1976) 37:1398–1406. https://doi.org/10.1097/BRS.0b013e31824c767e
Yagi M, Kaneko S, Yato Y, Asazuma T, Machida M (2016) Walking sagittal balance correction by pedicle subtraction osteotomy in adults with fixed sagittal imbalance. Eur Spine J 25:2488–2496. https://doi.org/10.1007/s00586-016-4604-3
Funding
This research has not received any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declared that they have no potential conflict of interest.
Ethical approval
The research project was approved by the ethics department of Shanghai Changzheng Hospital, Shanghai. We have consensus with all participants. All the procedures were done under the Declaration of Helsinki and relevant policies in China. The Manuscript submitted does not contain information about medical device(s)/drug(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yin, J., Ma, X., Lin, T. et al. Characteristics and treatment of dynamic sagittal imbalance in adult spinal deformity. Eur Spine J 29, 2340–2353 (2020). https://doi.org/10.1007/s00586-020-06459-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06459-8