Abstract
Purpose
Postoperative bracing treatment is widely used after surgery for lumbar degenerative diseases. However, the guidelines are lacking in this regard, and its use is mainly driven by individual surgeon preferences. The objective of the current review was to evaluate the available evidence on the use of postoperative bracing after surgery for degenerative disease of the lumbar spine.
Methods
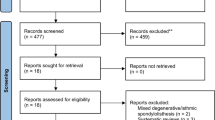
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were followed while conducting a systematic search of the PubMed/Medline, Scopus, and Cochrane databases from January 1990 to January 2019. High-quality studies were included that evaluated disability, pain, quality of life, the rate of fusion, complications, and rate of reoperations in patients who had surgery for lumbar degenerative disease, with and without postoperative bracing. The overall strength of evidence across the studies was assessed using the Grading of Recommendations Assessment, Development, and Evaluation framework.
Results
Of the 391 citations screened, four randomized controlled trials met the inclusion criteria and were included in the review. Based on low- to moderate-quality evidence, postoperative bracing in patients with lumbar degenerative disease does not result in improved disability, pain, and quality of life compared to no bracing patients. Low-quality evidence suggests that there was no significant difference between the two groups in terms of the rate of fusion, complications, and the need for reoperation.
Conclusions
To date, there is not a medical evidence to support the use of bracing after surgery for lumbar degenerative disease.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.


Similar content being viewed by others
References
Yee AJ, Yoo JU, Marsolais EB et al (2008) Use of a postoperative lumbar corset after lumbar spinal arthrodesis for degenerative conditions of the spine: a prospective randomized trial. J Bone Joint Surg Am 90(10):2062–2068
Soliman HA, Barchi S, Parent S et al (2017) The early impact of postoperative bracing on pain and quality of life following posterior instrumented fusion for lumbar degenerative conditions: a randomized trial. Spine 43(3):155–160
Yao YC, Lin HH, Chang MC (2018) Bracing following transforaminal lumbar interbody fusion is not necessary for patients with degenerative lumbar spine disease: a prospective, randomized trial. Clin Spine Surg 1(9):E441–E445
Zoia C, Bongetta D, Alicino C, Chimenti M, Pugliese R, Gaetani P (2018) Usefulness of corset adoption after single-level lumbar discectomy: a randomized controlled trial. J Neurosurg Spine 28(5):481–485
Bible JE, Biswas D, Whang PG, Simpson AK, Rechtine GR, Grauer JN (2009) Postoperative bracing after spine surgery for degenerative conditions: a questionnaire study. Spine J 9(4):309–316
Bogaert L, Van Wambeke P, Thys T et al (2019) Postoperative bracing after lumbar surgery: a survey amongst spinal surgeons in Belgium. Eur Spine J 28(2):442–449
Dailey AT, Ghogawala Z, Choudhri TF et al (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 14: brace therapy as an adjunct to or substitute for lumbar fusion. J Neurosurg Spine 21(1):91–101
Zhu MP, Tetreault LA, Sorefan-Mangou F, Garwood P, Wilson JR (2018) Efficacy, safety, and economics of bracing after spine surgery: a systematic review of the literature. Spine J 18(9):1513–1525
Johnsson R, Strömqvist B, Axelsson P, Selvik G (1992) Influence of spinal immobilization on consolidation of posterolateral lumbosacral fusion: a roentgen stereophotogrammetric and radiographic analysis. Spine 17:16–21
Axelsson P, Johnsson R, Strömqvist B (1992) Effect of lumbar orthosis on intervertebral mobility: a roentgen stereophotogrammetric analysis. Spine 17:678–681
Axelsson P, Johnsson R, Strömqvist B (1993) Lumbar orthosis with unilateral hip immobilization: effect on intervertebral mobility determined by roentgen stereophotogrammetric analysis. Spine 18:876–879
Rohlmann A, Bergmann G, Graichen F, Neff G (1999) Braces do not reduce loads on internal spinal fixation devices. Clin Biomech 14:97–102
North American Spine Society website. Clinical guidelines. Available from: https://www.spine.org/ResearchClinicalCare/QualityImprovement/ClinicalGuidelines. Accessed 16th April 2018
Guyatt G, Oxman AD, Akl EA et al (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–394
Archer KR, Wegener ST, Seebach C et al (2011) The effect of fear of movement beliefs on pain and disability after surgery for lumbar and cervical degenerative conditions. Spine 36:1554–1562
Madera M, Brady J, Deily S et al (2017) The role of physical therapy and rehabilitation after lumbar fusion surgery for degenerative disease: a systematic review. J Neurosurg Spine 26:694–704
Dobran M, Marini A, Nasi D et al (2017) Risk factors of surgical site infections in instrumented spine surgery. Surg Neurol Int 8:212
Dobran M, Marini A, Gladi M et al (2017) Deep spinal infection in instrumented spinal surgery: diagnostic factors and therapy. G Chir 38:124–129
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nasi, D., Dobran, M. & Pavesi, G. The efficacy of postoperative bracing after spine surgery for lumbar degenerative diseases: a systematic review. Eur Spine J 29, 321–331 (2020). https://doi.org/10.1007/s00586-019-06202-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06202-y