Abstract
Purpose
The purpose of this study was to elucidate whether lung-protective ventilation-induced respiratory acidosis increased the duration of neuromuscular blockade by rocuronium.
Methods
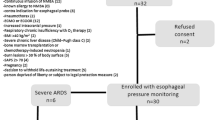
A total of 72 patients were enrolled. After the induction of general anesthesia, rocuronium 0.6 mg/kg real body weight was administered. Tidal volume and positive end-expiratory pressure were randomly assigned as either 10 ml/kg predicted body weight and 0 cmH2O (group S) or 6 ml/kg and 5 cmH2O (group L), respectively. Respiratory rate was started at 10/min. Neuromuscular blockade was monitored by acceleromyography at the adductor pollicis with train-of-four stimulation. The time from the initial bolus injection of rocuronium to first recovery of the first twitch was defined as DUR1. Immediately, rocuronium 0.15 mg/kg was administered. The time from first recovery of the first twitch to second recovery of the first twitch was defined as DUR2. We also measured arterial pH (pH1 and pH2, respectively).
Results
Data from 66 patients (33 each in groups L and S) were eventually available. pH1 and pH2 were significantly lower in group L compared with group S [pH1: 7.308 (7.288–7.334) vs. 7.439 (7.423–7.466); p < 0.01, pH2: 7.306 (7.285–7.330) vs. 7.453 (7.436–7.476); p < 0.01]. DUR1 and DUR2 were significantly prolonged in group L compared with group S [DUR1: 31 (24–36) vs. 24 (20–30) min; p = 0.029, DUR2: 19 (15–22) vs. 15 (12–17) min; p = 0.020].
Conclusions
Lung-protective ventilation-induced respiratory acidosis increased the duration of neuromuscular blockade by rocuronium.



Similar content being viewed by others
References
Aziz L, Ono K, Ohta Y, Morita K, Hirakawa M. The effect of CO2-induced acid-base changes on the potencies of muscle relaxants and antagonism of neuromuscular block by neostigmine in rat in vitro. Anesth Analg. 1994;78:322–7.
Severgnini P, Selmo G, Lanza C, Chiesa A, Frigerio A, Bacuzzi A, Dionigi G, Novario R, Gregoretti C, de Abreu MG, Schultz MJ, Jaber S, Futier E, Chiaranda M, Pelosi P. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;118:1307–21.
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37.
Leykin Y, Pellis T, Lucca M, Lomangino G, Marzano B, Gullo A. The pharmacodynamic effects of rocuronium when dosed according to real body weight or ideal body weight in morbidly obese patients. Anesth Analg. 2004;99:1086–9.
The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8.
Ito S, Nagata O, Ozaki M. Estimated blood concentration of rocuronium administrated by continuous infusion to maintain an appropriate neuromuscular blockade under propofol anesthesia (in Japanese with English abstract). Masui (Jpn J Anesthesiol). 2010;59:82–6.
Altman DG. Statistics and ethics in medical research: III How large a sample? Br Med J. 1980;281:1336–8.
Ono K, Ohta Y, Morita K, Kosaka F. The influence of respiratory-induced acid-base changes on the action of non-depolarizing muscle relaxants in rats. Anesthesiology. 1988;68:357–62.
Ono K, Nagano O, Ohta Y, Kosaka F. Neuromuscular effects of respiratory and metabolic acid-base changes in vitro with and without nondepolarizing muscle relaxants. Anesthesiology. 1990;73:710–6.
Adamus M, Gabrhelik T, Marek O. Influence of gender on the course of neuromuscular block following a single bolus dose of cisatracurium or rocuronium. Eur J Anaesthesiol. 2008;25:589–95.
Matteo RS, Ornstein E, Schwartz AE, Ostapkovich N, Stone JG. Pharmacokinetics and pharmacodynamics of rocuronium (Org 9426) in elderly surgical patients. Anesth Analg. 1993;77:1193–7.
Aziz L, Ono K, Ohta Y, Morita K, Hirakawa M. Effect of hypothermia on the in vitro potencies of neuromuscular blocking agents and on their antagonism by neostigmine. Br J Anaesth. 1994;73:662–6.
Smeulers NJ, Wierda JM, van den Broek L, Gallandat Huet RC, Hennis PJ. Hypothermic cardiopulmonary bypass influences the concentration-response relationship and the biodisposition of rocuronium. Eur J Anaesthesiol. 1995;12(Suppl 11):91–4.
Wulf H, Ledowski T, Linstedt U, Proppe D, Sitzlack D. Neuromuscular blocking effects of rocuronium during desflurane, isoflurane, and sevoflurane anaesthesia. Can J Anaesth. 1998;45:526–32.
Wang T, Huang S, Geng G. Comparison of the duration of neuromuscular blockade following a single bolus dose of rocuronium during laparoscopic gynaecological surgery vs conventional open surgery. Anaesthesia. 2014;69:854–9.
Acknowledgments
We thank Keita Hazama (Kawasaki Medical School) for technical advice and Toshifumi Shoho, Minori Noda, and Shoichiro Hirata (Fukuyama City Hospital) for technical assistance.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Taguchi, S., Ono, K., Hidaka, H. et al. Effect of lung-protective ventilation-induced respiratory acidosis on the duration of neuromuscular blockade by rocuronium. J Anesth 30, 994–998 (2016). https://doi.org/10.1007/s00540-016-2235-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2235-9