Abstract
Purpose
Fatigue has found increasing attention as a debilitating and lasting condition of cancer patients. However, it has remained unclear to what degree long-term survivors of malignant melanoma suffer from fatigue. Therefore, this study aimed to determine fatigue and its link with quality of life, aftercare behavior, and mental and physical symptoms among melanoma survivors.
Methods
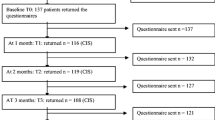
A register-based sample of 684 long-term survivors an average of 8.4 (SD = 1.72; range 5.67–12.17) years after diagnosis was compared to 2049 participants from a representative survey by the Multidimensional Fatigue Inventory. In a hierarchical linear regression, statistical predictors for fatigue were ascertained.
Results
Overall fatigue was not increased in melanoma survivors except for younger melanoma survivors under 40 years. As in the general population, fatigue increased with age, and it was higher in women compared to men. Fatigue was associated with decreased quality of life, reduced functioning, and increased physical and mental symptoms. Substantial predictors (30% explained variance) were higher age, additional chronic illness, self-blame, detrimental interactions and lack of social support, and also fear of recurrence. There was neither an effect of medical parameters (clinical stage, time since diagnosis) nor of participation in follow-up care.
Conclusions
Fatigue needs to be taken seriously in the aftercare of melanoma survivors as it is associated with multiple functional and quality of life impairments and heightened distress. Reduction of fatigue in melanoma patients should address younger survivors (under 40 years) and older survivors (over 60 years) with additional chronic illness and focus on illness coping and social support.

Similar content being viewed by others
References
Simard EP, Ward EM, Siegel R, Jemal A (2012) Cancers with increasing incidence trends in the United States: 1999 through 2008. CA Cancer J Clin 62(2):118–128. https://doi.org/10.3322/caac.20141
Loquai C, Scheurich V, Syring N, Schmidtmann I, Rietz S, Werner A, Grabbe S, Beutel ME (2013) Screening for distress in routine oncological care-a survey in 520 melanoma patients. PLoS One 8(7):e66800. https://doi.org/10.1371/journal.pone.0066800
McLoone J, Watts K, Menzies S, Meiser B, Butow P, Kasparian N (2012) When the risks are high: psychological adjustment among melanoma survivors at high risk of developing new primary disease. Qual Health Res 22(8):1102–1113. https://doi.org/10.1177/1049732312448542
Beutel ME, Fischbeck S, Binder H, Blettner M, Brahler E, Emrich K, Friedrich-Mai P, Imruck BH, Weyer V, Zeissig SR (2015) Depression, anxiety and quality of life in long-term survivors of malignant melanoma: a register-based cohort study. PLoS One 10(1):e0116440. https://doi.org/10.1371/journal.pone.0116440
Kocalevent RD, Hinz A, Brahler E, Klapp BF (2011) Determinants of fatigue and stress. BMC Res Notes 4:238. https://doi.org/10.1186/1756-0500-4-238
World Health Organization (2001) International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland
Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol 52:397–422. https://doi.org/10.1146/annurev.psych.52.1.397
Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, Cleeland C, Dotan E, Eisenberger MA, Escalante CP, Jacobsen PB, Jankowski C, LeBlanc T, Ligibel JA, Loggers ET, Mandrell B, Murphy BA, Palesh O, Pirl WF, Plaxe SC, Riba MB, Rugo HS, Salvador C, Wagner LI, Wagner-Johnston ND, Zachariah FJ, Bergman MA, Smith C (2015) Cancer-related fatigue, version 2.2015. J Natl Compr Cancer Netw 13(8):1012–1039. https://doi.org/10.6004/jnccn.2015.0122
Fiorentino L, Rissling M, Liu L, Ancoli-Israel S (2011) The symptom cluster of sleep, fatigue and depressive symptoms in breast cancer patients: severity of the problem and treatment options. Drug Discov Today Dis Model 8(4):167–173. https://doi.org/10.1016/j.ddmod.2011.05.001
Dimsdale JE, Dantzer R (2007) A biological substrate for somatoform disorders: importance of pathophysiology. Psychosom Med 69(9):850–854. https://doi.org/10.1097/PSY.0b013e31815b00e7
Spruit MA, Vercoulen JH, Sprangers MAG, Wouters EFM (2017) Fatigue in COPD: an important yet ignored symptom. Lancet Respir Med 5(7):542–544. https://doi.org/10.1016/s2213-2600(17)30158-3
Beutel ME, Hinz A, Albani C, Brahler E (2006) Fatigue assessment questionnaire: standardization of a cancer-specific instrument based on the general population. Oncology 70(5):351–357. https://doi.org/10.1159/000098108
Weis J, Tomaszewski KA, Hammerlid E, Ignacio Arraras J, Conroy T, Lanceley A, Schmidt H, Wirtz M, Singer S, Pinto M, Alm El-Din M, Compter I, Holzner B, Hofmeister D, Chie WC, Czeladzki M, Harle A, Jones L, Ritter S, Flechtner HH, Bottomley A, Group EQoL (2017) International Psychometric Validation of an EORTC Quality of Life Module Measuring Cancer Related Fatigue (EORTC QLQ-FA12). J Natl Cancer Inst 109(5). https://doi.org/10.1093/jnci/djw273
Johnson JA, Garland SN, Carlson LE, Savard J, Simpson JS, Ancoli-Israel S, Campbell TS (2016) The LITE study: rationale and protocol for a randomized controlled trial of light therapy for cancer-related fatigue in cancer survivors. Contemp Clin Trials 49:166–173. https://doi.org/10.1016/j.cct.2016.07.004
Kuhnt S, Szalai C, Erdmann-Reusch B, Kubel C, Boehncke A, Hoffmann W, Mehnert A, Weis J (2017) Cancer related fatigue in rehabilitation care. Rehabilitation (Stuttg) 56(5):337–343. https://doi.org/10.1055/s-0043-101142
Glaus A, Müller S (2001) Messung der Müdigkeit bei Krebskranken im Deutschen Sprachraum: Die Entwicklung des Fatigue Assessment Questionnaires. Pflege 14:161–170
Mehnert A, Hartung TJ, Friedrich M, Vehling S, Brahler E, Harter M, Keller M, Schulz H, Wegscheider K, Weis J, Koch U, Faller H (2018) One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psycho-Oncology 27(1):75–82. https://doi.org/10.1002/pon.4464
Given B, Given CW, McCorkle R, Kozachik S, Cimprich B, Rahbar MH, Wojcik C (2002) Pain and fatigue management: results of a nursing randomized clinical trial. Oncol Nurs Forum 29(6):949–956. https://doi.org/10.1188/02.ONF.949-956
Bennett B, Goldstein D, Friedlander M, Hickie I, Lloyd A (2007) The experience of cancer-related fatigue and chronic fatigue syndrome: a qualitative and comparative study. J Pain Symptom Manag 34(2):126–135. https://doi.org/10.1016/j.jpainsymman.2006.10.014
Jones JM, Olson K, Catton P, Catton CN, Fleshner NE, Krzyzanowska MK, McCready DR, Wong RK, Jiang H, Howell D (2016) Cancer-related fatigue and associated disability in post-treatment cancer survivors. J Cancer Surviv 10(1):51–61. https://doi.org/10.1007/s11764-015-0450-2
Bower JE (2014) Cancer-related fatigue--mechanisms, risk factors, and treatments. Nat Rev Clin Oncol 11(10):597–609. https://doi.org/10.1038/nrclinonc.2014.127
Nashan D, Reuter K, Mohr P, Agarwala SS (2012) Understanding and managing interferon-alpha-related fatigue in patients with melanoma. Melanoma Res 22(6):415–423. https://doi.org/10.1097/CMR.0b013e328358d98c
Kuhnt S, Ehrensperger C, Singer S, Hofmeister D, Papsdorf K, Weis J, Zwerenz R, Brähler E (2011) Prädiktoren tumorassoziierter Fatigue. Psychotherapeut 56(3):216–223. https://doi.org/10.1007/s00278-011-0822-7
Smets EMA, Garssen B, Bonke B, De Haes JCJM (1995) The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res 39(3):315–325. https://doi.org/10.1016/0022-3999(94)00125-o
Smets EMA, Garssen B, Cull A, de Haes J (1996) Application of the multidimensional fatigue inventory (MFI-20) in cancer patients receiving radiotherapy. Br J Cancer 73(2):241–245. https://doi.org/10.1038/bjc.1996.42
Zeissig SR, Weyer-Elberich V, Emrich K, Binder H, Fischbeck S, Imruck BH, Friedrich-Mai P, Beutel ME, Blettner M (2017) Recruiting former melanoma patients via hospitals in comparison to office-based dermatologists in a register-based cohort study that required indirect contact. BMC Med Res Methodol 17(1):150. https://doi.org/10.1186/s12874-017-0425-2
Schwarz R, Krauss O, Hinz A (2003) Fatigue in the general population. Onkologie 26(2):140–144. https://doi.org/10.1159/000069834
Cronbach LJ (1951) Coefficient alpha and the internal structure of tests. Psychometrika 16(3):297–334. https://doi.org/10.1007/bf02310555
Kocalevent R-D, Hinz A, Brähler E (2013) Standardization of a screening instrument (PHQ-15) for somatization syndromes in the general population. BMC Psychiatry 13:91. https://doi.org/10.1186/1471-244x-13-91
Löwe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, Herzberg PY (2008) Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care 46(3):266–274. https://doi.org/10.1097/MLR.0b013e318160d093
Hinz A, Singer S, Brähler E (2014) European reference values for the quality of life questionnaire EORTC QLQ-C30: results of a German investigation and a summarizing analysis of six European general population normative studies. Acta Oncol 53(7):958–965. https://doi.org/10.3109/0284186X.2013.879998
Carver CS (1997) You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med 4(1):92–100. https://doi.org/10.1207/s15327558ijbm0401_6
Carver CS, Scheier MF, Weintraub JK (1989) Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 56(2):267–283
Revenson TA, Schiaffino KM, Deborah Majerovitz S, Gibofsky A (1991) Social support as a double-edged sword: the relation of positive and problematic support to depression among rheumatoid arthritis patients. Soc Sci Med 33(7):807–813. https://doi.org/10.1016/0277-9536(91)90385-p
Ramm GC, Hasenbring M (2003) Die deutsche Adaptation des Illness-specific Social Support Scale und ihre teststatistische Überprüfung beim Einsatz an Patienten vor und nach Knochenmarktransplantation [The German adaptation of the Illness-specific Social Support Scale and the test statistical evaluation on the basis of patients undergoing bone marrow transplantation]. Zeitschrift für Medizinische Psychologie 12(1):29–38
Cohen J (1992) A power primer. Psychol Bull 112(1):155–159
Kim SH, Son BH, Hwang SY, Han W, Yang JH, Lee S, Yun YH (2008) Fatigue and depression in disease-free breast cancer survivors: prevalence, correlates, and association with quality of life. J Pain Symptom Manag 35(6):644–655. https://doi.org/10.1016/j.jpainsymman.2007.08.012
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A (2005) Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 330(7493):702. https://doi.org/10.1136/bmj.38343.670868.D3
Mitchell SA (2010) Cancer-related fatigue: state of the science. PM R 2(5):364–383. https://doi.org/10.1016/j.pmrj.2010.03.024
Quinten C, Coens C, Ghislain I, Zikos E, Sprangers MA, Ringash J, Martinelli F, Ediebah DE, Maringwa J, Reeve BB, Greimel E, King MT, Bjordal K, Flechtner HH, Schmucker-Von Koch J, Taphoorn MJ, Weis J, Wildiers H, Velikova G, Bottomley A, Probe GEC (2015) The effects of age on health-related quality of life in cancer populations: a pooled analysis of randomized controlled trials using the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 involving 6024 cancer patients. Eur J Cancer (Oxford, England: 1990) 51(18):2808–2819. https://doi.org/10.1016/j.ejca.2015.08.027
Ubel PA, Jankovic A, Smith D, Langa KM, Fagerlin A (2005) What is perfect health to an 85-year-old? Med Care 43(10):1054–1057. https://doi.org/10.1097/01.mlr.0000178193.38413.70
Piazza JR, Charles ST, Almeida DM (2007) Living with chronic health conditions: age differences in affective well-being. J Gerontol Ser B Psychol Sci Soc Sci 62(6):P313–P321. https://doi.org/10.1093/geronb/62.6.P313
Acknowledgments
We gratefully acknowledge the support of the Deutsche Krebshilfe e. V. We greatly appreciate the generous support of the physicians participating (including the occupational union of dermatologists), and especially the former patients’ willingness to participate.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol was approved by the Ethics Committee of the Statutory Physician Board of the State of Rhineland Palatinate (Reference number 837.161.11.7703).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tibubos, A.N., Ernst, M., Brähler, E. et al. Fatigue in survivors of malignant melanoma and its determinants: a register-based cohort study. Support Care Cancer 27, 2809–2818 (2019). https://doi.org/10.1007/s00520-018-4587-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4587-1