Abstract
Background
Local anesthesia at the trocar site in laparoscopic cholecystectomy is expected to decrease postoperative pain and hence expedite recovery. The aims of this prospective randomized study were to investigate the effect of local anesthesia and to discover whether it is cost effective.
Methods
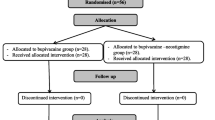
For this study, 100 patients undergoing laparoscopic cholecystectomy were randomized into two groups. The 43 study patients were injected with 0.5% bupivacaine hydrochloride at the trocar site before the trocars were inserted. They then were compared with 41 control patients who received no local anesthesia. The remaining 16 patients were excluded from the study. The postoperative pain was evaluated at the standard four trocar sites at 4 h and 24 h after surgery on a scale 1 (the mildest pain the patient had ever experienced) to 10 (the most severe pain the patient had ever experienced). Postoperative pain medications and their cost were evaluated.
Results
There was no difference between the two groups with regard to gender, age, weight, operative time, estimated operative blood loss, and bile culture. The patients who received bupivacaine at the trocar site clinically had less pain (p<0.001 for all four sites) both at 4 and 24 h after surgery. The treatment group patients used less mepiridine and promethzine than the control group (p=0.001 and 0.002, respectively) postoperatively. Overall, the patients who had local anesthesia used less postoperative pain and antiemetic medication than the control patients (p=0.02). This afforded a significant decrease in the costs and charges of these medications (p=0.004 and 0.005, respectively). Three patients in the study group were discharged from the hospital the day of surgery.
Conclusion
Preinsertion of local anesthesia at the trocar site in laparoscopic cholecystectomy significantly reduces postoperative pain and decreases medication usage costs.
Similar content being viewed by others
References
Benhamou D (1998) Evaluation of postoperative pain. Ann Fr Anesth Reanim 17: 555–572
Bissgaard T, Klarskov B, Kristiansen VB, Callesen T, Schulze S, Kehlet H, Rosenberg J (1999) Multiregional local anesthetic infiltration during laparoscopic cholecystectomy in patients receiving prophylactic multimodal analgesia: a randomized, double-blinded placebo-controlled study. Anesth Analg 89: 1017–1024
Dath D, Park AE (1999) Randomized, controlled trial of bupivacaine injection to decrease pain after laparoscopic cholecystectomy. Can J Surg 42: 284–288
Johnson RC, Hedges AR, Morris R, Stamatakis JD (1999) Ideal pain relief following laparoscopic cholecystectomy. Int J Clin Pract 53: 16–18
Tsimoyiannis EC, Glantzounis G, Lekkas ET, Siakas P, Jabarin M, Tzourou H (1998) Intraperitoneal normal saline and bupivacaine infusion for reduction of postoperative pain after laparoscopic cholecystectomy. Surg Laparosc Endosc 8: 416–420
Author information
Authors and Affiliations
Additional information
Online publication: 5 July 2001
Rights and permissions
About this article
Cite this article
Hasaniya, N.W., Zayed, F.F., Faiz, H. et al. Preinsertion local anesthesia at the trocar site improves perioperative pain and decreases costs of laparoscopic cholecystectomy. Surg Endosc 15, 962–964 (2001). https://doi.org/10.1007/s004640000294
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s004640000294