Abstract
Background
Perforation is a rare but serious adverse event of endoscopic retrograde cholangiopancreatography (ERCP). The aim of this study was to determine the predictors of morbidity and mortality after surgical management of ERCP-related perforation (EP).
Methods
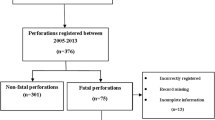
The records of patients with EP requiring surgical intervention at a tertiary referral center in a 12-year period (2004–2016) were retrospectively analyzed for demography, indications for ERCP, risk factors, timing and type of surgical repair, post-operative course, hospital stay, and outcome. Multiple logistic regression was used to identify the parameters predicting survival.
Results
Of 25,300 ERCPs, 380 (1.5%) had EP. Non-operative management was successful in 330 (86.8%) patients. 50 (13.2%) patients were operated for EP. Out of 50, the perforation was detected during ERCP (intra-procedure) in 32 patients (64%). In 30 patients (60%), the surgery was performed within 24 h of ERCP. Twenty patients underwent delayed surgery (after 24 h of ERCP) following the failure of initial non-operative management. The delayed surgery after an unsuccessful medical treatment had a detrimental effect on morbidity, mortality and hospital stay. Post-operative duodenal leak was the only independent predictor of 90-day mortality (p = 0.02, OR = 9.1, 95% CI 1.52–54.64). Addition of T-tube duodenostomy (TTD) to the primary repair for either type I or type II perforations increased post-operative duodenal leak (type I, p = 0.048 and type II; p = 0.001) and mortality (type I, p = 0.009 and type II, p = 0.045).
Conclusion
Although EP is a rare event, it has a serious impact on morbidity and mortality. Delaying of surgery following failed non-operative management worsens the prognosis. Addition of TTD to the repair is not helpful in these patients.

Similar content being viewed by others
References
Stapfer M, Selby RR, Strain SC et al (2000) Management of duodenal perforations after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg 232:191–198
Wu HM, Dixon E, May GR et al (2006) Management of perforation after endoscopic retrograde cholangiopancreatography (ERCP): a population-based review. HPB (Oxford) 8:393–399
Dubecz A, Ottmann J, Schweigert M et al (2012) Management of ERCP-related small bowel perforations: the pivotal role of physical investigation. Can J Surg 55:99–104
Kim J, Lee SH, Paik WH et al (2012) Clinical outcomes of patients who experienced perforations associated with endoscopic retrograde cholangiopancreatography. Surg Endosc 26:3293–3300
Alfieri S, Rosa F, Cina C et al (2013) Management of duodeno-pancreato-biliary perforations after ERCP: outcomes from an Italian tertiary referral center. Surg Endosc 27:2005–2012
Szary NM, Al-Kawas FH (2013) Complications of endoscopic retrograde cholangiopancreatography: how to avoid and manage them. Gastroenterol Hepatol 9:496–504
Andriulli A, Loperfido S, Napolitano G et al (2007) Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102:1781–1788
Machado NO (2012) Management of duodenal perforation postendoscopic retrograde cholangiopancreatography. When and whom to operate and what factors determine the outcome? A review article. JOP 13:18–25
Prachayakul V, Aswakul P (2014) Endoscopic retrograde cholangiopancreatography-related perforation: management and prevention. World J Clin Cases 2:522–527
Bell RC, Van Steigmann G, Goff J et al (1991) Decision for surgical management of perforation following endoscopic sphincterotomy. Am Surg 57:237–240
Loperfido S, Angelini G, Benedetti G et al (1998) Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 48:1–10
Lee TH, Han JH, Park SH (2013) Endoscopic treatment of endoscopic retrograde cholangiopancreatography-related duodenal perforations. Clin Endosc 46:522–528
Avgerinos DV, Llaguna OH, Lo AY et al (2009) Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc 23:833–838
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic co morbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Cotton PB, Lehman G, VennesJ et al (1991) Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37:383–393
Huang L, Yu QS, Zhang Q et al (2015) Comparison between double-guidewire technique and transpancreatic sphincterotomy technique for difficult biliary cannulation. Dig Endosc 27:381–387
Bone RC, Balk RA, Cerra FB et al (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 101:1644–1655
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Slankamenac K, Graf R, Barkun J et al (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Scarlett PY, Falk GL (1994) The management of perforation of the duodenum following endoscopic sphincterotomy: a proposal for selective therapy. Aust N Z J Surg 64:843–846
Ercan M, Bostanci EB, Dalgic T et al (2012) Surgical outcome of patients with perforation after endoscopic retrograde cholangiopancreatography. J Laparoendosc Adv Surg Tech A 22:371–377
Jin YJ, Jeong S, Kim JH et al (2013) Clinical course and proposed treatment strategy for ERCP-related duodenal perforation: a multicenter analysis. Endoscopy 45:806–812
Vezakis A, Fragulidis G, Polydorou A (2015) Endoscopic retrograde cholangiopancreatography-related perforations: diagnosis and management. World J Gastrointest Endosc 7:1135–1141
Knudson K, Raeburn CD, McIntyre RC et al (2008) Management of duodenal and pancreaticobiliary perforations associated with periampullary endoscopic procedures. Am J Surg 196:975–981
Snyder WH, Weigelt JA, Watkins WL et al (1980) The surgical management of duodenal trauma. Precepts based on a review of 247 cases. Arch Surg 115:422–429
Carrillo EH, Richardson JD, Miller FB (1996) Evolution in the management of duodenal injuries. J Trauma 40:1037–1045
DuBose JJ, Inaba K, Teixeira PG et al (2008) Pyloric exclusion in the treatment of severe duodenal injuries: results from the National Trauma Data Bank. Am Surg 74:925–929
Seamon MJ, Pieri PG, Fisher CA et al (2007) A ten-year retrospective review: does pyloric exclusion improve clinical outcome after penetrating duodenal and combined pancreaticoduodenal injuries? J Trauma 62:829–833
Cogbill TH, Moore EE, Feliciano DV et al (1990) Conservative management of duodenal trauma: a multicenter perspective. J Trauma 30:1469–1475
Ivatury RR, Gaudino J, Ascer E et al (1985) Treatment of penetrating duodenal injuries: primary repair vs. repair with decompressive enterostomy/serosal patch. J Trauma 25:337–341
Author information
Authors and Affiliations
Contributions
All authors listed above made substantial contributions to the conception and design of this study, have revised its intellectual content, and have approved of the final submitted version.
Corresponding author
Ethics declarations
Disclosures
The authors Nilesh Patil, Nisha Solanki, Pramod Kumar Mishra, Barjesh Chander Sharma, and Sundeep Singh Saluja have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patil, N.S., Solanki, N., Mishra, P.K. et al. ERCP-related perforation: an analysis of operative outcomes in a large series over 12 years. Surg Endosc 34, 77–87 (2020). https://doi.org/10.1007/s00464-019-06733-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06733-x