Abstract
Background
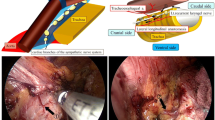
In esophageal squamous cell carcinoma, the number of dissected lymph nodes (LNs), including those along the recurrent laryngeal nerves (RLNs), influences prognosis and nodal staging accuracy. However, dissection of LNs along the RLN increases the risk of complications, especially RLN palsy. Therefore, complete dissection of these LNs with prevention of RLN palsy is recommended. We present herein a new method for lymphadenectomy along the right RLN, named the Pincers maneuver, during thoracoscopic esophagectomy in the prone position (TEP).
Methods
The fundamental concept in this new method is to first exfoliate the two-dimensional membrane (lateral pedicle), which includes the right RLN, LNs along the right RLN, and the primary esophageal artery, from the right side of the trachea toward the neck. Using a Pincers strategy, closing in from the inner and outer sides of the two-dimensional membrane (lateral pedicle), lymphadenectomy along the right RLN toward the right inferior thyroid artery should be easy. This technique was evaluated in 30 consecutive cases of TEP for squamous cell cancer.
Results
There were 15 patients who underwent the new method (Pincers maneuver; Pm) and 15 patients who underwent the conventional method (Cm). There were no significant differences between the two groups in the duration of the thoracic procedure and dissection along the right RLN. No intraoperative and postoperative morbidity related to the right RLN was observed in either group. The Pm group had a higher number of dissected LNs along the right RLN than the Cm group (6.3 vs 3.1, p = 0.044).
Conclusions
The Pincers maneuver for lymphadenectomy along the right RLN during TEP is technically safe and feasible. It increases the number of dissected LNs along the right RLN.






Similar content being viewed by others
References
Altorki NK, Zhou XK, Stiles B, Port JL, Paul S, Lee PC, Mazumdar M (2008) Total number of resected lymph nodes predicts survival in esophageal cancer. Ann Surg 248:221–226
Rizk NP, Ishwaran H, Rice TW, Chen LQ, Schipper PH, Kesler KA, Law S, Lerut TE, Reed CE, Salo JA, Scott WJ, Hofstetter WL, Watson TJ, Allen MS, Rusch VW, Blackstone EH (2010) Optimum lymphadenectomy for esophageal cancer. Ann Surg 251:46–50
Lin CS, Cheng CT, Liu CY, Lee MY, Hsiao MC, Shih CH, Liu CC (2015) Radical lymph node dissection in primary esophagectomy for esophageal squamous cell carcinoma. Ann Thorac Surg 100:278–286
Watanabe H, Kato H, Tachimori Y (2000) Significance of extended systemic lymph node dissection for thoracic esophageal carcinoma in Japan. Recent Results Cancer Res 155:123–133
Shiozaki H, Yano M, Tsujinaka T, Inoue M, Tamura S, Doki Y, Yasuda T, Fujiwara Y, Monden M (2001) Lymph node metastasis along the recurrent nerve chain is an indication for cervical lymph node dissection in thoracic esophageal cancer. Dis Esophagus 14:191–196
Tsurumaru M, Kajiyama Y, Udagawa H, Akiyama H (2001) Outcomes of extensive lymph node dissection for squamous cell carcinoma of the thoracic esophagus. Ann Thorac Cardiovasc Surg 7:325–329
Gockel I, Kneist W, Keilmann A, Junginger T (2005) Recurrent laryngeal nerve paralysis (RLNP) following esophagectomy for carcinoma. Eur J Surg Oncol 31:277–281
Hulscher JB, van Sandick JW, Devriese PP, van Lanschot JJ, Obertop H (1999) Vocal cord paralysis after subtotal oesophagectomy. Br J Surg 86:1583–1587
Baba M, Natsugoe S, Shimada M, Nakano S, Noguchi Y, Kawachi K, Kusano C, Aikou T (1999) Does hoarseness of voice from recurrent nerve paralysis after esophagectomy for carcinoma influence patient quality of life? J Am Coll Surg 188:231–236
Sato Y, Kosugi SI, Aizawa N, Ishikawa T, Kano Y, Ichikawa H, Hanyu T, Hirashima K, Bamba T, Wakai T (2015) Risk factors and clinical outcomes of recurrent laryngeal nerve paralysis after esophagectomy for thoracic esophageal carcinoma. World J Surg 40:129–136
Osugi H, Takemura M, Higashino M, Takada N, Lee S, Kinoshita H (2003) A comparison of video-assisted thoracoscopic oesophagectomy and radical lymph node dissection for squamous cell cancer of the oesophagus with open operation. Br J Surg 90:108–113
Palanivelu C, Prakash A, Senthikumar R, Senthilnathan P, Parthasarathi R, Rajan PS, Venkatachlam S (2006) Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position experience of 130 patients. J Am Coll Surg 203:7–16
The Japan Esophageal Society (2015) Japanese classification of esophageal cancer, 11th edn. Kanehara & Co., Ltd, Tokyo, pp 1–128
Sannohe Y, Hiratsuka R, Doki K (1981) Lymph node metastases in cancer of the thoracic esophagus. Am J Surg 141:216–218
Ma GW, Situ DR, Ma QL, Long H, Zhang LJ, Lin P, Rong TH (2014) Three-field vs two-field lymph node dissection for esophageal cancer: a meta-analysis. World J Gastroenterol 20:18022–18030
Rice TW, Blackstone EH, Rusch VW (2010) 7th edition of the AJCC cancer staging manual: esophagus and esophagogastric junction. Ann Surg Oncol 17:1721–1724
Chen J, Wu S, Zheng X, Pan J, Zhu K, Chen Y, Li J, Liao L, Lin Y, Liao Z (2014) Cervical lymph node metastasis classified as regional nodal staging in thoracic esophageal squamous cell carcinoma after radical esophagectomy and three-field lymph node dissection. BMC Surg 14:110
Yamasaki M, Miyata H, Miyazaki Y, Takahashi T, Kurokawa Y, Nakajima K, Takiguchi S, Mori M, Doki Y (2014) Evaluation of the Nodal Status in the 7th edition of the UICC-TNM classification for esophageal squamous cell carcinoma: proposed modifications for improved survival stratification. Ann Surg Oncol 21:2850–2856
Oshikiri T, Yasuda T, Harada H, Goto H, Oyama M, Hasegawa H, Ohara T, Sendo H, Nakamura T, Fujino Y, Tominaga M, Kakeji Y (2015) A new method (the “Bascule method”) for lymphadenectomy along the left recurrent laryngeal nerve during prone esophagectomy for esophageal cancer. Surg Endosc 29:2442–2450
Salassa JR, Pearson BW, Payne WS (1977) Gross and microscopical blood supply of the trachea. Ann Thorac Surg 24:100–107
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Taro Oshikiri, Tetsu Nakamura, Yukiko Miura, Masashi Yamamoto, Shingo Kanaji, Kimihiro Yamashita, Takeru Matsuda, Yasuo Sumi, Satoshi Suzuki, and Yoshihiro Kakeji have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Oshikiri, T., Nakamura, T., Miura, Y. et al. A new method (the “Pincers maneuver”) for lymphadenectomy along the right recurrent laryngeal nerve during thoracoscopic esophagectomy in the prone position for esophageal cancer. Surg Endosc 31, 1496–1504 (2017). https://doi.org/10.1007/s00464-016-5124-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5124-2