Abstract
Background
The use of simulation to train novice surgeons in laparoscopic skills is becoming increasingly popular. To maximize benefit from simulation, training needs to be delivered and assessed in a structured manner. This study aimed to define performance goals, demonstrate construct validity of the training program, and evaluate whether novice surgeons could reach the preset performance goals.
Methods
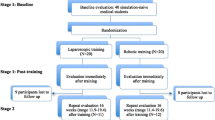
Nine expert laparoscopic surgeons established performance goals for three basic modules of an augmented-reality laparoscopic simulator. The three laparoscopic modules were used by 40 novice surgeons and 40 surgical trainees (postgraduate years [PGYs] 1–4). The performance outcomes were analyzed across the different groups (novice, PGYs 1 and 2, PGYs 3 and 4, expert) to determine construct validity. Then 26 recruited novices trained on the three modules with the aim of reaching the performance goals.
Results
The results demonstrated a significant difference in performance between all levels of experience for time (p < 0.001), motion analysis (p < 0.001), and error score (p < 0.001), thus demonstrating construct validity. All 26 novice surgeons significantly improved in performance with repetition for the metrics of time (p < 0.001) and motion analysis (p < 0.001). For two of the modules, the proficiency goals were reached in fewer than 10 trials by 80 % of the study participants.
Conclusion
Basic skills in laparoscopic surgery can be learned and improved using proficiency-based simulation training. It is possible for novice surgeons to achieve predefined performance goals in a reasonable time frame.


Similar content being viewed by others

References
European Communities (organisation of working time; activities of doctors in training) Regulations 2004 Statutory Instrument S.I. No. 494 of 2004. Available at www.dohc.ie/legislation. Accessed 12 Jan 2012
Kennedy I (2001) Learning from Bristol: the report of the public enquiry into children’s heart surgery at the Bristol Royal Infirmary 1984–1995. Command paper CM 5207. Available at http://www.bristol-inquiry.org.uk. Accessed 10 Jan 2012
Kohn LT, Corrigan JM, Donaldson M (1999) To err is human: building a safer health system. Institute of Medicine, Washington, DC
Asch DA, Parker RM (1988) The Libby Zion case: one step forward or two steps backward? N Engl J Med 318:771–775
Bridges M, Diamond DL (1999) The financial impact of teaching surgical residents in the operating room. Am J Surg 117:28–32
Southern Surgeons Club (1995) The learning curve of laparoscopic cholecystectomy. Am J Surg 170:55–59
Gallagher AG, McClure N, McGuigan J, Ritchie K, Sheehy NP (1998) An ergonomic analysis of the fulcrum effect in the acquisition of endoscopic skills. Endoscopy 30:617–620
Gallagher AG, Ritter EM, Lederman AB, McClusky DA III, Smith CD (2005) Video-assisted surgery represents more than a loss of three-dimensional vision. Am J Surg 189:76–80
Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MCl (1993) Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg 165:9–14
Flum DR, Koepsel T, Heagerty P, Pelligrini CA (2002) The nationwide frequency of major adverse outcomes in antireflux surgery and the role of surgeon experience, 1992–1997. J Am Coll Surg 195:611–618
Sturm LP, Windsor JA, Cosman PH, Cregan P, Hewett PJ, Maddern GJ (2008) A systematic review of skills transfer after surgical simulation training. Ann Surg 248:166–179
Stefanidis D, Korndorffer JR Jr, Sierra R, Touchard C, Dunne JB, Scott DJ (2005) Skill retention following proficiency based laparoscopic simulator training. Surgery 138:165–170
Seymour N, Gallagher AG, O’Brien M, Roman S, Andersen D, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–464
Aggarwal R, Grantcharov TP, Darzi A (2007) Framework for systematic training and assessment of technical skills. J Am Coll Surg 204:697–705
Chodhary RK (2004) Qualities of a good surgeon. Br Med J 329:314
Anjum SN, Quinn P, Anwar R (2005) Qualities of a good surgeon. Br Med J 331:1176
Pellen MG, Horgan LF, Barton JR, Attwood SE (2009) Construct validity of the ProMIS laparoscopic simulator. Surg Endosc 23:130–139
Aggarwal R, Crochet P, Dias A, Misra A, Ziprin P, Darzi A (2009) Development of a virtual reality training curriculum for laparoscopic cholecystectomy. Br J Surg 96:1086–1093
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K, SAGESFLS Committee (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135:21–27
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room: a randomized controlled trial. Am J Surg 199:115–120
Soper NJ, Fried GM (2008) The fundamentals of laparoscopic surgery: its time has come. Bull Am Coll Surg 93:30–32
Brinkman WM, Buzink SN, Alevizos L, de Hingh IH, Jakimowicz JJ (2012) Criterion-based laparoscopic training reduces total training time. Surg Endosc 26:1095–1101
Verdaasdonk EG, Dankelman J, Lange JF, Stassen LP (2008) Incorporation of proficiency criteria for basic laparoscopic skills training: how does it work? Surg Endosc 22:2609–2615
Stefanidis D, Acker CE, Greene FL (2010) Performance goals on simulators boost resident motivation and skills laboratory attendance. J Surg Educ 67:66–70
Grantcharov TP, Funch-Jensen P (2009) Can everyone achieve proficiency with the laparoscopic technique? Learning curve patterns in technical skills acquisition. Am J Surg 197:447–449
Hassan I, Gerdes B, Koller M, Dick B, Hellwig D, Rothmund M, Zielke A (2007) Spatial perception predicts laparoscopic skills on virtual reality laparoscopy simulator. Childs Nerv Syst 23:685–689
Hedman L, Ström P, Andersson P, Kjellin A, Wredmark T, Felländer-Tsai L (2006) High-level visual–spatial ability for novices correlates with performance in a visual–spatial complex surgical simulator task. Surg Endosc 20:1275–1280
Ritter EM, McClusky DA 3rd, Gallagher AG, Enochsson L, Smith CD (2006) Perceptual, visuospatial, and psychomotor abilities correlate with duration of training required on a virtual-reality flexible endoscopy simulator. Am J Surg 192:379–384
Stefandis D, Hope WW, Korndorffer JR Jr, Markley S, Scott DJ (2010) Initial laparoscopic basic skills training shortens the learning curve of laparoscopic suturing and is cost effective. J Am Coll Surg 210:436–440
Disclosures
Emmeline Nugent, Nicole Shirilla, Adnan Hafeez, Diarmuid S. O’Riordain, Oscar Traynor, Anthony M. Harrison, and Paul Neary have no conflicts of interest or financial ties to disclosure.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nugent, E., Shirilla, N., Hafeez, A. et al. Development and evaluation of a simulator-based laparoscopic training program for surgical novices. Surg Endosc 27, 214–221 (2013). https://doi.org/10.1007/s00464-012-2423-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2423-0