Abstract
Background and aims
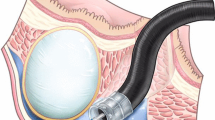
Based on our experience with endoscopic submucosal dissection (ESD) and new endoscopic techniques for endoscopic closure of iatrogenic upper gastrointestinal (upper-GI) perforations, we developed methods to remove upper-GI subepithelial tumors (SETs) originating from the muscularis propria by endoscopic muscularis dissection (EMD). The aim of this study is to evaluate the clinical feasibility and safety of EMD.
Methods
31 patients with upper-GI SETs originating from the muscularis propria were treated by EMD. The EMD differed from ESD in (1) precutting the overlying mucosa above the lesion by using snare or longitudinal incision instead of circumferential incision, (2) dissecting the complete tumors away from submucosal and muscularis propria tissue by electrical dissection combined with blunt dissection, and (3) closing the wound with clips. Perforations occurring during dissection were closed by endoscopic methods.
Results
30 of 31 tumors were resected completely (96.8 %). One esophageal lesion was resected partially because of severe adhesions with surrounding tissue. Mean resected tumor size was 22.1 mm × 15.5 mm, and mean operation time was 76.8 min (range 15–330 min). Histological diagnosis was gastrointestinal stromal tumor (GIST) in 16 lesions [6 esophageal, 3 cardial, 7 gastric; 6 very low risk and 10 low risk according to the National Institutes of Health (NIH) risk classification] and leiomyoma in 15 lesions (8 esophageal, 4 cardial, 3 gastric). No patient developed delayed hemorrhage. Perforation occurred in four patients (12.9 %), all of which were managed successfully by endoscopic techniques. The mean follow-up time was 17.7 months (range 7–35 months). Follow-up found no tumor recurrence in any patient.
Conclusions
In this early experience, EMD appears to be a feasible and minimally invasive treatment for some patients with upper-GI SETs originating from the muscularis propria. Although there is a higher risk of perforation than with ESD, this will improve with extended practice, and perforations have become manageable endoscopically.



Similar content being viewed by others
References
Kawamoto K, Yamada Y, Furukawa N, Utsunomiya T, Haraguchi Y, Mizuguchi M, Oiwa T, Takano H, Masuda K (1997) Endoscopic submucosal tumorectomy for gastrointestinal submucosal tumors restricted to the submucosa: a new form of endoscopic minimal surgery. Gastrointest Endosc 46:311–317
Hyun JH, Jeen YT, Chun HJ, Lee HS, Lee SW, Song CW, Choi JH, Um SH, Kim CD, Ryu HS (1997) Endoscopic resection of submucosal tumor of the esophagus: results in 62 patients. Endoscopy 29:165–170
Connolly EM, Gaffney E, Reynolds JV (2003) Gastrointestinal stromal tumours. Br J Surg 90:1178–1186
Lee IL, Lin PY, Tung SY, Shen CH, Wei KL, Wu CS (2006) Endoscopic submucosal dissection for the treatment of intraluminal gastric subepithelial tumors originating from the muscularis propria layer. Endoscopy 38:1024–1028
Bialek A, Wiechowska-Kozlowska A, Huk J (2010) Endoscopic submucosal dissection of large gastric stromal tumor arising from muscularis propria. Clin Gastroenterol Hepatol 8:e119–e120
Raju GS (2009) Endoscopic closure of gastrointestinal leaks. Am J Gastroenterol 104:1315–1320
Costamagna G, Marchese M (2010) Management of esophageal perforation after therapeutic endoscopy. Gastroenterol Hepatol 6:391–392
Mangiavillano B, Viaggi P, Masci E (2010) Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis 11:12–18
Madanick RD (2008) Medical management of iatrogenic esophageal perforations. Curr Treat Options Gastroenterol 11:54–63
Nishida T, Hirota S, Yanagisawa A, Sugino Y, Minami M, Yamamura Y, Otani Y, Shimada Y, Takahashi F, Kubota T, GIST Guideline Subcommittee (2008) Clinical practice guidelines for gastrointestinal stromal tumor (GIST) in Japan: English version. Int J Clin Oncol 13:416–430
Reddy P, Boci K, Charbonneau C (2007) The epidemiologic, health-related quality of life, and economic burden of gastrointestinal stromal tumours. J Clin Pharm Ther 32:557–565
Sepe PS, Brugge WR (2009) A guide for the diagnosis and management of gastrointestinal stromal cell tumors. Nat Rev Gastroenterol Hepatol 6:363–371
Kojima T, Takahashi H, Parra-Blanco A, Kohsen K, Fujita R (1999) Diagnosis of submucosal tumor of the upper GI tract by endoscopic resection. Gastrointest Endosc 50:516–522
Hwang JC, Kim JH, Kim JH, Shin SJ, Cheong JY, Lee KM, Yoo BM, Lee KJ, Cho SW (2009) Endoscopic resection for the treatment of gastric subepithelial tumors originated from the muscularis propria layer. Hepatogastroenterology 56:1281–1286
Tamiya Y, Nakahara K, Kominato K, Serikawa O, Watanabe Y, Tateishi H, Takedatsu H, Toyonaga A, Sata M (2010) Pneumomediastinum is a frequent but minor complication during esophageal endoscopic submucosal dissection. Endoscopy 42:8–14
Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC (2004) Evolving options in the management of esophageal perforation. Ann Thorac Surg 77:1475–1483
Tanaka M, Ono H, Hasuike N, Takizawa K (2008) Endoscopic submucosal dissection of early gastric cancer. Digestion 77(Suppl 1):23–28
Farhat S, Chaussade S, Ponchon T, Coumaros D, Charachon A, Barrioz T, Koch S, Houcke P, Cellier C, Heresbach D, Lepilliez V, Napoleon B, Bauret P, Coron E, Le Rhun M, Bichard P, Vaillant E, Calazel A, Bensoussan E, Bellon S, Mangialavori L, Robin F, Prat F, SFED ESD study group (2011) Endoscopic submucosal dissection in a European setting. A multi-institutional report of a technique in development. Endoscopy 43:664–670
van Heel NC, Haringsma J, Spaander MC, Bruno MJ, Kuipers EJ (2010) Short-term esophageal stenting in the management of benign perforations. Am J Gastroenterol 105:1515–1520
Schmidt SC, Strauch S, Rösch T, Veltzke-Schlieker W, Jonas S, Pratschke J, Weidemann H, Neuhaus P, Schumacher G (2010) Management of esophageal perforations. Surg Endosc 24:2809–2813
Amrani L, Ménard C, Berdah S, Emungania O, Soune PA, Subtil C, Brunet C, Grimaud JC, Barthet M (2009) From iatrogenic digestive perforation to complete anastomotic disunion: endoscopic stenting as a new concept of “stent-guided regeneration and re-epithelialization”. Gastrointest Endosc 69:1282–1287
Binmoeller KF, Grimm H, Soehendra N (1993) Endoscopic closure of a perforation using metallic clips after snare excision of a gastric leiomyoma. Gastrointest Endosc 39:172–174
Grupka MJ, Benson J (2008) Endoscopic clipping. J Dig Dis 9:72–78
Raju GS, Gajula L (2004) Endoclips for GI endoscopy. Gastrointest Endosc 59:267–279
Grotz TE, Donohue JH (2011) Surveillance strategies for gastrointestinal stromal tumors. J Surg Oncol 104:921–927
Joensuu H (2008) Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol 39:1411–1419
Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF, Schuetze S, Sundar HM, Trent JC, Wayne JD (2010) NCCN Task Force report:updateon the managementof patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 8:S1–S41
Takahashi T, Nakajima K, Nishitani A, Souma Y, Hirota S, Sawa Y, Nishida T (2007) An enhanced risk-group stratification system for more practical prognostication of clinically malignant gastrointestinal stromal tumors. Int J Clin Oncol 12:369–374
Kingham TP, DeMatteo RP (2009) Multidisciplinary treatment of gastrointestinal stromal tumors. Surg Clin North Am 89:217–233
Disclosures
Authors Bing-Rong Liu, Ji-Tao Song, Bo Qu, Ji-Feng Wen, Ji-Bin Yin, and Wei Liu have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, BR., Song, JT., Qu, B. et al. Endoscopic muscularis dissection for upper gastrointestinal subepithelial tumors originating from the muscularis propria. Surg Endosc 26, 3141–3148 (2012). https://doi.org/10.1007/s00464-012-2305-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2305-5