Abstract
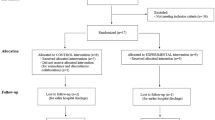
Dysphagia is common after stroke. Neuromuscular electrical stimulation (NMES) and fiberoptic endoscopic evaluation of swallowing (FEES) for the treatment of dysphagia have gained in popularity, but the combined application of these promising modalities has rarely been studied. We aimed to evaluate whether combined NMES, FEES, and traditional swallowing rehabilitation can improve swallowing functions in stroke patients with moderate to severe dysphagia. Thirty-two patients with moderate to severe dysphagia poststroke (≥3 weeks) were recruited. Patients received 12 sessions of NMES for 1 h/day, 5 days/week within a period of 2–3 weeks. FEES was done before and after NMES for evaluation and to guide dysphagic therapy. All patients subsequently received 12 sessions of traditional swallowing rehabilitation (50 min/day, 3 days/week) for 4 weeks. Primary outcome measure was the Functional Oral Intake Scale (FOIS). Secondary outcome measures included clinical degree of dysphagia, the patient’s self-perception of swallowing ability, and the patient’s global satisfaction with therapy. Patients were assessed at baseline, after NMES, at 6-month follow-up, and at 2-year follow-up. Twenty-nine patients completed the study. FOIS, degree of dysphagia, and patient’s self-perception of swallowing improved significantly after NMES, at the 6-month follow-up, and at the 2-year follow-up (p < 0.001, each compared with baseline). Most patients reported considerable satisfaction with no serious adverse events. Twenty-three of the 29 (79.3 %) patients maintained oral diet with no pulmonary complications at 2-year follow-up. This preliminary case series demonstrated that combined NMES, FEES, and traditional swallowing rehabilitation showed promise for improving swallowing functions in stroke patients with moderate-to-severe dysphagia. The benefits were maintained for up to 2 years. The results are promising enough to justify further studies.


Similar content being viewed by others
References
Mann G, Hankey GJ, Cameron D. Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis. 2000;10:380–6.
Smithard DG, O’Neill PA, England RE, et al. The natural history of dysphagia following a stroke. Dysphagia. 1997;12:188–93.
Teasell RW, Bach D, McRae M. Prevalence and recovery of aspiration poststroke: a retrospective analysis. Dysphagia. 1994;9:35–9.
Dziewas R, Ritter M, Schilling M, et al. Pneumonia in acute stroke patients fed by nasogastric tube. J Neurol Neurosurg Psychiatry. 2004;75:852–6.
Geeganage C, Beavan J, Ellender S et al. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Syst Rev. 2012:CD000323.
Merletti R, Zelaschi F, Latella D, Galli M, Angeli S, Bellucci Sessa M. A control study of muscle force recovery in hemiparetic patients during treatment with functional electrical stimulation. Scand J Rehabil Med. 1987;10:147–54.
Hainaut K, Duchateau J. Neuromuscular electrical stimulation and voluntary exercise. Sports Med. 1992;14:100–13.
Freed ML, Freed L, Chatburn RL, Christian M. Electrical stimulation for swallowing disorders caused by stroke. Respir Care. 2001;46:466–74.
Lake DA. Neuromuscular electrical stimulation. An overview, and its application in the treatment of sports injuries. Sports Med. 1992;13:320–36.
Bulow M, Speyer R, Baijens L, Woisard V, Ekberg O. Neuromuscular electrical stimulation (NMES) in stroke patients with oral and pharyngeal dysfunction. Dysphagia. 2008;23:302–9.
Carnaby-Mann GD, Crary MA. Adjunctive neuromuscular electrical stimulation for treatment-refractory dysphagia. Ann Otol Rhinol Laryngol. 2008;117:279–87.
Hamdy S, Rothwell JC, Aziz Q, Thompson DG. Organization and reorganization of human swallowing motor cortex: implications for recovery after stroke. Clin Sci. 2000;99:151–7.
Fraser C, Rothwell J, Power M, Hobson A, Thompson D, Hamdy S. Differential changes in human pharyngoesophageal motor excitability induced by swallowing, pharyngeal stimulation, and anesthesia. Am J Physiol Gastrointest Liver Physiol. 2003;285:137–44.
Carnaby-Mann GD, Crary MA. Examining the evidence on neuromuscular electrical stimulation for swallowing. Arch Otolaryngol Head Neck Surg. 2007;133:564–71.
Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2:216–9.
Langmore SE, McCulloch TM. Examination of the pharynx and larynx and endoscopic examination of pharyngeal swallowing. In: Perlman A, Shulze C, editors. Deglutition and its disorders. San Diego: Singular Publishing; 1996. p. 201–26.
Langmore SE. Endoscopic evaluation and treatment of swallowing disorders. New York: Thieme; 2001.
Leder SB. Serial fiberoptic endoscopic swallowing evaluations in the management of patients with dysphagia. Arch Phys Med Rehabil. 1998;79:1264–9.
Crary MA, Carnaby Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20.
Ludlow CL, Humbert I, Saxon K, Poletto C, Sonies B, Crujido L. Effects of surface electrical stimulation both at rest and during swallowing in chronic pharyngeal dysphagia. Dysphagia. 2007;22:1–10.
Freed M, Wijting Y. VitalStim Certification Program. Training manual for patient assessment, treatment using VitalStim electrical stimulation. Hixson: Chattanooga Group; 2003.
Erketin C, Aydogdu I, Tarlaci S, Turman AB, Kiylioglu N. Mechanism of dysphagia in suprabulbar palsy with lacunar infarct. Stroke. 2000;31:1370–6.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke. Prognosis and prognostic factors at 6 months. Stroke. 1999;30:744–8.
Martin L, Cometti G, Pousson M, Morlon B. Effect of electrical stimulation training on the contractile characteristics of the triceps surae muscle. Eur J Appl Physiol. 1993;67:457–61.
Leelamanit V, Limsakul C, Geater A. Synchronized electrical stimulation in treating pharyngeal dysphagia. Laryngoscope. 2002;112:2204–10.
Oh BM, Kim DY, Paik NJ. Recovery of swallowing function is accompanied by the expansion of the cortical map. Int J Neurosci. 2007;117:1215–27.
Snyder-Mackler L, Delitto A, Bailey SL, Stralka SW. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. J Bone Joint Surg Am. 1995;77:1166–73.
DeKroon JR, Ijzermann MJ, Chae J, Lankhorst GJ, Zilvold G. Relation between stimulation characteristics and clinical outcome in studies using electrical stimulation to improve motor control of the upper extremity in stroke. J Rehabil Med. 2005;37:65–74.
Shaw GY, Sechtem PR, Searl J, Keller K, Rawi TA, Dowdy E. Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: myth or reality? Ann Otol Rhinol Laryngol. 2007;116:36–44.
Halper A, Cherney L, Cichowski K, Zhang M. Dysphagia after head trauma: The effects of cognitive-communicative impairments on functional outcomes. J Head Trauma. 1999;14:489–96.
Acknowledgments
This study was supported by an academic research fund from Kaohsiung Veterans General Hospital (VGHKS96-079). The study is registered in http://www.clinicaltrials.gov (unique identifier: NCT01731847).
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, SF., Hsu, CW., Lin, HS. et al. Combined Neuromuscular Electrical Stimulation (NMES) with Fiberoptic Endoscopic Evaluation of Swallowing (FEES) and Traditional Swallowing Rehabilitation in the Treatment of Stroke-Related Dysphagia. Dysphagia 28, 557–566 (2013). https://doi.org/10.1007/s00455-013-9466-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-013-9466-9