Abstract
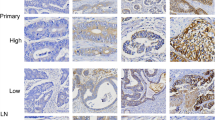
The clinical and prognostic significance of HER3 expression and its relation to HER2 status in primary colorectal cancer (pCRC) were investigated. We retrospectively analysed 365 consecutive cases of pCRC that had been previously evaluated for HER2 status and included their 143 matched lymph node metastases. Immunohistochemistry (IHC) was performed to assess HER3 expression using tissue array methods. Of 364 eligible patients, HER3 overexpression was detected in 251 cases (69 %) (IHC 2+, n = 186 and IHC 3+, n = 65). HER3 overexpression was inversely correlated with histologic grade (p = 0.006), tumour size (p < 0.001), tumour depth (p < 0.001), TNM stage (p = 0.002), lymphatic invasion (p = 0.004), lymph node metastasis (p = 0.013) and distant metastasis (p = 0.039). Moreover, it positively correlated with both HER2 overexpression (p = 0.007) and HER2 gene amplification (p = 0.006). Although HER3 overexpression was associated with longer survival in univariate analysis (p = 0.026), it was not an independent prognostic factor in multivariate analysis (p = 0.359). Moreover, co-alteration of HER3 and HER2 was associated with neither survival nor any clinicopathologic parameter except tumour location in the rectum. Although not an independent prognostic factor for overall survival, HER3 overexpression was associated with several favourable prognostic clinicopathologic parameters. Additionally, HER3 overexpression strongly correlated with HER2 positivity in this cohort of patients.


Similar content being viewed by others
References
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA: Cancer J Clin 64(1):9–29
Fearon ER, Vogelstein B (1990) A genetic model for colorectal tumorigenesis. Cell 61(5):759–767
Markowitz SD, Bertagnolli MM (2009) Molecular origins of cancer: molecular basis of colorectal cancer. N Engl J Med 361(25):2449–2460. doi:10.1056/NEJMra0804588
Network CGA (2012) Comprehensive molecular characterization of human colon and rectal cancer. Nature 487(7407):330–337. doi:10.1038/nature11252
Budinska E, Popovici V, Tejpar S, D’Ario G, Lapique N, Sikora KO, Di Narzo AF, Yan P, Hodgson JG, Weinrich S, Bosman F, Roth A, Delorenzi M (2013) Gene expression patterns unveil a new level of molecular heterogeneity in colorectal cancer. J Pathol 231(1):63–76. doi:10.1002/path.4212
Miyakura Y, Sugano K, Konishi F, Ichikawa A, Maekawa M, Shitoh K, Igarashi S, Kotake K, Koyama Y, Nagai H (2001) Extensive methylation of hMLH1 promoter region predominates in proximal colon cancer with microsatellite instability. Gastroenterology 121(6):1300–1309
Bosman FT, Carneiro F, Hruban RH, Theise ND (2010) WHO classification of tumours of the digestive system. vol Ed. 4. World Health Organization
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474. doi:10.1245/s10434-010-0985-4
Edge SB, Byrd DR, Compton C, Fritz A, Greene F, Trotti A (2010) American joint committee on cancer staging manual. American Joint Committee on Cancer Staging Manual
Beji A, Horst D, Engel J, Kirchner T, Ullrich A (2012) Toward the prognostic significance and therapeutic potential of HER3 receptor tyrosine kinase in human colon cancer. Clin Cancer Res 18(4):956–968. doi:10.1158/1078-0432.ccr-11-1186
Ledel F, Hallstrom M, Ragnhammar P, Ohrling K, Edler D (2014) HER3 expression in patients with primary colorectal cancer and corresponding lymph node metastases related to clinical outcome. Eur J Cancer 50(3):656–662. doi:10.1016/j.ejca.2013.11.008
Jaiswal BS, Kljavin NM, Stawiski EW, Chan E, Parikh C, Durinck S, Chaudhuri S, Pujara K, Guillory J, Edgar KA, Janakiraman V, Scholz RP, Bowman KK, Lorenzo M, Li H, Wu J, Yuan W, Peters BA, Kan Z, Stinson J, Mak M, Modrusan Z, Eigenbrot C, Firestein R, Stern HM, Rajalingam K, Schaefer G, Merchant MA, Sliwkowski MX, de Sauvage FJ, Seshagiri S (2013) Oncogenic ERBB3 mutations in human cancers. Cancer Cell 23(5):603–617. doi:10.1016/j.ccr.2013.04.012
Hynes NE, Lane HA (2005) ERBB receptors and cancer: the complexity of targeted inhibitors. Nat Rev Cancer 5(5):341–354. doi:10.1038/nrc1609
Jiang N, Saba NF, Chen ZG (2012) Advances in targeting HER3 as an anticancer therapy. Chemother Res Pract 2012:817304. doi:10.1155/2012/817304
Begnami MD, Fukuda E, Fregnani JH, Nonogaki S, Montagnini AL, da Costa WL Jr, Soares FA (2011) Prognostic implications of altered human epidermal growth factor receptors (HERs) in gastric carcinomas: HER2 and HER3 are predictors of poor outcome. J Clin Oncol 29(22):3030–3036. doi:10.1200/jco.2010.33.6313
Yoon HH, Sukov WR, Shi Q, Sattler CA, Wiktor AE, Diasio RB, Wu TT, Jenkins RB, Sinicrope FA (2013) HER-2/neu gene amplification in relation to expression of HER2 and HER3 proteins in patients with esophageal adenocarcinoma. Cancer. doi:10.1002/cncr.28435
Hsieh AC, Moasser MM (2007) Targeting HER proteins in cancer therapy and the role of the non-target HER3. Br J Cancer 97(4):453–457. doi:10.1038/sj.bjc.6603910
Montemurro F, Scaltriti M (2014) Biomarkers of drugs targeting HER-family signalling in cancer. J Pathol 232(2):219–229. doi:10.1002/path.4269
Baselga J, Swain SM (2009) Novel anticancer targets: revisiting ERBB2 and discovering ERBB3. Nat Rev Cancer 9(7):463–475. doi:10.1038/nrc2656
Kapitanovic S, Radosevic S, Slade N, Kapitanovic M, Andelinovic S, Ferencic Z, Tavassoli M, Spaventi S, Pavelic K, Spaventi R (2000) Expression of erbB-3 protein in colorectal adenocarcinoma: correlation with poor survival. J Cancer Res Clin Oncol 126(4):205–211
Lee JC, Wang ST, Chow NH, Yang HB (2002) Investigation of the prognostic value of coexpressed ErbB family members for the survival of colorectal cancer patients after curative surgery. Eur J Cancer 38(8):1065–1071
Kountourakis P, Pavlakis K, Psyrri A, Rontogianni D, Xiros N, Patsouris E, Pectasides D, Economopoulos T (2006) Prognostic significance of HER3 and HER4 protein expression in colorectal adenocarcinomas. BMC Cancer 6:46. doi:10.1186/1471-2407-6-46
Baiocchi G, Lopes A, Coudry RA, Rossi BM, Soares FA, Aguiar S, Guimaraes GC, Ferreira FO, Nakagawa WT (2009) ErbB family immunohistochemical expression in colorectal cancer patients with higher risk of recurrence after radical surgery. Int J Colorectal Dis 24(9):1059–1068. doi:10.1007/s00384-009-0702-6
Ljuslinder I, Malmer B, Isaksson-Mettavainio M, Oberg A, Henriksson R, Stenling R, Palmqvist R (2009) ErbB 1-4 expression alterations in primary colorectal cancers and their corresponding metastases. Anticancer Res 29(5):1489–1494
Seo AN, Kwak Y, Kim DW, Kang SB, Choe G, Kim WH, Lee HS (2014) HER2 status in colorectal cancer: its clinical significance and the relationship between HER2 gene amplification and expression. PLoS One 9(5):e98528. doi:10.1371/journal.pone.0098528
Lee HS, Cho SB, Lee HE, Kim MA, Kim JH, Park do J, Kim JH, Yang HK, Lee BL, Kim WH (2007) Protein expression profiling and molecular classification of gastric cancer by the tissue array method. Clin Cancer Res 13(14):4154–4163. doi:10.1158/1078-0432.ccr-07-0173
Hofmann M, Stoss O, Shi D, Buttner R, van de Vijver M, Kim W, Ochiai A, Ruschoff J, Henkel T (2008) Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology 52(7):797–805. doi:10.1111/j.1365-2559.2008.03028.x
Oh JR, Kim DW, Lee HS, Lee HE, Lee SM, Jang JH, Kang SB, Ku JL, Jeong SY, Park JG (2012) Microsatellite instability testing in Korean patients with colorectal cancer. Fam Cancer 11(3):459–466. doi:10.1007/s10689-012-9536-4
Kim JH, Bae JM, Kim KJ, Rhee YY, Kim Y, Cho NY, Lee HS, Chang MS, Kang GH (2014) Differential features of microsatellite-unstable colorectal carcinomas depending on EPCAM expression status. Korean J Pathol 48(4):276–282. doi:10.4132/KoreanJPathol.2014.48.4.276
Baselga J, Cortes J, Kim SB, Im SA, Hegg R, Im YH, Roman L, Pedrini JL, Pienkowski T, Knott A, Clark E, Benyunes MC, Ross G, Swain SM (2012) Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med 366(2):109–119. doi:10.1056/NEJMoa1113216
Swain SM, Kim SB, Cortes J, Ro J, Semiglazov V, Campone M, Ciruelos E, Ferrero JM, Schneeweiss A, Knott A, Clark E, Ross G, Benyunes MC, Baselga J (2013) Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA study): overall survival results from a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol 14(6):461–471. doi:10.1016/s1470-2045(13)70130-x
Iida M, Brand TM, Starr MM, Huppert EJ, Luthar N, Bahrar H, Coan JP, Pearson HE, Salgia R, Wheeler DL (2014) Overcoming acquired resistance to cetuximab by dual targeting HER family receptors with antibody-based therapy. Mol Cancer 13(1):242. doi:10.1186/1476-4598-13-242
Sergina NV, Rausch M, Wang D, Blair J, Hann B, Shokat KM, Moasser MM (2007) Escape from HER-family tyrosine kinase inhibitor therapy by the kinase-inactive HER3. Nature 445(7126):437–441. doi:10.1038/nature05474
Tanner B, Hasenclever D, Stern K, Schormann W, Bezler M, Hermes M, Brulport M, Bauer A, Schiffer IB, Gebhard S, Schmidt M, Steiner E, Sehouli J, Edelmann J, Lauter J, Lessig R, Krishnamurthi K, Ullrich A, Hengstler JG (2006) ErbB-3 predicts survival in ovarian cancer. J Clin Oncol 24(26):4317–4323. doi:10.1200/jco.2005.04.8397
Ekberg T, Nestor M, Engstrom M, Nordgren H, Wester K, Carlsson J, Anniko M (2005) Expression of EGFR, HER2, HER3, and HER4 in metastatic squamous cell carcinomas of the oral cavity and base of tongue. Int J Oncol 26(5):1177–1185
Gespach C (2012) Increasing potential of HER3 signaling in colon cancer progression and therapy. Clin Cancer Res 18(4):917–919. doi:10.1158/1078-0432.ccr-11-3143
Wheeler DL, Huang S, Kruser TJ, Nechrebecki MM, Armstrong EA, Benavente S, Gondi V, Hsu KT, Harari PM (2008) Mechanisms of acquired resistance to cetuximab: role of HER (ErbB) family members. Oncogene 27(28):3944–3956. doi:10.1038/onc.2008.19
Huang S, Li C, Armstrong EA, Peet CR, Saker J, Amler LC, Sliwkowski MX, Harari PM (2013) Dual targeting of EGFR and HER3 with MEHD7945A overcomes acquired resistance to EGFR inhibitors and radiation. Cancer Res 73(2):824–833. doi:10.1158/0008-5472.can-12-1611
Hsu FD, Nielsen TO, Alkushi A, Dupuis B, Huntsman D, Liu CL, van de Rijn M, Gilks CB (2002) Tissue microarrays are an effective quality assurance tool for diagnostic immunohistochemistry. Mod Pathol 15(12):1374–1380. doi:10.1097/01.mp.0000039571.02827.ce
Voduc D, Kenney C, Nielsen TO (2008) Tissue microarrays in clinical oncology. Semin Radiat Oncol 18(2):89–97. doi:10.1016/j.semradonc.2007.10.006
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI14C1813).
Conflict of interest
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table S1
Demographic characteristics of patients (DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Seo, A.N., Kwak, Y., Kim, W.H. et al. HER3 protein expression in relation to HER2 positivity in patients with primary colorectal cancer: clinical relevance and prognostic value. Virchows Arch 466, 645–654 (2015). https://doi.org/10.1007/s00428-015-1747-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-015-1747-2