Abstract
Objectives
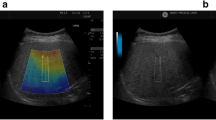
To prospectively assess the role of the US attenuation imaging coefficient (AC) for the diagnosis and quantification of hepatic steatosis.
Methods
One hundred and one patients underwent liver biopsy and US-AC measurement on the same day. Liver steatosis was graded according to biopsy as absent (S0 < 5%), mild (S1 5–33%), moderate (S2 33–66%), or severe (S3 > 66%); liver fibrosis was graded from F0 to F4. The correlation between AC and steatosis on pathology (%) was calculated using the Pearson correlation coefficient. The Student t or Mann–Whitney U test was used to compare continuous variables and ROC curve analysis was used to assess diagnostic performance of AC in diagnosing steatosis.
Results
Overall, 43 (42%), 35 (35%), 12 (12%), and 11 (11%) patients were classified as S0, S1, S2, and S3, respectively. The AC was positively correlated with steatosis as a continuous variable (%) on pathology (r = 0.58, p < 0.01). Patients with steatosis of any grade had a higher AC than those without steatosis (mean 0.77 ± 0.13 vs. 0.63 ± 0.09 dB/cm/MHz, respectively; p < 0.01, AUROC = 0.805). Patients with S2–S3 had a higher AC than patients with S0–1 (0.85 ± 0.11 vs. 0.67 ± 0.11 dB/cm/MHz, respectively; p < 0.01, AUROC = 0.892). AC > 0.69 dB/cm/MHz had a sensitivity and specificity of 76% and 86%, respectively, for diagnosing any grade of steatosis (S1–S3), and AC > 0.72 dB/cm/MHz had a sensitivity and specificity of 96% and 74%, respectively, for diagnosing S2–S3. The presence of advanced fibrosis (F3–F4) did not affect the calculated AC.
Conclusions
The attenuation imaging coefficient is a promising quantitative technique for the non-invasive diagnosis and quantification of hepatic steatosis.
Key Points
• Measurement of the attenuation coefficient is achieved with a very high rate of technical success.
• We found a significant positive correlation between the attenuation coefficient and the grade of steatosis on pathology.
• The attenuation imaging coefficient is a promising quantitative technique for the noninvasive diagnosis and quantification of hepatic steatosis.





Similar content being viewed by others
Abbreviations
- AC:
-
Attenuation coefficient
- ATI:
-
Attenuation imaging
- CAP:
-
Controlled attenuation parameter
- EASL:
-
European Association for the Study of the Liver
- NAFLD:
-
Non-alcoholic fatty liver disease
References
European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO) (2016) EASLEASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 64:1388–1402
Browning JD, Szczepaniak LS, Dobbins R et al (2004) Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 40:1387–1395
Vernon G, Baranova A, Younossi ZM (2011) Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 34:274–285
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M (2016) Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64:73–84
Bellentani S, Bedogni G, Miglioli L, Tiribelli C (2004) The epidemiology of fatty liver. Eur J Gastroenterol Hepatol 16:1087–1093
Ballestri S, Zona S, Targher G et al (2016) Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol 31:936–944
Adinolfi LE, Gambardella M, Andreana A, Tripodi MF, Utili R, Ruggiero G (2001) Steatosis accelerates the progression of liver damage of chronic hepatitis C patients and correlates with specific HCV genotype and visceral obesity. Hepatology 33:1358–1364
McCormack L, Petrowsky H, Jochum W, Furrer K, Clavien PA (2007) Hepatic steatosis is a risk factor for postoperative complications after major hepatectomy: a matched case-control study. Ann Surg 245:923–930
d’Assignies G, Fayard C, Leitao H et al (2016) Liver steatosis assessed by preoperative MRI: an independent risk factor for severe complications after major hepatic resection. Surgery 159:1050–1057
Koneru B, Dikdan G (2002) Hepatic steatosis and liver transplantation current clinical and experimental perspectives. Transplantation 73:325–330
Palmentieri B, de Sio I, La Mura V et al (2006) The role of bright liver echo pattern on ultrasound B-mode examination in the diagnosis of liver steatosis. Dig Liver Dis 38:485–489
Bohte AE, van Werven JR, Bipat S, Stoker J (2011) The diagnostic accuracy of US, CT, MRI and 1H-MRS for the evaluation of hepatic steatosis compared with liver biopsy: a meta-analysis. Eur Radiol 21:87–97
Sasso M, Beaugrand M, de Ledinghen V et al (2010) Controlled attenuation parameter (CAP): a novel VCTE guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol 36:1825–1835
de Ledinghen V, Vergniol J, Capdepont M et al (2014) Controlled attenuation parameter (CAP) for the diagnosis of steatosis: a prospective study of 5323 examinations. J Hepatol 60:1026–1031
Tada T, Kumada T, Toyoda H et al (2019) Utility of attenuation coefficient measurement using an ultrasound-guided attenuation parameter for evaluation of hepatic steatosis: comparison with MRI-determined proton density fat fraction. AJR Am J Roentgenol 212:332–341
Bae JS, Lee DH, Lee JY et al (2019) Assessment of hepatic steatosis by using attenuation imaging: a quantitative, easy-to-perform ultrasound technique. Eur Radiol. https://doi.org/10.1007/s00330-019-06272-y
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR (1999) Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 94:2467–2474
Bedossa P, Dargere D, Paradis V (2003) Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology 38:1449–1457
Hamaguchi M, Kojima T, Itoh Y et al (2007) The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol 102:2708–2715
Ballestri S, Lonardo A, Romagnoli D et al (2012) Ultrasonographic fatty liver indicator, a novel score which rules out NASH and is correlated with metabolic parameters in NAFLD. Liver Int 32:1242–1252
Fishbein M, Castro F, Cheruku S et al (2005) Hepatic MRI for fat quantitation: its relationship to fat morphology, diagnosis, and ultrasound. J Clin Gastroenterol 39:619–625
Stern C, Castera L (2017) Non-invasive diagnosis of hepatic steatosis. Hepatol Int 11:70–78
Strauss S, Gavish E, Gottlieb P, Katsnelson L (2007) Interobserver and intraobserver variability in the sonographic assessment of fatty liver. AJR Am J Roentgenol 189:W320–W323
Friedrich-Rust M, Ong MF, Martens S et al (2008) Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology 134:960–974
Suh CH, Kim SY, Kim KW et al (2014) Determination of normal hepatic elasticity by using real-time shear-wave elastography. Radiology 271:895–900
Karlas T, Petroff D, Sasso M et al (2017) Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol 66:1022–1030
Shi KQ, Tang JZ, Zhu XL et al (2014) Controlled attenuation parameter for the detection of steatosis severity in chronic liver disease: a meta-analysis of diagnostic accuracy. J Gastroenterol Hepatol 29:1149–1158
Ratziu V, Charlotte F, Heurtier A et al (2005) Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology 128:1898–1906
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Marco Dioguardi Burgio.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Methodology
• prospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 7880 kb)
Rights and permissions
About this article
Cite this article
Dioguardi Burgio, M., Ronot, M., Reizine, E. et al. Quantification of hepatic steatosis with ultrasound: promising role of attenuation imaging coefficient in a biopsy-proven cohort. Eur Radiol 30, 2293–2301 (2020). https://doi.org/10.1007/s00330-019-06480-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06480-6