Abstract
Background
The aim of this study was to examine the relation between periampullary diverticula (PAD) and biliary tract stones.
Methods
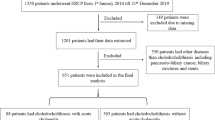
A total of 732 cases of patients with PAD identified from among 6,221 patients who underwent endoscopic retrograde cholangiopancreatography were compared to 750 controls (without PAD) in terms of biliary stone formation, incidence of sphincter of Oddi dysfunction (SOD), and choledocholithiasis. The biliary tract diseases were diagnosed based on medical history, clinical symptoms and signs, and imaging findings using ultrasonography, computed tomography, or magnetic resonance cholangiopancreatography.
Results
The PAD group contained a significantly larger number of patients with biliary stones including stones in the primary common bile duct, SOD with bile duct stones (p < 0.05), and choledocholithiasis after cholecystectomy (p < 0.01).
Conclusions
There is a close correlation between PAD and the formation of biliary tract stones. A particularly close correlation was found between PAD and choledocholithiasis after cholecystectomy. PAD may be an important risk factor for the occurrence or recurrence of biliary tract stones.
Similar content being viewed by others
References
Lobo DN, Balfour TW, Iftikhar SY et al (1999) Periampullary diverticula and pancreaticobiliary disease. Br J Surg 86:588–597
Vaira D, Owsett JF, Hatfield ARW et al (1989) Is duodenal diverticulum a risk factor for sphincterotomy? Cut 30:939–942
Egawa N, Damisawa T, Tu Y et al (1998) The role of juxtapapillary duodenal diverticulum in the formation of gallbladder stones. Hepatogastroenterology 45:917–920
Miyazawa Y, Okinaga K, Nishida K et al (1995) Recurrent common bile duct stones associated with periampullary duodenal diverticula and calcium bilirubinate stones. Int Surg 80:120–124
Mackenzie ME, Davies WT, Farnel MB et al (1996) Risk of recurrent biliary tract disease after cholecystectomy in patients with duodenal diverticula. Arch Surg 131:1083–1085
Perissat J, Huibregtse K, Keane FBV et al (1994) Management of bile duct stones in the era of laparoscopic cholecystectomy. Br J Surg 81:799–810
Boender J, Nix GAJJ, de Ridder MAJ et al (1994) Endoscopic papillotomy for common bile duct stones: factors influencing the complication rate. Endoscopy 26:209–216
Kimura W, Nagai H, Kuroda A et al (1992) No significant correlation between histological changes of the papilla of Vater and juxtapapillary diverticulum: special reference to the pathogenesis of gallstones. Scand J Gastroenterol 27:951–956
Novacek G, Walgram M, Bauer P et al (1997) The relationship between juxtapapillary duodenal diverticula and biliary stone disease. Eur J Gastroenterol Hepatol 9:375–379
Lobo DN, Balfour TW, Iftikhar SY (1998) Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl 80:326–331
Kim MH, Myung SJ, Seo DW et al (1998) Association of periampullary diverticula with primary choledocholithiasis but not with secondary choledocholithiasis. Endoscopy 30:601–604
Wu SD, Su Y, Fan Y et al (2007) Relationship between intraduodenal periampullary diverticulum and biliary disease in 178 patients undergoing ERCP. Hepatobiliary Pancreat Dis Int 6:299–302
Psathakis D, Utschakowski A, Muller G et al (1994) Clinical significance of duodenal diverticula. J Am Coll Surg 178:257–260
Tzeng JJ, Lai KH, Peng NJ et al (2005) Influence of juxtapapillary diverticulum on hepatic clearance in patients after endoscopic sphincterotomy. J Gastroenterol Hepatol 20:772–776
Suda K, Mizuguchi K, Matsumoto M (1983) A histopathological study on the etiology of duodenal diverticulum related to the fusion of the pancreatic anlage. Am J Gastroenterol 78:335–338
Egawa N, Anjiki H, Takuma K et al (2010) Juxtapapillary duodenal diverticula and pancreatobiliary disease. Dig Surg 27:105–109
Kubota Y, Yamaguchi T, Tani K et al (1993) Anatomical variation of pancreaticobiliary ducts in biliary stone diseases. Abdom Imaging 18:145–149
Skar V, Skar AG, Bratlie J et al (1989) Beta-glucuronidase activity in the bile of gallstone patients both with and without duodenal diverticula. Scand J Gastroenterol 24:205–212
Skar V, Skar AG, Osnes M (1989) The duodenal bacterial flora in the region of papilla of Vater in patients with and without duodenal diverticula. Scand J Gastroenterol 24:649–656
Shinagawa N, Fukui T, Maohita K (1991) The relationship between juxtapapillary duodenal diverticula and the presence of bacteria in the bile. Jpn J Surg 21:284–291
Løtveit T, Osnes M, Aune S et al (1980) Studies of the choledochoduodenal sphincter in patients with and without juxta-papillary duodenal diverticula. Scand J Gastroenterol 15:875–880
Miyazaki S, Sakamoto T, Miyata M et al (1995) Function of the sphincter of Oddi in patients with juxtapapillary duodenal diverticula: evaluation by intraoperative biliary manometry under a duodenal pressure load. World J Surg 19:307–312. doi:10.1007/BF00308647
Tanaka M (2002) Advances in research and clinical practice in motor disorders of the sphincter of Oddi. J Hepatobiliary Pancreat Surg 9:564–568
Evans PR, Bak YT, Dowsett JF et al (1997) Small bowel dysmotility in patients with postcholecystectomy sphincter of Oddi dysfunction. Dig Dis Sci 42:1507–1512
Evans PR, Dowsett JF, Bak YT et al (1995) Abnormal sphincter of Oddi response to cholecystokinin in postcholecystectomy syndrome patients with irritable bowel syndrome: the irritable sphincter. Dig Dis Sci 40:1149–1156
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, X., Zhu, K., Zhang, L. et al. Periampullary Diverticulum May Be an Important Factor for the Occurrence and Recurrence of Bile Duct Stones. World J Surg 36, 2666–2669 (2012). https://doi.org/10.1007/s00268-012-1716-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1716-8