Abstract
Purpose
Determine the sensitivity, specificity and accuracy of unenhanced and enhanced MRI in diagnosing scaphoid proximal pole (PP) avascular necrosis (AVN) and correlate whether MRI can help guide the selection of a vascularized or nonvascularized bone graft.
Methods
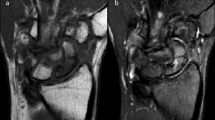
The study was approved by the IRB. Two MSK radiologists independently performed a retrospective review of unenhanced and enhanced MRIs from 18 patients (16 males, 2 females; median age, 17.5 years) with scaphoid nonunions and surgery performed within 65 days of the MRI. AVN was diagnosed on the unenhanced MRI when a diffusely decreased T1-W signal was present in the PP and on the enhanced MRI when PP enhancement was less than distal pole enhancement. Surgical absence of PP bleeding was diagnostic of PP AVN. Postoperative osseous union (OU) was assessed with computed tomography and/or radiographs.
Results
Sensitivity, specificity and accuracy for PP AVN were 71, 82 and 78 % for unenhanced and 43, 82 and 67 % for enhanced MRI. Patients with PP AVN on unenhanced MRI had 86 % (6/7) OU; 100 % (5/5) OU with vascularized bone grafts and 50 % (1/2) OU with nonvascularized grafts. Patients with PP AVN on enhanced MRI had 80 % (4/5) OU; 100 % (3/3) OU with vascularized bone grafts and 50 % (1/2) OU with nonvascularized grafts. Patients with viable PP on unenhanced and enhanced MRI had 91 % (10/11) and 92 % (12/13) OU, respectively, all but one with nonvascularized graft.
Conclusions
When PP AVN is evident on MRI, OU is best achieved with vascularized grafts. If PP AVN is absent, OU is successful with nonvascularized grafts.





Similar content being viewed by others
References
Barton NJ. The late consequences of scaphoid fractures. J Bone Joint Surg (Br). 2004;86-B:626–30.
Adams JE, Steinmann SP. Acute scaphoid fractures. Orthop Clin N Am. 2007;38:229–35.
Morgan WJ, Breen TF, Coumas JM, Schulz LA. Role of magnetic resonance imaging in assessing factors affecting healing in scaphoid nonunions. Clin Orthop Relat Res. 1997;336:240–6.
Ciprian S, Iochum S, Kohlmann R, Dautel G, Dap F, Blum A. MR imaging accuracy in the prediction of bone graft healing potential in scaphoid non-union. J Radiol. 2004;85:1699–706.
Gunal I, Ozcelik A, Gukturk E, Ada S, Demirtas M. Correlation of magnetic resonance imaging and intraoperative punctate bleeding to assess the vascularity of scaphoid nonunion. Arch Orthop Trauma Surg. 1999;119:285–7.
Perlik PC, Guilford WB. Magnetic resonance imaging to assess vascularity of scaphoid nonunions. J Hand Surg [Am]. 1991;16A(3):479–84.
Sakuma M, Nakamura R, Imaeda T. Analysis of proximal fragment sclerosis and surgical outcome of scaphoid non-union by magnetic resonance imaging. J Hand Surg (Br). 1995;20B(2):201–5.
Trumble TE. Avascular necrosis after scaphoid fracture: a correlation of magnetic resonance imaging and histology. J Hand Surg [Am]. 1990;15A(4):557–64.
Desser TS, McCarthy S, Trumble TE. Scaphoid fractures and Kienbock’s disease of the lunate: MR imaging with histopathologic correlation. Magn Reson Imaging. 1990;8:357–61.
Fox MG, Gaskin CM, Chhabra AB, Anderson MW. Assessment of scaphoid viability with MRI: a reassessment of findings on unenhanced MR images. Am J Roentgenol. 2010;195:W281–6.
Cerezal L, Abascal F, Canga A, Garcia-Valtuille R, Bustamante M, del Pinal F. Usefulness of gadolinium enhanced MR imaging in the evaluation of the vascularity of scaphoid nonunions. Am J Roentgenol. 2000;174:141–9.
Singh AK, Davis TRC, Dawson JS, Oni JA, Downing ND. Gadolinium enhanced MR assessment of proximal fragment vascularity in nonunions after scaphoid fracture: does it predict the outcome of reconstructive surgery? J Hand Surg (Br). 2004;29B(5):444–8.
Donati OF, Zanetti M, Nagy L, Bode B, Schweizer A, Pfirrmann CWA. Is dynamic gadolinium enhancement needed in MR imaging for the preoperative assessment of scaphoidal viability in patients with scaphoid nonunion? Radiology. 2011;260(3):808–16.
Anderson SE, Steinbach LS, Tschering-Vogel D, Martin M, Nagy L. MR imaging of avascular scaphoid nonunion before and after vascularized bone grafting. Skelet Radiol. 2005;34:314–20.
Ciprian S, Iochum S, Kohlmann R, Dautel G, Dap F, Blum A. MR imaging accuracy in the prediction of bone graft healing potential in scaphoid non-union. J Radiol. 2004;85(10 Pt 1):1699–706. French.
Dailiana ZH, Zachos V, Varitimidis S, Papanagiotou P, Karantanas A, Malizos KN. Scaphoid nonunions treated with vascularised bone grafts: MRI assessment. Eur J Radiol. 2004;50(3):217–24.
Imaeda T, Nakamura R, Miura T, Makino N. Magnetic resonance imaging in scaphoid fractures. J Hand Surg (Br). 1992;17-B:20–7.
Sebag G, Ducou Le Pointe H, Klein I, et al. Dynamic gadolinium-enhanced subtraction MR imaging: a simple technique for the early diagnosis of Legg-Calvé-Perthes disease: preliminary results. Pediatr Radiol. 1997;27(3):216–20.
Sakai T, Sugano N, Nishii T, Haraguchi K, Ochi T, Ohzono K. MR findings of necrotic lesions and the extralesional area of osteonecrosis of the femoral head. Skelet Radiol. 2000;29(3):133–41.
Dawson JS, Martel AL, Davis TRC. Scaphoid blood flow and acute fracture healing. A dynamic MRI study with enhancement with gadolinium. J Bone Joint Surg (Br). 2001;83-B:809–14.
Verstraete KL, De Deene Y, Roels H, Dierick A, Uyttendaele D, Kunnen M. Benign and malignant musculoskeletal lesions: dynamic contrast-enhanced MR imaging—parametric “first-pass” images depict tissue vascularization and perfusion. Radiology. 1994;192(3):835–43.
Conflict of interest
The authors declare that they have no conflict of interest, grants or financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fox, M.G., Wang, D.T. & Chhabra, A.B. Accuracy of enhanced and unenhanced MRI in diagnosing scaphoid proximal pole avascular necrosis and predicting surgical outcome. Skeletal Radiol 44, 1671–1678 (2015). https://doi.org/10.1007/s00256-015-2221-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2221-6