Abstract
Background
The onset of Crohn disease (CD) can occur in childhood. Imaging, which often involves radiation, is frequent in CD both for disease diagnosis and follow-up. However, information regarding radiation dose for contemporary CT and fluoroscopy is not available for determining the cost/benefit ratio for imaging strategies.
Objective
To compare effective dose (ED) for small-bowel follow-through (SBFT) and abdomen/pelvis MDCT in pediatric CD.
Materials and methods
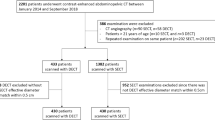
Average fluoroscopic time and number of radiographs were obtained for 30 consecutive pediatric SBFTs. The numbers of SBFTs and CT scans performed per child among children with CD (1990–2005) were determined. The ED was determined (ICRP 60, 10-year-old phantom, MOSFET) for a 5-min fluoroscopy examination of the central abdomen and right lower quadrant (110 kVp, 0.3 mA) and pelvis (110 kVp, 0.35 mA). The ED for a 16-slice abdomen/pelvis MDCT scan was determined using the 10-year-old protocol: 16×1.25 mm, pitch 1.375, 27.5 mm/rotation, 0.5 s, 140 kVp, 85 mA.
Results
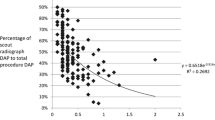
A total of 176 children with CD underwent imaging, averaging 1.2 SBFTs and 1.1 CT scans. On average SBFT took 5.1 min with 3.3 abdominal radiographs. The EDs (mSv) for a 5-min fluoroscopy were 0.15 for the central abdomen, 0.35 for the right lower quadrant, and 0.56 for the pelvis, yielding an average ED for SBFT (5-min fluoroscopy, 3.3 abdominal radiographs) of 1.8–2.2 mSv. The ED for MDCT was 3.48 mSv.
Conclusion
Although the ED for MDCT might be up to twice that for SBFT, excessive fluoroscopy time and number of abdominal radiographs can result in actual EDs that are equivalent. Attention must be paid to SBFT technique to minimize radiation dose and to the indication to determine the appropriate examination.


Similar content being viewed by others
References
Rose JD, Roberts GM, Williams G et al (1988) Cardiff Crohn’s disease jubilee: the incidence over 50 years. Gut 29:346–351
Heyman MB, Kirschner BS, Gold BD et al (2005) Children with early-onset inflammatory bowel disease (IBD): analysis of a pediatric IBD consortium registry. J Pediatr 146:35–40
Baldassano RN, Piccoli DA (1999) Inflammatory bowel disease in pediatric and adolescent patients. Gastroenterol Clin North Am 28:445–458
Sawczenko A, Sandhu BK (2003) Presenting features of inflammatory bowel disease in Great Britain and Ireland. Arch Dis Child 88:995–1000
Jess T, Gamborg M, Matzen P et al (2005) Increased risk of intestinal cancer in Crohn’s disease: a meta-analysis of population-based cohort studies. Am J Gastroenterol 100:2724–2729
Kandiel A, Fraser AG, Korelitz BI et al (2005) Increased risk of lymphoma among inflammatory bowel disease patients treated with azathioprine and 6-mercaptopurine. Gut 54:1121–1125
Rosh JR, Gross T, Mamula P et al (2007) Hepatosplenic T-cell lymphoma in adolescents and young adults with Crohn’s disease: a cautionary tale? Inflamm Bowel Dis 13:1024–1030
Brenner D, Elliston C, Hall E et al (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR 176:289–296
Vock P (2005) CT dose reduction in children. Eur Radiol 15:2330–2340
Hall EJ (2002) Lessons we have learned from our children: cancer risks from diagnostic radiology. Pediatr Radiol 32:700–706
Gubatova D, Varchenya V, Kristinya V (1989) Tissue equivalent phantoms in radiological protection. Kernenergie 32:10–13
CIRS (2007) Handling Instruction Manual, Atom Pediatric Ten Year Old Phantom. CIRS, Norfolk, VA
Best Medical Canada (2007) Datasheets/publications. http://www.thomson-elec.com Accessed 4 October 2006
Frush DP, Donnelly LF, Rosen NS (2003) Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics 112:951–957
Wall BF, Hart D (1997) Revised radiation doses for typical X-ray examinations. Report on a recent review of doses to patients from medical X-ray examinations in the UK by NRPB. National Radiological Protection Board. Br J Radiol 70:437–439
Gorson RO, Lassen M, Rosenstein M (1984) Patient dosimetry in diagnostic radiology. Handbook of medical physics, vol II. CRC Press, Boca Raton, pp 467–526
NCRP (1989) Exposure of the U.S. Population from Diagnostic Medical Radiation: Report no. 100. NCRP, Bethesda, MD
Mettler FA Jr, Wiest PW, Locken JA et al (2000) CT scanning: patterns of use and dose. J Radiol Prot 20:353–359
Donnelly LF (2005) Reducing radiation dose associated with pediatric CT by decreasing unnecessary examinations. AJR 184:655–657
Jabra AA, Fishman EK, Taylor GA (1991) Crohn disease in the pediatric patient: CT evaluation. Radiology 179:495–498
Jabra AA, Fishman EK, Taylor GA (1994) CT findings in inflammatory bowel disease in children. AJR 162:975–979
Jamieson DH, Shipman PJ, Israel DM et al (2003) Comparison of multidetector CT and barium studies of the small bowel: inflammatory bowel disease in children. AJR 180:1211–1216
Morgan HT (2002) Dose reduction for CT pediatric imaging. Pediatr Radiol 32:724–728; discussion 751–754
Huda W, Vance A (2007) Patient radiation doses from adult and pediatric CT. AJR 188:540–546
Darbari A, Sena L, Argani P et al (2004) Gadolinium-enhanced magnetic resonance imaging: a useful radiological tool in diagnosing pediatric IBD. Inflamm Bowel Dis 10:67–72
Durno CA, Sherman P, Williams T et al (2000) Magnetic resonance imaging to distinguish the type and severity of pediatric inflammatory bowel diseases. J Pediatr Gastroenterol Nutr 30:170–174
Ott DJ, Chen YM, Gelfand DW et al (1985) Detailed per-oral small bowel examination vs. enteroclysis. Part I: Expenditures and radiation exposure. Radiology 155:29–31
Thoeni RF, Gould RG (1991) Enteroclysis and small bowel series: comparison of radiation dose and examination time. Radiology 178:659–662
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gaca, A.M., Jaffe, T.A., Delaney, S. et al. Radiation doses from small-bowel follow-through and abdomen/pelvis MDCT in pediatric Crohn disease. Pediatr Radiol 38, 285–291 (2008). https://doi.org/10.1007/s00247-007-0702-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0702-z