Abstract
Rationale
Increased activity of the hypothalamic–pituitary–adrenal (HPA) axis is an important aspect of the pathophysiology of major depression and schizophrenia. Despite the usefulness of atypical antipsychotics in the treatment of depression and their positive influence on cognitive functioning possibly related to their impact on cortisol, little is known about their effect on HPA axis function.
Objective
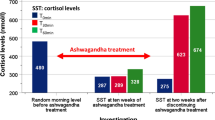
Therefore, this double-blind, placebo-controlled, randomized cross-over study investigated the influence of the atypical antipsychotics quetiapine and olanzapine in comparison with haloperidol and placebo on plasma adrenocorticotropic hormone (ACTH), cortisol, and prolactin levels. Eleven healthy male volunteers were studied during four sessions one week apart, orally receiving placebo, quetiapine (50 mg), olanzapine (5 mg), or haloperidol (3 mg). Blood samples were taken at hourly intervals from 0900 until 1700 hours. For ACTH, cortisol, and prolactin a significant effect of treatment condition (p≤0.005; p≤0.035; p≤0.0001, respectively) for area under the curve (AUC) was found. In comparison to placebo, quetiapine and olanzapine significantly reduced ACTH (p≤0.002; p≤0.05, respectively) and cortisol (p≤0.005; p≤0.03, respectively). No effect of haloperidol on AUC of ACTH or cortisol levels was observed. In comparison with placebo, haloperidol (p≤0.0001) and olanzapine (p≤0.0001) elevated AUC of prolactin plasma levels, whereas no significant effect was observed for quetiapine as a main effect of treatment condition. The atypical antipsychotics’ strong influence on HPA-function with pronounced ACTH and cortisol lowering is possibly related to the atypicals’ blockade of serotonergic receptors, but blockade of adrenergic or histaminergic receptors may play a role as well. The observed HPA-axis down-regulation may be clinically important for the atypicals’ effects on depressive symptomatology and cognitive functioning.

Similar content being viewed by others
References
Abi Saab W, Seibyl JP, D’Souza DC, Karper LP, Gueorgueva R, Abi Dargham A, Wong ML, Rajhans S, Erdos JP, Heninger GR, Charney DS, Krystal JH (2002) Ritanserin antagonism of m-chlorophenylpiperazine effects in neuroleptic-free schizophrenics patients: support for serotonin-2 receptor modulation of schizophrenia symptoms. Psychopharmacology (Berl) 162:55–62
Adityanjee, Schulz SC (2002) Clinical use of quetiapine in disease states other than schizophrenia. J Clin Psychiatry 63:32–38
al Damluji S (1993) Adrenergic control of the secretion of anterior pituitary hormones. Baillieres. Clin Endocrinol Metab 7:355–392
Alexiadis M, Whitehorn D, Woodley H, Kopala L (2002) Prolactin elevation with quetiapine. Am J Psychiatry 159:1608–1609
Allolio B, Deuss U, Kaulen D, Winkelmann W (1983) Effect of meclastine, a selective H1 receptor antagonist, upon ACTH release. Clin Endocrinol (Oxf) 19:239–245
Allolio B, Schulte HM, Deuss U, Winkelmann W (1987) Cyproheptadine inhibits the corticotropin releasing hormone (CRH)—induced hormone release in normal subjects. Horm Metab Res Suppl 16:36–38
Altamura AC, Boin F, Maes M (1999) HPA axis and cytokines dysregulation in schizophrenia: potential implications for the antipsychotic treatment. Eur Neuropsychopharmacol 10:1–4
Baptista T, Alastre T, Contreras Q, Martinez JL, Araujo de Baptista E, Paez X, Hernandez L (1997a) Effects of the antipsychotic drug sulpiride on reproductive hormones in healthy men: relationship with body weight regulation. Pharmacopsychiatry 30:250–255
Baptista T, Molina MG, Martinez JL, de Quijada M, Calanche de Cuesta I, Acosta A, Paez X, Martinez JM, Hernandez L (1997b) Effects of the antipsychotic drug sulpiride on reproductive hormones in healthy premenopausal women: relationship with body weight regulation. Pharmacopsychiatry 30:256–262
Barbieri C, Parodi M, Bruno S, Bertassi F, Benaglia D, Moser P, Meroni R, Dubini A (1984) Effects of acute administration of zetidoline, a new antidopaminergic drug, on plasma prolactin and aldosterone levels in man. Eur J Clin Pharmacol 26:29–32
Belanoff JK, Gross K, Yager A, Schatzberg AF (2001) Corticosteroids and cognition. J Psychiatr Res 35:127–145
Bilder RM, Goldman RS, Volavka J, Czobor P, Hoptman M, Sheitman B, Lindenmayer JP, Citrome L, McEvoy J, Kunz M, Chakos M, Cooper TB, Horowitz TL, Lieberman JA (2002) Neurocognitive effects of clozapine, olanzapine, risperidone, and haloperidol in patients with chronic schizophrenia or schizoaffective disorder. Am J Psychiatry 159:1018–1028
Borison RL, Arvanitis LA, Miller BG (1996) ICI 204,636, an atypical antipsychotic: efficacy and safety in a multicenter, placebo-controlled trial in patients with schizophrenia. US SEROQUEL Study Group J Clin Psychopharmacol 16:158–169
Breier A, Buchanan RW, Waltrip RW 2nd, Listwak S, Holmes C, Goldstein DS (1994) The effect of clozapine on plasma norepinephrine: relationship to clinical efficacy. Neuropsychopharmacology 10:1–7
Brown ES, Varghese FP, McEwen BS (2004) Association of depression with medical illness: does cortisol play a role? Biol Psychiatry 55:1–9
Calabrese JR, Macfadden W, McCoy R, Minkwitz M, Wilson E, Mullen J (2004) Double-blind, placebo-controlled study of quetiapine in bipolar depression. In: Association AP (ed) American psychiatric association 157th annual meeting. American Psychiatric Association, New York, USA, p 284, NR756
Cohrs S, Pohlmann K, Guan Z, Jordan W, Meier A, Huether G, Rüther E, Rodenbeck A (2004) Quetiapine reduces nocturnal urinary cortisol excretion in healthy subjects. Psychopharmacology (Berl) 174:414–420
Collu R, Jequier JC, Leboeuf G, Letarte J, Ducharme JR (1975) Endocrine effects of pimozide, a specific dopaminergic blocker. J Clin Endocrinol Metab 41:981–984
Contesse V, Lefebvre H, Lenglet S, Kuhn JM, Delarue C, Vaudry H (2000) Role of 5-HT in the regulation of the brain–pituitary–adrenal axis: effects of 5-HT on adrenocortical cells. Can J Physiol Pharmacol 78:967–983
de Koning P, de Vries MH (1995) A comparison of the neuro-endocrinological and temperature effects of DU 29894, flesinoxan, sulpiride and haloperidol in normal volunteers. Br J Clin Pharmacol 39:7–14
Fuller RW, Snoddy HD (1984) Central dopamine receptors mediating pergolide-induced elevation of serum corticosterone in rats. Characterization by the use of antagonists. Neuropharmacology 23:1389–1394
Ghadirian AM, Chouinard G, Annable L (1982) Sexual dysfunction and plasma prolactin levels in neuroleptic-treated schizophrenic outpatients. J Nerv Ment Dis 170:463–467
Goodnick PJ, Rodriguez L, Santana O (2002) Antipsychotics: impact on prolactin levels. Expert Opin Pharmacother 3:1381–1391
Gruen PH, Sachar EJ, Langer G, Altman N, Leifer M, Frantz A, Halpern FS (1978) Prolactin responses to neuroleptics in normal and schizophrenic subjects. Arch Gen Psychiatry 35:108–116
Hamner MB, Arvanitis LA, Miller BG, Link CG, Hong WW (1996) Plasma prolactin in schizophrenia subjects treated with Seroquel (ICI 204,636). Psychopharmacol Bull 32:107–110
Harrow M, Yonan CA, Sands JR, Marengo J (1994) Depression in schizophrenia: are neuroleptics, akinesia, or anhedonia involved? Schizophr Bull 20:327–338
Hatzimanolis J, Lykouras L, Markianos M, Oulis P (1998) Neurochemical variables in schizophrenic patients during switching from neuroleptics to clozapine. Prog Neuro-Psychopharmacol Biol Psychiatry 22:1077–1085
Hennig J, Rzepka U, Mai B, Netter P (1995) Suppression of HPA-axis activity by haloperidol after experimentally induced heat stress. Prog Neuro-Psychopharmacol Biol Psychiatry 19:603–614
Holsboer F (2000) The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology 23:477–501
Hornig M, Amsterdam JD (2003) Prolactin, growth hormone, insulin, glucagon, and parathyroid hormone. In: Wolkowitz OM, Rothschild AJ (eds) Psychoneuroendocrinology. The Scientific basis of clinical practice. American Psychiatrist Publishing, Arlington, pp 107–136
Jezova Repcekova D, Klimes I, Jurcovicova J, Vigas M (1979) Effect of adrenergic receptor blockade on cortisol and GH response to insulin-induced hypoglycemia in man. Int J Clin Pharmacol Biopharm 17:64–67
Kahn RS, Siever L, Davidson M, Greenwald C, Moore C (1993) Haloperidol and clozapine treatment and their effect on M-chlorophenylpiperazine-mediated responses in schizophrenia: implications for the mechanism of action of clozapine. Psychopharmacology (Berl) 112:S90–S94
Kapur S, Zipursky R, Jones C, Shammi CS, Remington G, Seeman P (2000) A positron emission tomography study of quetiapine in schizophrenia: a preliminary finding of an antipsychotic effect with only transiently high dopamine D2 receptor occupancy. Arch Gen Psychiatry 57:553–559
Laakmann G, Wittmann M, Gugath M, Mueller OA, Treusch J, Wahlster U, Stalla GK (1984) Effects of psychotropic drugs (desimipramine, chlorimipramine, sulpiride and diazepam) on the human HPA axis. Psychopharmacology (Berl) 84:66–70
Laakmann G, Wittmann M, Schoen HW, Zygan K, Weiss A, Meissner R, Mueller OA, Stalla GK (1986) Effects of receptor blockers (methysergide, propranolol, phentolamine, yohimbine and prazosin) on desimipramine-induced pituitary hormone stimulation in humans-III. Hypothalamo–pituitary–adrenocortical axis. Psychoneuroendocrinology 11:475–489
Laakmann G, Schule C, Baghai T, Waldvogel E (1999) Effects of mirtazapine on growth hormone, prolactin, and cortisol secretion in healthy male subjects. Psychoneuroendocrinology 24:769–784
Langer G, Sachar EJ, Gruen PH, Halpern FS (1977) Human prolactin responses to neuroleptic drugs correlate with antischizophrenic potency. Nature 266:639–640
Marco EJ, Wolkowitz OM, Vinogradov S, Poole JH, Lichtmacher J, Reus VI (2002) Double-blind antiglucocorticoid treatment in schizophrenia and schizoaffective disorder: a pilot study. World J Biol Psychiatry 3:156–161
Markianos M, Hatzimanolis J, Lykouras L (1999) Switch from neuroleptics to clozapine does not influence pituitary–gonadal axis hormone levels in male schizophrenic patients. Eur Neuropsychopharmacol 9:533–536
Mauri M, Sinforiani E, Bono G, Vignati F, Berselli ME, Attanasio R, Nappi G (1993) Memory impairment in Cushing’s disease. Acta Neurol Scand 87:52–55
Meltzer HY (1989) Clinical studies on the mechanism of action of clozapine: the dopamine–serotonin hypothesis of schizophrenia. Psychopharmacology (Berl) 99(Suppl):S18–S27
Meltzer HY, Fang VS (1976) The effect of neuroleptics on serum prolactin in schizophrenic patients. Arch Gen Psychiatry 33:279–286
Möller HJ (2003) Management of the negative symptoms of schizophrenia: new treatment options. CNS Drugs 17:793–823
Murburg MM, Paly D, Wilkinson CW, Veith RC, Malas KL, Dorsa DM (1986) Haloperidol increases plasma beta endorphin-like immunoreactivity and cortisol in normal human males. Life Sci 39:373–381
Murburg MM, Wilkinson CW, Raskind MA, Veith RC, Dorsa DM (1993) Evidence for two differentially regulated populations of peripheral beta-endorphin-releasing cells in humans. J Clin Endocrinol Metab 77:1033–1040
Nemeroff CB (1997) Dosing the antipsychotic medication olanzapine. J Clin Psychiatry 58(Suppl 10):45–49
Nurnberger JI Jr, Simmons Alling S, Kessler L, Jimerson S, Schreiber J, Hollander E, Tamminga CA, Nadi NS, Goldstein DS, Gershon ES (1984) Separate mechanisms for behavioral, cardiovascular, and hormonal responses to dextroamphetamine in man. Psychopharmacology (Berl) 84:200–204
Purdon SE, Jones BD, Stip E, Labelle A, Addington D, David SR, Breier A, Tollefson GD (2000) Neuropsychological change in early phase schizophrenia during 12 months of treatment with olanzapine, risperidone, or haloperidol. The Canadian Collaborative Group for research in schizophrenia. Arch Gen Psychiatry 57:249–258
Richelson E, Souder T (2000) Binding of antipsychotic drugs to human brain receptors focus on newer generation compounds. Life Sci 68:29–39
Rubin RT, Poland RE, O’Connor D, Gouin PR, Tower BB (1976) Selective neuroendocrine effects of low-dose haloperidol in normal adult men. Psychopharmacologia 47:135–140
Scheepers FE, Gespen de Wied CC, Kahn RS (2001) The effect of olanzapine treatment on m-chlorophenylpiperazine-induced hormone release in schizophrenia. J Clin Psychopharmacol 21:575–582
Schule C, Baghai T, Zwanzger P, Ella R, Eser D, Padberg F, Moller HJ, Rupprecht R (2003) Attenuation of hypothalamic–pituitary–adrenocortical hyperactivity in depressed patients by mirtazapine. Psychopharmacology (Berl) 166:271–275
Seeman TE, McEwen BS, Singer BH, Albert MS, Rowe JW (1997) Increase in urinary cortisol excretion and memory declines: MacArthur studies of successful aging. J Clin Endocrinol Metab 82:2458–2465
Seibyl JP, Krystal JH, Price LH, Woods SW, D’Amico C, Heninger GR, Charney DS (1991) Effects of ritanserin on the behavioral, neuroendocrine, and cardiovascular responses to meta-chlorophenylpiperazine in healthy human subjects. Psychiatry Res 38:227–236
Shelton RC, Tollefson GD, Tohen M, Stahl S, Gannon KS, Jacobs TG, Buras WR, Bymaster FP, Zhang W, Spencer KA, Feldman PD, Meltzer HY (2001) A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 158:131–134
Shirayama Y, Hashimoto K, Suzuki Y, Higuchi T (2002) Correlation of plasma neurosteroid levels to the severity of negative symptoms in male patients with schizophrenia. Schizophr Res 58:69–74
Sonino N, Fava GA, Fallo F, Franceschetto A, Belluardo P, Boscaro M (2000) Effect of the serotonin antagonists ritanserin and ketanserin in Cushing’s disease. Pituitary 3:55–59
Tohen M, Vieta E, Calabrese J, Ketter TA, Sachs G, Bowden C, Mitchell PB, Centorrino F, Risser R, Baker RW, Evans AR, Beymer K, Dube S, Tollefson GD, Breier A (2003) Efficacy of olanzapine and olanzapine–fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 60:1079–1088
Tuomisto J, Mannisto P (1985) Neurotransmitter regulation of anterior pituitary hormones. Pharmacol Rev 37:249–332
Turrone P, Kapur S, Seeman MV, Flint AJ (2002) Elevation of prolactin levels by atypical antipsychotics. Am J Psychiatry 159:133–135
Velligan DI, Newcomer J, Pultz J, Csernansky J, Hoff AL, Mahurin R, Miller AL (2002) Does cognitive function improve with quetiapine in comparison to haloperidol? Schizophr Res 53:239–248
Volavka J, Czobor P, Cooper TB, Sheitman B, Lindenmayer JP, Citrome L, McEvoy JP, Lieberman JA (2004) Prolactin levels in schizophrenia and schizoaffective disorder patients treated with clozapine, olanzapine, risperidone, or haloperidol. J Clin Psychiatry 65:57–61
von Bahr C, Wiesel FA, Movin G, Eneroth P, Jansson P, Nilsson L, Ogenstad S (1991) Neuroendocrine responses to single oral doses of remoxipride and sulpiride in healthy female and male volunteers. Psychopharmacology (Berl) 103:443–448
Walder DJ, Walker EF, Lewine RJ (2000) Cognitive functioning, cortisol release, and symptom severity in patients with schizophrenia. Biol Psychiatry 48:1121–1132
Weizman A, Maoz B, Treves I, Asher I, Ben David M (1985) Sulpiride-induced hyperprolactinemia and impotence in male psychiatric outpatients. Prog Neuropsychopharmacol Biol Psychiatry 9:193–198
Wetzel H, Wiesner J, Hiemke C, Benkert O (1994) Acute antagonism of dopamine D2-like receptors by amisulpride: effects on hormone secretion in healthy volunteers. J Psychiatr Res 28:461–473
Wetzel H, Szegedi A, Hain C, Wiesner J, Schlegel S, Benkert O (1995) Seroquel (ICI 204 636), a putative “atypical” antipsychotic, in schizophrenia with positive symptomatology: results of an open clinical trial and changes of neuroendocrinological and EEG parameters. Psychopharmacology (Berl) 119:231–238
Wieck A, Haddad PM (2003) Antipsychotic-induced hyperprolactinaemia in women: pathophysiology, severity and consequences. Selective literature review. Br J Psychiatry 182:199–204
Wilcox CS, Aminoff MJ, Millar JG, Keenan J, Kremer M (1975) Circulating levels of corticotrophin and cortisol after infusions of l-DOPA, dopamine and noradrenaline, in man. Clin Endocrinol (Oxf) 4:191–198
Wolkowitz OM, Reus VI (1999) Treatment of depression with antiglucocorticoid drugs. Psychosom Med 61:698–711
Zerssen von D, Koeller DM (1976) Die Beschwerden-Liste (Manual). Klinische Selbstbeurteilungsskalen aus dem Muenchner Psychiatrischen Informationssystem (PSYCHIS). Beltz-Verlag, Beltz-Verlag
Acknowledgements
We are grateful to the dedicated staff of the Sleep Medicine Center of the Department of Psychiatry and Psychotherapy, University of Göttingen, Germany, including Roswitha Bianco, Iris Bossmann, Brigitte Marxen, and Andreas Müller-Struck.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cohrs, S., Röher, C., Jordan, W. et al. The atypical antipsychotics olanzapine and quetiapine, but not haloperidol, reduce ACTH and cortisol secretion in healthy subjects. Psychopharmacology 185, 11–18 (2006). https://doi.org/10.1007/s00213-005-0279-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0279-x