Abstract
Introduction and hypothesis
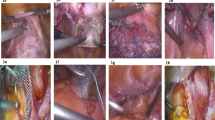
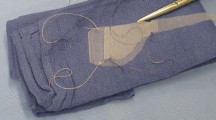
To prospectively evaluate the use of a particular polypropylene Y mesh for robotic sacrocolpopexy.
Methods
This was a prospective study of 120 patients who underwent robotic sacrocolpopexy. We compared preoperative and 12-month postoperative objective and subjective assessments via the Pelvic Organ Prolapse Quantification (POP-Q), the Pelvic Floor Distress Inventory, Short Form 20 (PFDI-20); the Pelvic Floor Impact Questionnaire, Short Form 7 (PFIQ-7); and the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire 12 (PISQ-12). Objective “anatomical success” was defined as POP-Q stage 0 or 1 at all postoperative intervals. We further defined “clinical cure” by simultaneously considering POP-Q points and subjective measures. To be considered a “clinical cure,” a given patient had to have all POP-Q points ≤0, apical POP-Q point C ≤5, no reported pelvic organ prolapse symptoms on the PFDI-20, and no reoperation for prolapse at all postoperative intervals.
Results
Of the 120 patients, 118 patients completed the 1-year follow-up. The objective “anatomical success” rate was 89 % and the “clinical cure” rate was 94 %. The PFDI-20 mean score improved from 100.4 at baseline to 21.0 at 12 months (p < 0.0001); PFIQ-7 scores improved from 61.6 to 8.0 (p < 0.0001); and PISQ-12 scores improved from 35.7 to 38.6 (p < 0.0009). No mesh erosions or mesh-related complications occurred.
Conclusion
The use of this ultra-lightweight Y mesh for sacrocolpopexy, eliminated the mesh-related complications in the first postoperative year, and provided significant improvement in subjective and objective outcomes.
Similar content being viewed by others
References
Lane FE (1962) Repair of posthysterectomy vaginal-vault prolapse. Obstet Gynecol 20:72–77
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM et al (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104:805–823
Culligan PJ, Blackwell L, Goldsmith LJ, Graham CA, Rogers A, Heit MH (2005) A randomized controlled trial comparing fascia lata and synthetic mesh for sacral colpopexy. Obstet Gynecol 106:29–37
Ostergard DR (2010) Polypropylene mesh grafts in gynecology. Obstet Gynecol 116:962–966
U. S. Food and Drug Administration (2008) FDA public health notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. Available at: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm061976.htm Accessed 26 August 2012
U.S. Food and Drug Administration (2011) FDA safety communication: UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. Available at: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm Accessed 26 August 2012
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H (1993) Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health 47:497–499
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193:103–113
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2003) A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct 14:164–168, discussion 168
Murphy M, Sternschuss G, Haff R, van Raalte H, Saltz S, Lucente V (2008) Quality of life and surgical satisfaction after vaginal reconstructive vs obliterative surgery for the treatment of advanced pelvic organ prolapse. Am J Obstet Gynecol 198(5):573.e1–573.e7
Salamon C, Shariati A, Culligan PJ (2010) Optimizing efficiency with robot-assisted laparoscopic sacrocolpopexy. Female Patient 35(4):33–38
Weber AM, Abrams P, Brubaker L, Davis G, Dmochowski RR et al (2001) The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 12:178–186
Brubaker L, Nygaard IE, Richter HE, Visco A, Weber AM, Cundiff G et al (2008) Two-year outcomes after sacrocolpopexy with and without Burch to prevent stress urinary incontinence. Obstet Gynecol 112:49–55
Paraiso MFR, Jelovsek JE, Frick A, Chen CCG, Barber MD (2011) Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse: a randomized controlled trial. Obstet Gynecol 118:1005–1013
Salamon CG, Culligan PJ (2012) Subjective and objective outcomes 1 year after robotic-assisted laparoscopic sacrocolpopexy. J Robotic Surg 88:245–246
Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE (2009) Complication and reoperation rates after apical vaginal prolapse surgical repair a systematic review. Obstet Gynecol 113:367–373
Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES (2011) Prevalence and risk factors for mesh erosion after laparoscopic-assisted sacrocolpopexy. Int Urogynecol J Pelvic Floor Dysfunct 22(2):205–212
Conflict of interest
The study was funded through an unrestricted grant from Coloplast A/S, Humlebæk, Denmark.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salamon, C.G., Lewis, C., Priestley, J. et al. Prospective study of an ultra-lightweight polypropylene Y mesh for robotic sacrocolpopexy. Int Urogynecol J 24, 1371–1375 (2013). https://doi.org/10.1007/s00192-012-2021-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-2021-7