Abstract
Purpose
The association between extracorporeal membrane oxygenation (ECMO) use and the development of thrombocytopenia is widely presumed yet weakly demonstrated. We hypothesized that longer duration of ECMO support would be independently associated with worsened thrombocytopenia.
Methods
We performed a single-center retrospective cohort study of 100 adults who received ECMO for acute respiratory failure. We used generalized estimating equations to test the association between days on ECMO and daily percentage of platelets compared to the first post-cannulation platelet count. We constructed a multivariable logistic regression model with backwards stepwise elimination to identify clinical predictors of severe thrombocytopenia (≤50,000/μL) while on ECMO.
Results
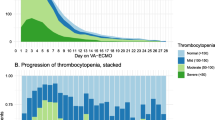
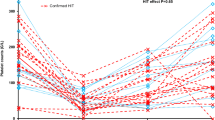
Days on ECMO was not associated with a decrease in platelet count in the unadjusted analysis (β −0.85, 95 % CI −2.05 to 0.36), nor after considering and controlling for days hospitalized prior to ECMO, APACHE II score, platelet transfusions, and potential thrombocytopenia-inducing medications (β −0.83, 95 % CI −1.9 to 0.25). Twenty-two subjects (22 %) developed severe thrombocytopenia. The APACHE II score and platelet count at the time of cannulation predicted the development of severe thrombocytopenia. The odds of developing severe thrombocytopenia increased 35 % for every 5-point increase in APACHE II score (OR 1.35, 95 % CI 0.94–1.94) and increased 35 % for every 25,000/μL platelets below a mean at cannulation of 188,000/μL (OR 1.35, 95 % CI 1.10–1.64).
Conclusions
Duration of ECMO is not associated with the development of thrombocytopenia. The severity of critical illness and platelet count at the time of cannulation predict the development of severe thrombocytopenia while receiving ECMO for respiratory failure. Future studies should validate these findings, especially in cohorts with more venoarterial ECMO patients, and should characterize the association between thrombocytopenia and bleeding events while on ECMO.


Similar content being viewed by others
References
Brodie D, Bacchetta M (2011) Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med 365:1905–1914
Abrams D, Brodie D (2013) Emerging indications for extracorporeal membrane oxygenation in adults with respiratory failure. Ann Am Thorac Soc 10:371–377
Brogan TV, Thiagarajan RR, Rycus PT, Bartlett RH, Bratton SL (2009) Extracorporeal membrane oxygenation in adults with severe respiratory failure: a multi-center database. Intensive Care Med 35:2105–2114
Roch A, Lepaul-Ercole R, Grisoli D, Bessereau J, Brissy O, Castanier M, Dizier S, Forel JM, Guervilly C, Gariboldi V, Collart F, Michelet P, Perrin G, Charrel R, Papazian L (2010) Extracorporeal membrane oxygenation for severe influenza A (H1N1) acute respiratory distress syndrome: a prospective observational comparative study. Intensive Care Med 36:1899–1905
Schmidt M, Tachon G, Devilliers C, Muller G, Hekimian G, Brechot N, Merceron S, Luyt CE, Trouillet JL, Chastre J, Leprince P, Combes A (2013) Blood oxygenation and decarboxylation determinants during venovenous ECMO for respiratory failure in adults. Intensive Care Med 39:838–846
Abrams D, Brodie D, Combes A (2013) What is new in extracorporeal membrane oxygenation for ARDS in adults? Intensive Care Med 39:2028–2030
Azoulay E, Citerio G, Bakker J, Bassetti M, Benoit D, Cecconi M, Curtis JR, Hernandez G, Herridge M, Jaber S, Joannidis M, Papazian L, Peters M, Singer P, Smith M, Soares M, Torres A, Vieillard-Baron A, Timsit JF (2014) Year in review in Intensive Care Medicine 2013: II. Sedation, invasive and noninvasive ventilation, airways, ARDS, ECMO, family satisfaction, end-of-life care, organ donation, informed consent, safety, hematological issues in critically ill patients. Intensive Care Med 40:305–319
Abrams D, Combes A, Brodie D (2014) Extracorporeal membrane oxygenation in cardiopulmonary disease in adults. J Am Coll Cardiol 63:2769–2778
Agerstrand CL, Burkart KM, Abrams DC, Bacchetta MD, Brodie D (2015) Blood conservation in extracorporeal membrane oxygenation for acute respiratory distress syndrome. Ann Thorac Surg 99:590–595
Paden ML, Rycus PT, Thiagarajan RR, Registry E (2014) Update and outcomes in extracorporeal life support. Semin Perinatol 38:65–70
Davies A, Jones D, Bailey M, Beca J, Bellomo R, Blackwell N, Forrest P, Gattas D, Granger E, Herkes R, Jackson A, McGuinness S, Nair P, Pellegrino V, Pettila V, Plunkett B, Pye R, Torzillo P, Webb S, Wilson M, Ziegenfuss M (2009) Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. JAMA 302:1888–1895
Pham T, Combes A, Roze H, Chevret S, Mercat A, Roch A, Mourvillier B, Ara-Somohano C, Bastien O, Zogheib E, Clavel M, Constan A, Marie Richard JC, Brun-Buisson C, Brochard L (2013) Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med 187:276–285
Weingart C, Lubnow M, Philipp A, Bein T, Camboni D, Muller T (2015) Comparison of coagulation parameters, anticoagulation, and need for transfusion in patients on interventional lung assist or veno-venous extracorporeal membrane oxygenation. Artif Organs 39:765–773
Nair P, Davies AR, Beca J, Bellomo R, Ellwood D, Forrest P, Jackson A, Pye R, Seppelt I, Sullivan E, Webb S (2011) Extracorporeal membrane oxygenation for severe ARDS in pregnant and postpartum women during the 2009 H1N1 pandemic. Intensive Care Med 37:648–654
Zapol WM, Snider MT, Hill JD, Fallat RJ, Bartlett RH, Edmunds LH, Morris AH, Peirce EC 2nd, Thomas AN, Proctor HJ, Drinker PA, Pratt PC, Bagniewski A, Miller RG Jr (1979) Extracorporeal membrane oxygenation in severe acute respiratory failure. A randomized prospective study. JAMA 242:2193–2196
Morris AH, Wallace CJ, Menlove RL, Clemmer TP, Orme JF Jr, Weaver LK, Dean NC, Thomas F, East TD, Pace NL, Suchyta MR, Beck E, Bombino M, Sittig DF, Bohm S, Hoffmann B, Becks H, Butler S, Pearl J, Rasmusson B (1994) Randomized clinical trial of pressure-controlled inverse ratio ventilation and extracorporeal CO2 removal for adult respiratory distress syndrome. Am J Respir Crit Care Med 149:295–305
Combes A, Bacchetta M, Brodie D, Muller T, Pellegrino V (2012) Extracorporeal membrane oxygenation for respiratory failure in adults. Curr Opin Crit Care 18:99–104
Yeo HJ, Kim do H, Jeon D, Kim YS, Cho WH (2015) Low-dose heparin during extracorporeal membrane oxygenation treatment in adults. Intensive Care Med 41:2020–2021
Haneya A, Philipp A, Diez C, Ried M, Puehler T, Camboni D, Zausig Y, Lehle K, Schmid C (2009) Comparison of two different minimized extracorporeal circulation systems: hematological effects after coronary surgery. ASAIO J 55:592–597
Oliver WC (2009) Anticoagulation and coagulation management for ECMO. Semin Cardiothorac Vasc Anesth 13:154–175
Peek GJ, Firmin RK (1999) The inflammatory and coagulative response to prolonged extracorporeal membrane oxygenation. ASAIO J 45:250–263
Panigada M, Artoni A, Passamonti SM, Maino A, Mietto C, L’Acqua C, Cressoni M, Boscolo M, Tripodi A, Bucciarelli P, Gattinoni L, Martinelli I (2016) Hemostasis changes during veno-venous extracorporeal membrane oxygenation for respiratory support in adults. Minerva Anestesiol 82:170–179
Glick D, Dzierba AL, Abrams D, Muir J, Eisenberger A, Diuguid D, Abel E, Agerstrand C, Bacchetta M, Brodie D (2015) Clinically suspected heparin-induced thrombocytopenia during extracorporeal membrane oxygenation. J Crit Care 30:1190–1194
Cuker A, Gimotty PA, Crowther MA, Warkentin TE (2012) Predictive value of the 4Ts scoring system for heparin-induced thrombocytopenia: a systematic review and meta-analysis. Blood 120:4160–4167
Laverdure F, Louvain-Quintard V, Kortchinsky T, Rezaiguia-Delclaux S, Imbert A, Stephan F (2016) PF4-heparin antibodies during ECMO: incidence, course, and outcomes. Intensive Care Med. doi:10.1007/s00134-016-4262-2
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Vincent JL, de Mendonca A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 26:1793–1800
Schmidt M, Zogheib E, Roze H, Repesse X, Lebreton G, Luyt CE, Trouillet JL, Brechot N, Nieszkowska A, Dupont H, Ouattara A, Leprince P, Chastre J, Combes A (2013) The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med 39:1704–1713
Meyer AD, Wiles AA, Rivera O, Wong EC, Freishtat RJ, Rais-Bahrami K, Dalton HJ (2012) Hemolytic and thrombocytopathic characteristics of extracorporeal membrane oxygenation systems at simulated flow rate for neonates. Pediatr Crit Care Med 13:e255–e261
Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD (2001) Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol 54:774–781
Weerasinghe A, Taylor KM (1998) The platelet in cardiopulmonary bypass. Ann Thorac Surg 66:2145–2152
Bonfiglio MF, Traeger SM, Kier KL, Martin BR, Hulisz DT, Verbeck SR (1995) Thrombocytopenia in intensive care patients: a comprehensive analysis of risk factors in 314 patients. Ann Pharmacother 29:835–842
Crowther MA, Cook DJ, Meade MO, Griffith LE, Guyatt GH, Arnold DM, Rabbat CG, Geerts WH, Warkentin TE (2005) Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care 20:348–353
Lee KH, Hui KP, Tan WC (1993) Thrombocytopenia in sepsis: a predictor of mortality in the intensive care unit. Singap Med J 34:245–246
Strauss R, Wehler M, Mehler K, Kreutzer D, Koebnick C, Hahn EG (2002) Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Crit Care Med 30:1765–1771
Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM (2011) The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest 139:271–278
Schmidt M, Brechot N, Combes A (2015) Ten situations in which ECMO is unlikely to be successful. Intensive Care Med. doi:10.1007/s00134-015-4013-9
Lubnow M, Philipp A, Dornia C, Schroll S, Bein T, Creutzenberg M, Diez C, Schmid C, Pfeifer M, Riegger G, Muller T, Lehle K (2014) D-dimers as an early marker for oxygenator exchange in extracorporeal membrane oxygenation. J Crit Care 29(473):e471–e475
Cheung PY, Sawicki G, Salas E, Etches PC, Schulz R, Radomski MW (2000) The mechanisms of platelet dysfunction during extracorporeal membrane oxygenation in critically ill neonates. Crit Care Med 28:2584–2590
Muller G, Flecher E, Lebreton G, Luyt CE, Trouillet JL, Brechot N, Schmidt M, Mastroianni C, Chastre J, Leprince P, Anselmi A, Combes A (2016) The ENCOURAGE mortality risk score and analysis of long-term outcomes after VA-ECMO for acute myocardial infarction with cardiogenic shock. Intensive Care Med 42:370–378
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Brodie is currently on the medical advisory boards of ALung Technologies and Kadence. All compensation for these activities is paid to Columbia University. All other authors have no conflicts of interest to report.
Additional information
M. Bacchetta and D. Brodie are co-senior authors.
D. Abrams and M. R. Baldwin contributed equally to this work.
Take-home message: This study demonstrates that in a large single-center cohort, duration of ECMO support was not associated with a decrease in platelet count, which is contrary to the generally held belief that thrombocytopenia is an inevitable consequence of ECMO use. Instead, the development of thrombocytopenia was associated with severity of illness and lower baseline platelet count, suggesting that the current paradigm, attributing thrombocytopenia to the use of ECMO over time, needs to be revisited.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abrams, D., Baldwin, M.R., Champion, M. et al. Thrombocytopenia and extracorporeal membrane oxygenation in adults with acute respiratory failure: a cohort study. Intensive Care Med 42, 844–852 (2016). https://doi.org/10.1007/s00134-016-4312-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4312-9