Abstract
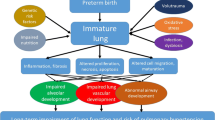
Advances in perinatal care have dramatically improved the outcome of preterm infants over the last few decades. Incidence of Bronchopulmonary Disease (BPD) has remained largely unchanged if not slightly increased over this time period, likely due to the increased survival of extremely preterm infants. BPD is a multifactorial disorder and infants frequently undergo treatment with various pharmacological agents, many of which lack efficacy in studies to date. BPD is an independent risk factor for neurodevelopmental delay and cerebral palsy (CP) in children. Therefore, the presence of CP needs to be considered when treating patients with BPD.
Similar content being viewed by others
References
Abman SH, Collaco JM, Shepherd EG et al (2017) Interdisciplinary care of children with severe bronchopulmonary dysplasia. J Pediatr 181:12–28e1
Advisory Committee on Immunization Practices (2017) The recommended immunization schedule for children and adolescents aged 18 years or younger. cdc.gov.
Barrington KJ (2001) The adverse neuro-developmental effects of postnatal steroids in the preterm infant: a systematic review of RCTs. BMC Pediatr 1:1. Meta-analysis
Bashir RA, Bhandari V, Vayalthrikkovil S et al (2016) Chorioamnionitis at birth does not increase the risk of neurodevelopmental disability in premature infants with bronchopulmonary dysplasia. Acta Paediatr 105:e506–e512
Bhandari A, McGrath-Morrow S (2013) Long-term pulmonary outcomes of patients with bronchopulmonary dysplasia. Semin Perinatol 37:132–137
Coalson JJ (2003) Pathology of new bronchopulmonary dysplasia. Semin Neonatol 8(1):73–81
Committee on infectious disease and bronchiolitis guideline committee AAP (2014) Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 134(2):415–420
Donn SM (2017) Bronchopulmonary dysplasia: myths of pharmacologic management. Semin Fetal Neonatal Med 22:354–358
Doyle LW, Anderson PJ (2009) Long term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med 14(6):391–395
Doyle LW, Cheong JL, Ehrenkranz RA et al (2017) Late (> 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev 10:CD001145-4
Fanaroff AA, Stoll BJ, Wright LL, NICHD Neonatal Research Network et al (2007) Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 196:147e1–147e8
Fok TF (2009) Adjunctive pharmacotherapy in neonates with respiratory failure. Semin Fetal Neonatal Med 14(1):49–55
Fortuna M, Carraro S, Temporin E et al (2016) Mid-childhood lung function in A Cohort of children with “New Bronchopulmonary Dysplasia”. Pediatr Pulmonol 51:1057–1064
Gibson AM, Doyle LW (2014) Respiratory outcomes for the tiniest or most immature infants. Semin Fetal Neonatal Med 19:105–111
Isayama T, Lee SK, Yang J et al (2017) Revisiting the definition of bronchopulmonary dysplasia effect of changing panoply of respiratory support for preterm neonates. JAMA Pediatr 171(3):271–279
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163(7):1723–1729
Malleske DT, Malleske DL, Chorna O, Maitre NL (2017) Pulmonary sequelae and functional limitations in children and adults with bronchopulmonary dysplasia. Paediatr Resp Rev. https://doi.org/10.1016/j.prrv.2017.07.002
Manja V, Saugstad OD, Lakshminrusimha S (2017) Oxygen saturation targets in preterm infants and outcomes at 18–24 months: a systematic review. Pediatrics 139(1):e20161609
Moon NM, Mohay HA, Gray PH (2007) Developmental patterns from 1 to 4 years of extremely preterm infants who required home oxygen therapy. Early Hum Dev 83:209–216
Northway WH Jr, Rosan RC, Porter DY (1967) Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med 276(7):357–368
Prais D, Kaplan E, Klinger G et al (2016) Short- and long-term pulmonary outcome of palivizumab in children born extremely prematurely. Chest 149(3):801–808
Roberts D, Brown J, Medley N et al (2006) Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev (2)
Schmidt B, Roberts RS, Davis P (2006) Caffeine therapy for apnea of prematurity. N Engl J Med 354:2112–2121
Schmidt B, Roberts RS, Davis P (2007) Long-term effects of caffeine therapy for apnea of prematurity. N Engl J Med 357:1893–1902
Schmidt B, Roberts RS, Anderson PJ, Caffeine for Apnea of Prematurity (CAP) Trial Group et al (2017) Academic performance, motor function, and behavior 11 years after neonatal caffeine citrate Therapy for apnea of prematurity: an 11-year follow-up of the CAP randomized clinical trial. JAMA Pediatr 171(6):564–572
Shi Z, Ma L, Luo K et al (2017) Chorioamnionitis in the development of cerebral palsy: a meta-analysis and systematic review. Pediatrics 139(6):e20163781
Skidmore MD, Rivers A, Hack M (1990) Increased risk of cerebral palsy among very low – birthweight infants with chronic lung disease. Dev Med Child Neurol 32:325–332
Stoll BJ, Hansen NI, Bell EF et al (2015) Trends in care practices, morbidity and mortality of extremely preterm neonates, 1993–2012. JAMA 314(10):1039–1051
Tin W, Wiswell TE (2009) Drug therapies in bronchopulmonary dysplasia: debunking the myths. Semin Fetal Neonatal Med 14(6):383–390
Tonson la Tour A, Spadola L, Sayegh Y et al (2013) Chest CT in bronchopulmonary dysplasia: clinical and radiological correlations. Pediatr Pulmonol 48:693–698
Van Marter LJ, Kuban KCK, Allred E et al (2011) Does bronchopulmonary dysplasia contribute to the occurrence of cerebral palsy among infants born before 28 weeks of gestation? Arch Dis Child Fetal Neonatal Ed 96:20–29
Yeh TF, Chen CM, Wu SY et al (2016) Intratracheal administration of budesonide/surfactant to prevent bronchopulmonary dysplasia. Am J Respir Crit Care Med 193:86–95
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this entry
Cite this entry
Flanagan, F., Bhandari, A. (2019). Bronchopulmonary Dysplasia and Cerebral Palsy. In: Miller, F., Bachrach, S., Lennon, N., O'Neil, M. (eds) Cerebral Palsy. Springer, Cham. https://doi.org/10.1007/978-3-319-50592-3_67-1
Download citation
DOI: https://doi.org/10.1007/978-3-319-50592-3_67-1
Received:
Accepted:
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-50592-3
Online ISBN: 978-3-319-50592-3
eBook Packages: Springer Reference MedicineReference Module Medicine