Abstract
Background
Venous thromboembolism (VTE) is a complication that affects approximately 30 % of moderate and severe traumatic brain injury (TBI) patients when pharmacologic prophylaxis is not used. Following TBI, specifically in the case of contusions, the safety and efficacy of pharmacologic thromboembolism prophylaxis (PTP) has been studied only in small sample sizes. In this study, we attempt to assess the safety and efficacy of a PTP protocol for TBI patients, as a quality improvement (QI) initiative, in the neuroscience intensive care unit (NSICU).
Methods
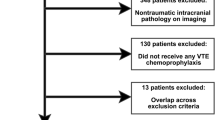
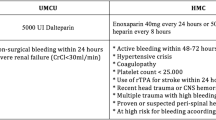
Between January 1st and December 31st, 2009, consecutive patients discharged from the University of Wisconsin NSICU after >a 48 h minimum stay were evaluated as part of a QI project. A protocol for the initiation of PTP was designed and implemented for NSICU patients. The protocol did not vary based on type of intracranial injury. The rate of VTE was reported as was heparin-induced thrombocytopenia and PTP-related expansion of intracranial hemorrhage (IH) requiring reoperation. The number of patients receiving PTP and the timing of therapy were tracked. Patients were excluded for persistent coagulopathy, other organ system bleeding (such as the gastrointestinal tract), or pregnancy. Faculty could opt out of the protocol without reason. Using the same criteria, patients discharged during the preceding 6 months, from July 1st to December 31st, 2008, were evaluated as controls as the PTP protocol was not in effect during this time.
Results
During the control period, there were 48 head trauma admissions who met the inclusion criteria. In 22 patients (45.8 %), PTP was initiated at an average of 4.9 ± 5.4 days after admission. During the protocol period, there were 87 head trauma admissions taken from 1,143 total NSICU stays who met criteria. In 63 patients (72.4 %), the care team in the NSICU successfully initiated PTP, at an average of 3.4 ± 2.8 days after admission. All 87 trauma patients were analyzed, and the rate of clinically significant deep venous thrombosis (DVT) was 6.9 % (6 of 87). Three protocol patients (3.45 %) went to the operating room for surgery after the initiation of PTP; none of these patients had a measurable change in hemorrhage size on head CT. The change in percentage of patients receiving PTP was significantly increased by the protocol (p < 0.0001); while the average days to first PTP dose trended down with institution of the protocol, this change was not statistically significant.
Conclusion
A PTP protocol in the NSICU is useful in controlling the number of complications from DVT and pulmonary embolism while avoiding additional IH. This protocol, based on a published body of literature, allowed for VTE rates similar to published rates, while having no PTP-related hemorrhage expansion. The protocol significantly changed physician behavior, increasing the percentage of patients receiving PTP during their hospitalization; whether long-term patient outcomes are affected is a potential goal for future study.






Similar content being viewed by others
References
Traumatic Brain Injury in the United States. 2010. http://www.cdc.gov/TraumaticBrainInjury/index.html. Accessed May 2011.
Ekeh AP, Dominguez KM, Markert RJ, McCarthy MC. Incidence and risk factors for deep venous thrombosis after moderate and severe brain injury. J Trauma. 2010;68:912–5.
Geerts WH, Code KI, Jay RM, Chen E, Szalai JP. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331:1601–6.
Kudsk KA, Fabian TC, Baum S, Gold RE, Mangiante E, Voeller G. Silent deep vein thrombosis in immobilized multiple trauma patients. Am J Surg. 1989;158:515–9.
Kim J, Gearhart MM, Zurick A, Zuccarello M, James L, Luchette FA. Preliminary report on the safety of heparin for deep venous thrombosis prophylaxis after severe head injury. J Trauma. 2002;53:38–42; discussion 43.
Dennis JW, Menawat S, Von Thron J, et al. Efficacy of deep venous thrombosis prophylaxis in trauma patients and identification of high-risk groups. J Trauma. 1993;35:132–8; discussion 138–9.
Arnold JD, Dart BW, Barker DE, et al. Gold Medal Forum Winner. Unfractionated heparin three times a day versus enoxaparin in the prevention of deep vein thrombosis in trauma patients. Am Surg. 2010;76:563–70.
Paffrath T, Wafaisade A, Lefering R, et al. Venous thromboembolism after severe trauma: incidence, risk factors and outcome. Injury. 2010;41:97–101.
Levy AS, Salottolo K, Bar-Or R, et al. Pharmacologic thromboprophylaxis is a risk factor for hemorrhage progression in a subset of patients with traumatic brain injury. J Trauma. 2010;68:886–94.
Norwood SH, Berne JD, Rowe SA, Villarreal DH, Ledlie JT. Early venous thromboembolism prophylaxis with enoxaparin in patients with blunt traumatic brain injury. J Trauma. 2008;65:1021–6; discussion 6–7.
Koehler DM, Shipman J, Davidson MA, Guillamondegui O. Is early venous thromboembolism prophylaxis safe in trauma patients with intracranial hemorrhage. J Trauma. 2011;70:324–9.
Scudday T, Brasel K, Webb T, et al. Safety and efficacy of prophylactic anticoagulation in patients with traumatic brain injury. J Am Coll Surg. 2011;213:148–53; discussion 53–4.
Dickinson LD, Miller LD, Patel CP, Gupta SK. Enoxaparin increases the incidence of postoperative intracranial hemorrhage when initiated preoperatively for deep venous thrombosis prophylaxis in patients with brain tumors. Neurosurgery. 1998;43:1074–81.
Agnelli G, Piovella F, Buoncristiani P, et al. Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med. 1998;339:80–5.
Nurmohamed MT, van Riel AM, Henkens CM, et al. Low molecular weight heparin and compression stockings in the prevention of venous thromboembolism in neurosurgery. Thromb Haemost. 1996;75:233–8.
Norwood SH, McAuley CE, Berne JD, et al. Prospective evaluation of the safety of enoxaparin prophylaxis for venous thromboembolism in patients with intracranial hemorrhagic injuries. Arch Surg. 2002;137:696–701; discussion 701–2.
Velmahos GC, Nigro J, Tatevossian R, et al. Inability of an aggressive policy of thromboprophylaxis to prevent deep venous thrombosis (DVT) in critically injured patients: are current methods of DVT prophylaxis insufficient? J Am Coll Surg. 1998;187:529–33.
Geerts WH, Jay RM, Code KI, et al. A comparison of low-dose heparin with low-molecular-weight heparin as prophylaxis against venous thromboembolism after major trauma. N Engl J Med. 1996;335:701–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nickele, C.M., Kamps, T.K. & Medow, J.E. Safety of a DVT Chemoprophylaxis Protocol Following Traumatic Brain Injury: A Single Center Quality Improvement Initiative. Neurocrit Care 18, 184–192 (2013). https://doi.org/10.1007/s12028-012-9786-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9786-x