Abstract
Background
Surgical site infection (SSI) after total joint arthroplasty (TJA) is a rare but devastating complication. Various skin antiseptic applications are used preoperatively to prevent SSI. Recent literature suggests 2% chlorhexidine gluconate (CHG) wipes reduce microbial content at surgical sites, but it is unclear whether they reduce rates of SSI.
Questions/purposes
We compared the SSI rates between TJAs with and without CHG wipe use (1) with all TJAs in one group and (2) stratified by surgical subgroup (THA, TKA).
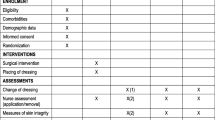
Methods
We retrospectively reviewed all 3715 patients who underwent primary TJA from 2007 to 2009. CHG wipes were introduced at our facility on April 21, 2008. We compared SSI of patients before (n = 1824) and after (n = 1891) the introduction of CHG wipes. The wipes were applied 1 hour before surgery. There were 1660 patients with THA (845 CHG, 815 no CHG) and 2055 patients with TKA (1046 CHG, 1009 no CHG). Infections were diagnosed based on the Musculoskeletal Infection Society Guidelines for periprosthetic joint infection. All patients were tracked for 1 year.
Results
SSI incidences were similar in patients receiving (1.0%, 18 of 1891) and not receiving (1.3%, 24 of 1824) CHG wipes. In patients with THA, there was no difference in SSI between those receiving (1.2%, 10 of 845) and not receiving (1.5%, 12 of 815) CHG wipes. In patients with TKA, there also was no difference in SSI between those receiving (0.8%, eight of 1046) and not receiving (1.2%, 12 of 1009) CHG wipes.
Conclusions
Introduction of CHG-impregnated wipes in the presurgical setting was not associated with a reduced SSI incidence. Our analysis suggests CHG wipes in TJA are unnecessary as an adjunct skin antiseptic, as suggested in previous smaller studies.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
References
Anderson DJ, Sexton DJ, Kanafani ZA, Auten G, Kaye KS. Severe surgical site infection in community hospitals: epidemiology, key procedures, and the changing prevalence of methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol. 2007;28:1047–1053.
Bode LG, Kluytmans JA, Wertheim HF, Bogaers D, Vandenbroucke-Grauls CM, Roosendaal R, Troelstra A, Box AT, Voss A, van der Tweel I, van Belkum A, Verbrugh HA, Vos MC. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010;362:9–17.
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51.
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133.
Broex EC, van Asselt AD, Bruggeman CA, van Tiel FH. Surgical site infections: how high are the costs? J Hosp Infect. 2009;72:193–201.
Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992;326:281–286.
Coello R, Charlett A, Wilson J, Ward V, Pearson A, Borriello P. Adverse impact of surgical site infections in English hospitals. J Hosp Infect. 2005;60:93–103.
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–397.
Dripps RD. New classification of physical status. Anesthesiology. 1963;24:111.
Edmiston CE Jr, Okoli O, Graham MB, Sinski S, Seabrook GR. Evidence for using chlorhexidine gluconate preoperative cleansing to reduce the risk of surgical site infection. AORN J. 2010;92:509–518.
Edmiston CE Jr, Seabrook GR, Johnson CP, Paulson DS, Beausoleil CM. Comparative of a new and innovative 2% chlorhexidine gluconate-impregnated cloth with 4% chlorhexidine gluconate as topical antiseptic for preparation of the skin prior to surgery. Am J Infect Control. 2007;35:89–96.
Edwards C, Counsell A, Boulton C, Moran CG. Early infection after hip fracture surgery: risk factors, costs and outcome. J Bone Joint Surg Br. 2008;90:770–777.
Eiselt D. Presurgical skin preparation with a novel 2% chlorhexidine gluconate cloth reduces rates of surgical site infection in orthopaedic surgical patients. Orthop Nurs. 2009;28:141–145.
Erratum. J Arthroplasty. 2012;27:658.
Jämsen E, Varonen M, Huhtala H, Lehto MU, Lumio J, Konttinen YT, Moilanen T. Incidence of prosthetic joint infections after primary knee arthroplasty. J Arthroplasty. 2010;25:87–92.
Johnson AJ, Daley JA, Zywiel MG, Delanois RE, Mont MA. Preoperative chlorhexidine preparation and the incidence of surgical site infections after hip arthroplasty. J Arthroplasty. 2010;25(6 suppl):98–102.
Karpanen TJ, Casey AL, Conway BR, Lambert PA, Elliott TS. Antimicrobial activity of a chlorhexidine intravascular catheter site gel dressing. J Antimicrob Chemother. 2011;66:1777–1784.
Kaye KS, Anderson DJ, Sloane R, Chen LF, Choi Y, Link K, Sexton DJ, Schmader KE. The effect of surgical site infection on older operative patients. J Am Geriatr Soc. 2009;57:46–54.
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725–730.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23:984–991.
Milstone AM, Passaretti CL, Perl TM. Chlorhexidine: expanding the armamentarium for infection control and prevention. Clin Infect Dis. 2008;46:274–281.
Monge Jodra V, Sainz de Los Terreros Soler L, Diaz-Agero Perez C, Saa Requejo CM, Plana Farras N. Excess length of stay attributable to surgical site infection following hip replacement: a nested case-control study. Infect Control Hosp Epidemiol. 2006;27:1299–1303.
Mortazavi SM, Schwartzenberger J, Austin MS, Purtill JJ, Parvizi J. Revision total knee arthroplasty infection: incidence and predictors. Clin Orthop Relat Res. 2010;468:2052–2059.
Murray MR, Saltzman MD, Gryzlo SM, Terry MA, Woodward CC, Nuber GW. Efficacy of preoperative home use of 2% chlorhexidine gluconate cloth before shoulder surgery. J Shoulder Elbow Surg. 2011;20:928–933.
National Nosocomial Infections Surveillance (NNIS) report, data summary from October 1986–April 1996, issued May 1996. A report from the National Nosocomial Infections Surveillance (NNIS) System. Am J Infect Control. 1996;24:380–388.
Ostrander RV, Botte MJ, Brage ME. Efficacy of surgical preparation solutions in foot and ankle surgery. J Bone Joint Surg Am. 2005;87:980–985.
Ouédraogo AS, Somé DA, Dakouré PW, Sanon BG, Birba E, Poda GE, Kambou T. Bacterial profile of surgical site infections at Souro Sanou National Hospital Center in Bobo Dioulasso, Burkina Faso. Med Trop (Mars). 2011;71:49–52.
Peersman G, Laskin R, Davis J, Peterson M. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res. 2001;392:15–23.
Rao N, Cannella B, Crossett LS, Yates AJ Jr, McGough R 3rd. A preoperative decolonization protocol for staphylococcus aureus prevents orthopaedic infections. Clin Orthop Relat Res. 2008;466:1343–1348.
Rao N, Cannella BA, Crossett LS, Yates AJ Jr, McGough RL 3rd, Hamilton CW. Preoperative screening/decolonization for Staphylococcus aureus to prevent orthopedic surgical site infection: prospective cohort study with 2-year follow-up. J Arthroplasty. 2011;26:1501–1507.
Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R. Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:844–850.
Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton LJ 3rd, Kurland RL, Berry DJ. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969–2008. Mayo Clin Proc. 2010;85:898–904.
Webb BG, Lichtman DM, Wagner RA. Risk factors in total joint arthroplasty: comparison of infection rates in patients with different socioeconomic backgrounds. Orthopedics. 2008;31:445.
Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23:183–189.
Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2011;26:1136–1138.
Zywiel MG, Daley JA, Delanois RE, Naziri Q, Johnson AJ, Mont MA. Advance pre-operative chlorhexidine reduces the incidence of surgical site infections in knee arthroplasty. Int Orthop. 2011;35:1001–1006.
Acknowledgments
The authors thank the University of Pittsburgh Medical Center Infection Prevention & Control Department staff for their assistance in obtaining data for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at University of Pittsburgh Medical Center, Shadyside Hospital, Pittsburgh, PA, USA.
About this article
Cite this article
Farber, N.J., Chen, A.F., Bartsch, S.M. et al. No Infection Reduction Using Chlorhexidine Wipes in Total Joint Arthroplasty. Clin Orthop Relat Res 471, 3120–3125 (2013). https://doi.org/10.1007/s11999-013-2920-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-2920-z