Abstract
Introduction
It is unclear which antibiotic regimen provides the best prophylaxis against surgical site infection (SSI) in patients undergoing hip and knee surgery.
Questions/purposes
Therefore, we determined whether dual antibiotic prophylaxis (1) reduced the rate of SSI compared to single antibiotic prophylaxis and (2) altered the microbiology of SSI.
Methods
We retrospectively reviewed 1828 primary THAs and TKAs performed between September 1, 2008 and December 31, 2010. We divided patients into two groups: (1) those who received a dual prophylactic antibiotic regimen of cefazolin and vancomycin (unless allergy), or (2) received cefazolin (unless allergy) as the sole prophylactic antibiotic. There were 701 males and 1127 females with an average age of 56 years (range, 15–97 years). We limited followup to 1 year, presuming subsequent infections were not related to the initial surgery.
Results
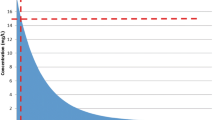
During this period, there were 22 SSIs (1.2%). The infection rates for dual antibiotic prophylaxis compared to a single antibiotic regimen were 1.1% and 1.4%, respectively. Of 1328 patients treated with dual antibiotic prophylaxis, only one (0.08%) SSI was culture positive for methicillin resistant Staphylococcus aureus (MRSA), while four of 500 patients (0.8%) receiving only cefazolin prophylaxis had culture positive MRSA infection at the time of reoperation.
Conclusion
The addition of vancomycin as a prophylactic antibiotic agent apparently did not reduce the rate of SSI compared to cefazolin alone. Use of vancomycin in addition to cefazolin appeared to reduce the incidence of MRSA infections; however, the number needed to treat to prevent a single MRSA infection was very high.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
References
American Academy of Orthopaedic Surgeons Advisory Statement: Recommendations for the use of intravenous antibiotic prophylaxis in primary total joint arthroplasty. Available at: http://www.aaos.org/about/papers/advistmt/1027.asp. Accessed August 27, 2011.
Ayliffe GA. Role of the environment of the operative suite in surgical wound infection. Rev Infect Dis. 1991;13(Suppl. 10):S800–S804.
Bauer TW, Parvizi J, Kobayashi N, Krebs V. Diagnosis of periprosthetic infection. J Bone Joint Surg Am. 2006;88:869–882.
Boxma H, Broekhuizen T, Patka P, Oosting H. Randomized control trial of a single dose antibiotic prophylaxis in surgical treatment of closed fractures: the Dutch Trauma Trial. Lancet. 1996;347:1133–1137.
Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am. 2005;87:570–576.
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133.
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51.
Bratzler DW, Houck PM; Surgical Infection Prevention Guideline Writers Workgroup. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Am J Surg. 2005;189:395–404.
Dale WB, Peter MH. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis. 2004;38:1706–1715.
Darouiche RO. Treatment of infections associated with surgical implants. N Engl J Med. 2004;350:1422–1429.
Douglas P, Asimus M, Swan J, Spigelman A. Prevention of orthopaedic wound infections: a quality improvement project. J Qual Clin Pract. 2001;21:149–153.
Dreghorn CR, Hamblen DL. Revision arthroplasty: a high price to pay. BMJ. 1989;296:648–649.
Fierobe L, Decré D, Mùller C, Lucet JC, Marmuse JP, Mantz J, Desmonts JM. Methicillin-resistant Staphylococcus aureus as a causative agent of postoperative intra-abdominal infection: relation to nasal colonization. Clin Infect Dis. 1999;29:1231–1238.
Finkelstein R, Rabino G, Mashiah T, Bar-El Y, Adler Z, Kertzman V, Cohen O, Milo S. Vancomycin versus cefazolin prophylaxis for cardiac surgery in the setting of a high prevalence of methicillin-resistant staphylococcal infections. J Thorac Cardiovasc Surg. 2002;123:326–332.
Gavin KL, Konigsberg BS. Infection following total knee arthroplasty: prevention and management. J Bone Joint Surg Am. 2011;93:1167–1175.
Gobran SR, Goldman S, Ferdinand F, Wertan MA, Trace C, Grunkemeier GL, Wu Y, Sutter FP. Outcomes after usage of a quality initiative program for off-pump coronary artery bypass surgery; a comparison with on-pump surgery. Ann Thorac Surg. 2004;78:2015–2021.
Gupta K, Strymish J, Abi-Haidar Y, Williams SA, Itani KM. Preoperative nasal methicillin-resistant Staphylococcus aureus status, surgical prophylaxis, and risk-adjusted postoperative outcomes in veterans. Infect Control Hosp Epidemiol. 2011;32:791–796.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13:606–608.
Jiranek WA, Hanssen AD, Greenwald AS. Antibiotic-loaded bone cement for infection prophylaxis in total joint replacement. J Bone Joint Surg Am. 2006;88:2487–2500.
Kim DH, Spencer M, Davidson SM, Li L, Shaw JD, Gulczynski D, Hunter DJ, Martha JF, Miley GB, Parazin SJ, Dejoie P, Richmond JC. Institutional prescreening for detection and eradication of MRS in patients undergoing elective orthopaedic surgery. J Bone Joint Surg Am. 2010;92:1820–1826.
Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. N Engl J Med. 1988;318:1728–1733.
Leung F, Richards CJ, Garbuz DS, Masri BA, Duncan CP. Two stage total hip arthroplasty: how often does it control methicillin-resistant infection? Clin Orthop Relat Res. 2011;469:1009–1015.
Lidwell OM, Lowbury EJ, Whyte W, Blowers R, Stanley SJ, Lowe D. Effects of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. Br Med J (Clin Res Ed). 1982;285:10–14.
Lynch RJ, Englesbe MJ, Sturm L, Bitar A, Budhiraj K, Kolla S, Polyachenko Y, Duck MG, Campbell DA Jr. Measurement of foot traffic in the operating room: implications for infection control. Am J Med Qual. 2009;24:45–52.
Malangoni MA, Cheadle WG, Dodson TF, Dohmen PM, Jones D, Katariya K, Kolvekar S, Urban JA. New opportunities for reducing risk of surgical site infection. Surg Infect (Larchmt). 2006;7(Suppl. 1):S23–S39.
Mangram AJ. A brief overview of the 1999 CDC guideline for the prevention of surgical site infection: centers for disease control and prevention. J Chemother. 2001;13:35–39.
Marculescu CE, Osmon DR. Antibiotic prophylaxis in orthopaedic prosthetic surgery. Infect Dis Clinic N Am. 2009;19:931–946.
Meehan J, Jamali AA, Nguyen, H. Prophylactic antibiotics in hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91:2480–2489.
Merrer J, Desbouchages L, Serazin V, Razafimamonjy J, Pauthier F, Leneveu M. Comparison of routine prophylaxis with vancomycin or cefazolin for femoral neck fracture surgery: microbiological and clinical outcomes. Infect Control Hosp Epidemiol. 2006;27:1366–1371.
Miller LG, McKinnell JA, Vollmer ME, Spellberg B. Impact of methicillin-resistant Staphylococcus aureus prevalence among S. aureus isolates on surgical site infection risk after coronary artery bypass surgery. Infect Control Hosp Epidemiol. 2011;32:342–350.
Peel TN, Dowsey MM, Daffy JR, Stanley PA, Choong PF, Buising KL. Risk factors for prosthetic hip and knee infections according to arthroplasty site. J Hosp Infect. 2011;79:129–133.
Perencevich EN, Sands KE, Cosgrove SE, Guadagnoli E, Meara E, Platt R. Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis. 2003;9:196–203.
Prokuski L. Prophylactic antibiotics in orthopaedic surgery. J Am Acad Orthop Surg. 2008;16:283–293.
Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R. Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:844–850.
Ritter MA, Barzilauskas CD, Faris PM, Keating PM. Vancomycin prophylaxis and elective total joint arthroplasty. Orthopedics. 1989;12:1333–1336.
Thomas C, Cadwallader HL, Riley TV. Surgical-site infections after orthopaedic surgery: statewide surveillance using linked administrative databases. J Hosp Infect. 2004;57:25–30.
Tyllianakis ME, Karageorgos ACh, Marangos MN, Saridis AG, Lambiris EE. Antibiotic prophylaxis in primary hip and knee arthroplasty: comparison between cefuroxime and two specific antistaphylococcal agents. J Arthroplasty. 2010;25:1078–1082.
van Kasteren ME, Mannien J, Kullberg BJ, de Boer AS, Nagelkerke NJ, Ridderhof M, Wille JC, Gyssens IC. Quality improvement of surgical prophylaxis in Dutch hospitals: evaluation of a multi-site intervention by time series analysis. J Antimicrob Chemother. 2005;56:1094–1102.
Walsh EE, Greene L, Kirshner R. Sustained reduction in methicillin-resistant Staphylococcus aureus wound infections after cardiothoracic surgery. Arch Intern Med. 2011;171:68–73.
Wiesel BB, Esterhai JJ. Chapter 4: Prophylaxis of musculoskeletal infection. In Calhoun JJ and Mader JT (eds). Musculoskeletal Infections. Marcel Dekker, Inc., New York, NY. 2003;115–129.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351:1645–1654.
Acknowledgments
The authors thank Jonathan P Garino MD, Charles L Nelson MD, and Craig L Israelite MD for contributing patients for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Sewick, A., Makani, A., Wu, C. et al. Does Dual Antibiotic Prophylaxis Better Prevent Surgical Site Infections in Total Joint Arthroplasty?. Clin Orthop Relat Res 470, 2702–2707 (2012). https://doi.org/10.1007/s11999-012-2255-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2255-1