Opinion statement
-
•The treatment of migraine headache in children depends on the following: a) defining the underlying cause; b) the frequency of the attacks; and c) the severity of the disability produced by the pain.
-
•Any medication taken to relieve pain is most effective if taken at maximum dose at the onset of the headache. The dose should be the maximum recommended by weight or age. Triptans are also more effective if used early.
-
•Over-the-counter (OTC) analgesics are often effective in relieving pediatric headache and should be tried before prescription drug therapy is attempted.
-
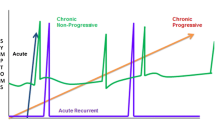
•The more frequent a child’s headaches are, the greater the danger that repeated doses of pain medications, including those purchased OTC, will lead to a chronic headache syndrome as the medication is reduced.
-
•Recurrent severe headaches, occurring more than once a week and resulting in interruption of normal activities or poor concentration, need to be treated with prophylactic medications taken daily so that the number of headaches can be reduced. Amitriptyline, propanolol, and periactin are the most frequently used drugs to block headaches, but valproate, verapamil, or other calcium channel blockers and other antidepressants are also useful.
-
•Biofeedback, relaxation, or cognitive therapies can also reduce headache frequency in children with both migraine and tension headaches.
-
•Headaches that are intractable to oral medication for the acute relief of pain may respond more rapidly to an efficiently absorbed drug administered by nasal spray or subcutaneously.
-
•The initial dose of an injectable drug should be given in a situation where a physician is immediately available.
-
•Recurrent headaches that have occurred over more than 6 months and that are associated with a normal neurologic examination are almost never caused by an intracranial lesion. Routine CT and MRI scans or an electroencephalogram (EEG) are generally unnecessary for these patients because these scans are rarely of value in these patients unless there is a history of another neurologic disorder or the headaches are focal, relentless, and worsening over time.
Similar content being viewed by others
References
Bille B: Migraine in school children. Acta Paediatrica 1962, 51(suppl):15–151.
Sillanpää M: Changes in the prevalence of migraine and other headaches during the first seven school years. Headache 1983, 23:15–19.
Prensky AL, Sommer D: Diagnosis and treatment of migraine in children. Neurology 1979, 29:506–510.
Headache Classification Committee of the International Headache Society: Classification and diagnostic criteria for headache disorders, cranial neuralgia and facial pain. Cephalgia 1988, 8(suppl):1–96.
Mathew NT: Transform migraine, analgesic, rebound and other chronic daily headaches. Neurol Clin 1997, 15:167–186.
Blau JN, Diamond S: Dietary factors in migraine precipitation: the physician’s view. Headache 1985, 25:184–187.
Silberstein SD: Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review). A report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000, 55:754–762. This paper summarizes four evidence-based reviews of the diagnosis and treatment of migraine. The reviews themselves are lengthy and thus far only available on the internet. Unfortunately, the method of classifying studies and grading results is not given in detail. However, the grading of acute and prophylactic therapy and the summary of nonpharmacologic treatments is very helpful. There is no special section for pediatric headache.
Hämäläinen JL, Hoppu K, Valkeila E, Santavuori P: Ibuprofen or acetaminophen for the acute treatment of migraine in children: A double-blind, randomized, placebo-controlled crossover study. Neurology 1997, 48:103–107. A double-blind crossover study that compares the effectiveness of acetaminophen with ibuprofen in children with acute migraine headaches. Both were compared with a placebo with regard to reduction of severity of headache 2 hours after a single dose. In addition, 15 mg/kg of acetaminophen was compared with10 mg/kg of ibuprofen. When headaches were rated on a five scale, ibuprofen resulted in a reduction of two or more grades three times as often as the placebo, and acetaminophen achieved similar results only twice as often.
Goldstein J, Gawel MJ, Wimer P, et al.: Comparison of butorphanol nasal spray and Fiorinal with codeine in the treatment of migraine. Headache 1998, 38:516–522.
Becker WJ, Riess CM, Hoag J: Effectiveness of subcutaneous dihydroergotamine by home injection for migraine. Headache 1996, 36:144–148.
Treves TA, Kuritzky A, Hering R, Korczyn AD: Dihydroergotamine nasal spray in the treatment of acute migraine. Headache 1998, 38:614–617.
Hämäläinen ML, Hoppu K, Santavuori P: Sumatriptan for migraine attacks in children: A randomized placebo-controlled study. Do children with migraine respond to oral sumatriptan differently from adults? Neurology 1997, 48:1100–1103. This was a randomized, double-blind, placebo-controlled crossover study with an endpoint of 50% or greater decrease in headache at 2 hours. There were 23 children studied, and the results with oral sumatriptan did not differ in any statistically significant way from the placebo in this small number of children.
Linder SL: Subcutaneous Sumatriptan in the clinical setting: The first 50 consecutive patients with acute migraine in a pediatric neurology office practice. Headache 1996, 36:419–422.
Robbins L, Maides JF: Long-term daily triptan use: 59 patients. Headache Q 2000, 11:127–131.
Couch JR, Ziegler DK, Hassanein R: Amitriptyline in the prophylaxis of migraine. Neurology 1976, 26:121–127.
Hershey AD, Powers SW, Bentti A, deGrauw TJ: Effectiveness of Amitriptyline in the prophylactic management of childhood headaches. Headache 2000, 40:539–549. A nonrandomized, nonblinded trial without controls in which children with greater than three headaches per month were started on daily amitriptyline that was gradually increased to 1 mg/kg. Eighty-four percent had an overall perception of improvement.
Forsythe WI, Gillies D, Sills MA: Propanolol (’Inderal’) in the treatment of childhood migraine. Develop Med Child Neurol 1984, 25:727–741.
Markley HG, Cheronis JCD, Piepho RW: Verapamil in prophylactic therapy of migraine. Neurology 1984, 34:973–976.
Silberstein SD, Collins SD: Safety of Divalproex in migraine prophylaxis: an open-label, long-term study. Headache 1999, 39:633–643.
Silberstein SD: Divalproex sodium in headache: literature review and clinical guidelines. Headache 1996, 36:547–555.
Holden EW, Deichmann MM, Levy JD: Empirically supported treatments in pediatric psychology: recurrent pediatric headache. J Pediatr Psychol 1999, 24:91–109.
Sarafino EP, Goehring P: Age comparisons in acquiring biofeedback control and success in reducing headache pain. Ann Behav Med 2000, 22:10–16.
Pryse-Phillips WEM, Dodick DW, Edmeads JG, et al.: Guidelines for the nonpharmacologic management of migraine in clinical practice. CMAJ 1998, 159:47–54.
Rokicki LA, Holroyd KA, France CR, et al.: Change mechanisms associated with combined relaxation/ EMG biofeedback training for chronic tension headache. Appl Psychophysiol Biofeedback 1997, 22:21–41.
Walker Z, Walker RWH, Robertson MM, Stansfeld S: Antidepressant treatment of chronic tension-type headache: a comparison between fluoxetine and desipramine. Headache 1998, 38:523–528.
Silberstein SD, Silberstein JR: Chronic daily headache: long-term prognosis following inpatient treatment with repetitive IV DHE. Headache 1992, 32:439–445.
Redillas C, Solomon S: Prophylactic pharmacological treatment of chronic daily headache. Headache 2000, 40:83–102.
Clerico DM: Sinus headaches reconsidered: referred cephalgia of rhinologic origin masquerading as refractory primary headache. Headache 1995, 35:185–192.
Wald ER: Chronic sinusitis in children. J Peds 1995, 127:339–347.
Vallon D, Ekberg EC, Nilner M, Kopp S: Short-term effect of occlusal adjustment on craniomandibular disorders including headaches. Acta Odontol Scand 1991, 49:89–96.
Magnusson T, Syren M: Therapeutic jaw exercises and interocclusal appliance therapy: a comparison between two common treatments of temporomandibular disorders. Swed Dent J 1999, 23:27–37.
DeVeber G, Chan A, Monagle P, et al.: Anticoagulation therapy in pediatric patients with sinovenous thrombosis: a cohort study. Arch Neurol 1998, 55:1533–1537.
Philips MF, Bagley LJ, Sinson GP, et al.: Endovascular thrombolysis for symptomatic cerebral venous thrombosis. J Neurosurg 1999, 90:65–71.
Silberstein SD: Evaluation and emergency treatment of headache. Headache 1992, 32:396–407.
Kan L, Nagelberg J, Maytal J: Headaches in a pediatric emergency department: etiology, imaging, and treatment. Headache 2000, 40:25–29.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Prensky, A. Childhood migraine headache syndromes. Curr Treat Options Neurol 3, 257–270 (2001). https://doi.org/10.1007/s11940-001-0007-8
Issue Date:
DOI: https://doi.org/10.1007/s11940-001-0007-8