Opinion statement
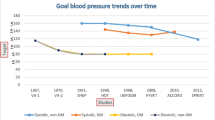
The American College of Cardiology (ACC)/American Heart Association (AHA) 2011 expert consensus document on hypertension in the elderly recommends that the blood pressure be reduced to less than 140/90 mmHg in adults aged 60–79 years and the systolic blood pressure to 140 to 145 mmHg if tolerated in adults aged 80 years and older. I strongly support these guidelines based on clinical trial data, especially from the Systolic Hypertension in the Elderly trial and from the Hypertension in the Very Elderly trial (HYVET). Other guidelines supporting reducing the blood pressure to less than 140/90 mmHg in adults aged 60 to 79 years of age include the European Society of Hypertension (ESH)/European Society of Cardiology (ESC) 2013 guidelines, the minority report from the 2013 Eighth Joint National Committee (JNC 8) guidelines, the 2013 Canadian Hypertension Education Program guidelines, the 2011 UK guidelines, the 2014 American Society of Hypertension (ASH)/International Society of Hypertension (ISH) guidelines, and the 2015 AHA/ACC/ASH scientific statement on treatment of hypertension in patients with coronary artery disease. I support these guidelines. In adults aged 80 years and older, a blood pressure below 150/90 mm Hg has been recommended by these guidelines, with a target goal of less than 140/90 mmHg considered in those with diabetes mellitus or chronic kidney disease. I support these guidelines. The 2013 JNC 8 guidelines recommend reducing the blood pressure to less than 140/90 mmHg in adults aged 60 years and older with diabetes mellitus or chronic kidney disease but to less than 150/90 mmHg in adults aged 60 years and older without diabetes mellitus or chronic kidney disease. I strongly disagree with this recommendation and am very much concerned that the higher systolic blood pressure goal recommended by JNC 8 guidelines in adults aged 60 years and older without diabetes mellitus or chronic kidney disease will lead to an increase in cardiovascular events and mortality in these adults.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57:2037–114. These guidelines recommend that the systolic blood pressure be reduced to less than 140 mm Hg in adults aged 60–79 years and to 140 to 145 mm Hg if tolerated in adults aged 80 years and older.
Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics-2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181.
Aronow WS, Ahmed MI, Ekundayo OJ, et al. A propensity-matched study of the association of PAD with cardiovascular outcomes in community-dwelling older adults. Am J Cardiol. 2009;103:130–5.
Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–72.
Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 Report. JAMA. 2003;289:2560–72.
Rosendorff C, Black HR, Cannon CP, et al. Treatment of hypertension in the prevention and management of ischemic heart disease. A scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115:2761–88.
Aronow WS. Hypertension guidelines. Hypertension. 2011;58:347–8.
Bangalore S, Qin J, Sloan S, et al. What is the optimal blood pressure in patients after acute coronary syndromes? relationship of blood pressure and cardiovascular events in the pravastatin or atorvastatin evaluation and infection therapy-thrombolysis in myocardial infarction (PROVE IT-TIMI) 22 trial. Circulation. 2010;122:2142–51.
Cooper-DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304:61–8.
The ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85.
Redon J, Mancia G, Sleight P, et al. Safety and efficacy of low blood pressures among patients with diabetes. Subgroup analyses from the ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial). J Am Coll Cardiol. 2012;59:74–83.
Mancia G, Schumacher H, Redon J, et al. Blood pressure targets recommended by guidelines and incidence of cardiovascular and renal events in the Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial (ONTARGET). Circulation. 2011;124:1727–36.
Appel LJ, Wright Jr JT, Greene T, et al. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010;363:918–29.
Lazarus JM, Bourgoignie JJ, Buckalew VM, et al. Achievement and safety of a low blood pressure goal in chronic renal disease: the Modification of Diet in Renal Disease Study Group. Hypertension. 1997;29:641–50.
Ruggenenti P, Perna A, Loriga G, et al. Blood-pressure control for renoprotection in patients with nondiabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet. 2005;365:939–46.
Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann Intern Med. 2011;154:541–8.
Banach M, Bhatia V, Feller MA, et al. Relation of baseline systolic blood pressure and long-term outcomes in ambulatory patients with chronic mild to moderate heart failure. Am J Cardiol. 2011;107:1208–14.
Ovbiagele B, Diener H-C, Yusuf S, et al. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA. 2011;306:2137–44.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265:3255–64.
Perry Jr HM, Davis BR, Price TR, et al. Effect of treating isolated systolic hypertension on the risk of developing various types and subtypes of stroke. The Systolic Hypertension in the Elderly Program (SHEP). JAMA. 2000;284:465–71.
Kostis JB, Davis BR, Cutler J, et al. Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. JAMA. 1997;278:212–6.
Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Eng J Med. 2008;358:1887–98.
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219. These guidelines recommend reducig the systolic blood pressure to less than 140 mm Hg in adults aged 60 to 79 years and in adults aged 80 years and older with a systolic blood pressure of 160 mm Hg or higher to between 140–150 mm Hg provided they are in good physical and mental conditions.
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20. These guidelines recommend reducing the systolic blood pressure in persons aged 60 years or older to less than 150 mm Hg if they do not have diabetes mellitus or chronic kidney disease and to less than 140 mm Hg if they have diabetes mellitus or chronic kidney disease.
Wright Jr JT, Fine LJ, Lackland DT, et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160:499–503. This minority report from JNC8 recommends that the systolic blood pressure goal in persons aged 60 to 79 years with hypertension without diabetes mellitus or chronic kidney disease should be reduced to less than 140 mm Hg.
Navar-Boggan AM, Pencina MJ, Williams K, et al. Proportion of US adults potentially affected by the 2014 hypertension guideline. JAMA. 2014;311:1424–9.
Banach M, Bromfield S, Howard G, et al. Association of systolic blood pressure levels with cardiovascular events and all-cause mortality among older adults taking antihypertensive medication. Int J Cardiol. 2014;176:219–26.
Bangalore S, Gong Y, Cooper-DeHoff RM, et al. 2014 Eighth Joint National Committee Panel recommendation for blood pressure targets revisited: results from the INVEST study. J Am Coll Cardiol. 2014;64:784–93.
Krakoff LR, Gillespie RL, Ferdinand KC, et al. 2014 hypertension recommendations from the eighth joint national committee panel members raise concerns for elderly black and female populations. J Am Coll Cardiol. 2014;64:394–402. The Association of Black Cardiologists and the Working Group on Women’s Cardiovascular Health support a systolic blood pressure goal of less than 140 mm Hg in persons aged 60 to 79 years and of less than 150 mm Hg in debilitated or frail persons aged 80 years and older.
National Institute for Health and Clinical Excellence. Hypertension: clinical management of primary hypertension in adults. London: National Institute for Health and Clinical Excellence; 2011. These guidelines recommend reducing the systolic blood pressure to less than 140 mm Hg in adults younger than 80 years.
Hackam DG, Quinn RR, Ravani P, et al. The 2013 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2013;29:528–42. These guidelines recommend decreasing the systolic blood pressure to less than 140 mm Hg in adults s younger than 80 years of age and to less than 150 mm Hg in adults aged 80 years and older.
Weber MA, Schiffrin EL White WB, et al. Clinical practice guidelines for the management of hypertension in the community. A statement by the American Society of Hypertension and the International Society of Hypertension. 2014;16:14–26. These guidelines recommend reducing the blood pressure to less than 140/90 mm Hg in adults aged 80 years and younger and to less than 150/90 mm Hg in adults older than 80 years unless these persons have diabetes mellitus or chronic kidney disease when a target goal of less than 140/90 mm Hg should be considered.
Rosendorff C, Lackland DT, Allison M, Aronow WS, et al. AHA/ACC/ASH scientific statement. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Circulation. 2015. doi:10.1161/CIR.0000000000000207. These guidelines recommend that the optimal blood pressure in adults with coronary artery disease is less than 140/90 mm Hg.
Midgley JP, Matthew AG, Greenwood CM, Logan AG. Effect of reduced dietary sodium on blood pressure: a meta-analysis of randomized controlled trials. JAMA. 1996;275:1590–7.
Cook NR, Cutler JA, Obarzanek E, et al. Long-term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007;334:885–8.
Chang HY, Hu YW, Yue CS, et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr. 2006;83:1289–96.
Karppanen H, Mervaala E. Prog Cardiovasc Dis. 2006;49:59–75.
Yang Q, Liu T, Kuklina EV, et al. Sodium and potassium intake and mortality among US adults: prospective data from the third national health and nutrition examination survey. Arch Intern Med. 2011;171:1183–91.
He FJ, Pombo-Rodrigues S, Macgregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014;4, e004549. doi:10.1136/bmjopen-2013-004549.
US Department of Health and Human Services and US Department of Agriculture. Dietary guidelines for Americans. 6th ed. Washington DC: US Government Printing Office; 2005. January, 2005.
Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi:10.1136/bmj.b1665.
Aronow WS. Might losartan reduce sudden cardiac death in diabetic patients with hypertension? Lancet. 2003;362:591–2.
Carlberg B, Samuelson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet. 2004;364:1684–9.
Aronow WS. Current role of beta blockers in the treatment of hypertension. Expert Opin Pharmacother. 2010;11:2599–607.
Aronow WS. Multiple blood pressure medications and mortality among elderly individuals. JAMA. 2015;313:1362–3.
Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE study. JAMA Intern Med. 2014. doi:10.1001/jamainternmed. 8012.
Banach M, Aronow WS. Blood pressure J curve. Curr Hypertens Rep. 2012;14:556–66.
Chiong JR, Aronow WS, Khan IA, et al. Secondary hypertension: current diagnosis and treatment. Int J Cardiol. 2008;124:6–21.
ASTRAL Investigators, Wheatley K, Ives N, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009;361:1953–62.
Bax L, Woittiez AJ, Kouwenberg HJ, et al. Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med. 2009;150:840–8.
Cooper CJ, Murphy TP, Cutlip DE, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370:13–22.
Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–26.
Myat A, Redwood SR, Quereshi AC, et al. Resistant hypertension. BMJ. 2012;345, e7473. doi:10.1136/bmj.e7473 (published 20 November 2012).
Pimenta E, Calhoun DA. Resistant hypertension. Incidence, prevalence, and prognosis. Circulation. 2012;125:1594–6.
Gandelman G, Aronow WS, Varma R. Prevalence of adequate blood pressure control in self-pay or medicare patients versus medicaid or private insurance patients with systemic hypertension followed in a university cardiology or general medicine clinic. Am J Cardiol. 2004;94:815–6.
Chapman N, Dobson J, Wilson S, et al. Effect of spironolactone on blood pressure in subjects with resistant hypertension. Hypertension. 2007;49:839–45.
Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension. Durability of blood pressure reduction out to 24 months. Hypertension. 2011;57:911–7.
Esler MD, Krum H, Schlaich M, et al. Renal sympathetic denervation for treatment of drug-resistant hypertension: one-year results from the Symplicity HTN-2 randomized, controlled trial. Circulation. 2012;126:2976–82.
Davis MI, Filion KB, Zhang D, et al. Effectiveness of renal denervation therapy for resistant hypertension. J Am Coll Cardiol. 2013;62:231–41.
Schlaich MP, Schmieder RE, Bakris G, et al. International expert consensus statement. Percutaneous transluminal renal denervation for the treatment of resistant hypertension. J Am Coll Cardiol. 2013;62:2031–45.
Bhatt DL, Kandzari DE, O’Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:393–401.
Bakris GL, Townsend RR, Liu M, et al. Impact of renal denervation on 24-hour ambulatory blood pressure: results from SYMPLICITY HTN-3. J Am Coll Cardiol. 2014;64:1071–8.
Bakris GL, Townsend RR, Flack JM, et al. 12-month blood pressure results of catheter-based renal artery denervation for resistant hypertension: the SYMPLICITY HTN-3 trial. J Am Coll Cardiol. 2015;65:1314–21.
Compliance with Ethics Guidelines
Conflict of Interest
Wilbert S. Aronow declares no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Prevention
Rights and permissions
About this article
Cite this article
Aronow, W.S. Blood Pressure Goals and Targets in the Elderly. Curr Treat Options Cardio Med 17, 33 (2015). https://doi.org/10.1007/s11936-015-0394-x
Published:
DOI: https://doi.org/10.1007/s11936-015-0394-x