Abstract
Purpose
Metabolic Syndrome (MetS) is more predominant in overweight, obese and minority populations. This study examined the prevalence of MetS in an exclusively African-American (AA) cohort of breast cancer (BC) survivors; an underrepresented group in previous studies demonstrating negative BC outcomes disparities for females with MetS.
Methods
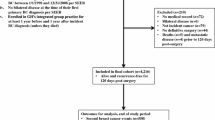
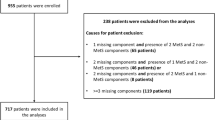
Using a case-control design, overweight/obese AA women with treated Stage I–IIIa BC were matched 1:1 on age, race, sex, and body mass index (BMI) category with non-cancer population controls (n = 444). Three of the following conditions were used to define MetS: HDL cholesterol <50 mg/dL (1.3 mmol/L), serum triglycerides ≥150 mg/dL (1.7 mmol/L), blood glucose ≥100 mg/dL (or on treatment), waist circumference ≥88 cm, or ≥130 mmHg systolic or ≥85 mmHg diastolic blood pressure (or on treatment). Matched-pairs analyses were conducted.
Results
For BC cases, most women had self-reported Stage I (n = 76) or Stage II (n = 91) disease and were 6.9 (±5.2) years post-diagnosis. MetS was significantly lower in BC survivors vs. their non-cancer population controls (43.2 vs. 51.4 %, respectively; p < 0.05). The diagnosis of MetS did not differ by BMI stratification. A lower prevalence of ≥2 risk factors (80.2 vs. 85.6 %, p < 0.05) was observed for all cases vs. controls.
Conclusions
While MetS occurred less frequently in our BC cases vs. non-cancer controls, our estimates are nearly two times those reported in other BC survivors, suggesting important racial/ethnic differences.
Implications for cancer survivors
The prognostic implications of MetS among AA BC survivors remain unknown and warrant further investigation.
Similar content being viewed by others
References
DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, et al. Cancer statistics for African Americans, 2016: progress and opportunities in reducing racial disparities. CA Cancer J Clin. 2016. doi:10.3322/caac.21340.
American Cancer Society Cancer Facts and Figures 2016. http://www.cancer.org. Accessed 5 Feb. 2016.
Akinyemiju T, Moore JX, Ojesina AI, Waterbor JW, Altekruse SF. Racial disparities in individual breast cancer outcomes by hormone-receptor subtype, area-level socio-economic status and healthcare resources. Breast Cancer Res Treat. 2016;157(3):575–86. doi:10.1007/s10549-016-3840-x.
Hirschman J, Whitman S, Ansell D. The black:white disparity in breast cancer mortality: the example of Chicago. Cancer Causes Control. 2007;18(3):323–33. doi:10.1007/s10552-006-0102-y.
Orsi JM, Margellos-Anast H, Whitman S. Black-white health disparities in the United States and Chicago: a 15-year progress analysis. Am J Public Health. 2010;100(2):349–56. doi:10.2105/AJPH.2009.165407.
Reeder-Hayes KE, Wheeler SB, Mayer DK. Health disparities across the breast cancer continuum. Semin Oncol Nurs. 2015;31(2):170–7. doi:10.1016/j.soncn.2015.02.005.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7. doi:10.1001/jama.2012.39.
Chan DS, Vieira AR, Aune D, Bandera EV, Greenwood DC, McTiernan A, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol. 2014;25(10):1901–14. doi:10.1093/annonc/mdu042.
Kwan ML, Chen WY, Kroenke CH, Weltzien EK, Beasley JM, Nechuta SJ, et al. Pre-diagnosis body mass index and survival after breast cancer in the after breast cancer pooling project. Breast Cancer Res Treat. 2012;132(2):729–39. doi:10.1007/s10549-011-1914-3.
NIH. National Heart, Lung and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/ms/. Accessed 12 Nov. 2015.
Sung KC, Ryu S, Cheong ES, Kim BS, Kim BJ, Kim YB, et al. All-cause and cardiovascular mortality among Koreans: effects of obesity and metabolic health. Am J Prev Med. 2015;49(1):62–71. doi:10.1016/j.amepre.2015.02.010.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356–9.
Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003;163(4):427–36.
Bhandari R, Kelley GA, Hartley TA, Rockett IR. Metabolic syndrome is associated with increased breast cancer risk: a systematic review with meta-analysis. Int J Breast Cancer. 2014;2014:189384. doi:10.1155/2014/189384.
Berrino F, Villarini A, Traina A, Bonanni B, Panico S, Mano MP, et al. Metabolic syndrome and breast cancer prognosis. Breast Cancer Res Treat. 2014;147(1):159–65. doi:10.1007/s10549-014-3076-6.
CDC. Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf. Accessed 13 Nov. 2015.
CDC. Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/BP.pdf. Accessed November 15 2015.
CDC. Centers for Disease Control and Prevention. 2007. http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/hdl_d_met_cholesterol_hdl_h717.pdf. Accessed 17 Nov. 2015.
CDC. Centers for Disease Control and Prevention. 2011. http://www.cdc.gov/nchs/nhanes/nhanes2009–2010/TRIGLY_F.htm. Accessed 11 November 2015.
CDC. Centers for Disease Control and Prevention. 2007. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/glu_e_met_fasting_glucose_ModP.pdf. Accessed 15 Nov. 2015.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112(17):2735–52. doi:10.1161/CIRCULATIONAHA.105.169404.
National Cholesterol Education Program Expert Panel. On detection E, treatment of high blood cholesterol in a. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002;106(25):3143–421.
Calip GS, Malone KE, Gralow JR, Stergachis A, Hubbard RA, Boudreau DM. Metabolic syndrome and outcomes following early-stage breast cancer. Breast Cancer Res Treat. 2014;148(2):363–77. doi:10.1007/s10549-014-3157-6.
Colonna SV, Douglas Case L, Lawrence JA. A retrospective review of the metabolic syndrome in women diagnosed with breast cancer and correlation with estrogen receptor. Breast Cancer Res Treat. 2012;131(1):325–31. doi:10.1007/s10549-011-1790-x.
Vona-Davis L, Howard-McNatt M, Rose DP. Adiposity, type 2 diabetes and the metabolic syndrome in breast cancer. Obes Rev. 2007;8(5):395–408. doi:10.1111/j.1467-789X.2007.00396.x.
Esposito K, Chiodini P, Capuano A, Bellastella G, Maiorino MI, Rafaniello C, et al. Metabolic syndrome and postmenopausal breast cancer: systematic review and meta-analysis. Menopause. 2013;20(12):1301–9. doi:10.1097/GME.0b013e31828ce95d.
Rose DP, Haffner SM, Baillargeon J. Adiposity, the metabolic syndrome, and breast cancer in African-American and white American women. Endocr Rev. 2007;28(7):763–77.
McTiernan A, Rajan KB, Tworoger SS, Irwin M, Bernstein L, Baumgartner R, et al. Adiposity and sex hormones in postmenopausal breast cancer survivors. J Clin Oncol. 2003;21(10):1961–6. doi:10.1200/jco.2003.07.057.
Stephenson GD, Rose DP. Breast cancer and obesity: an update. Nutrition & Cancer. 2003;45(1):1–16.
Goodwin PJ, Ennis M, Pritchard KI, Trudeau ME, Koo J, Madarnas Y, et al. Fasting insulin and outcome in early-stage breast cancer: results of a prospective cohort study. J Clin Oncol. 2002;20(1):42–51. doi:10.1200/jco.20.1.42.
Blackburn GL, Wang KA. Dietary fat reduction and breast cancer outcome: results from the Women's Intervention Nutrition Study (WINS). Am J Clin Nutr. 2007;86(3):878S–1.
Pierce BL, Ballard-Barbash R, Bernstein L, Baumgartner RN, Neuhouser ML, Wener MH, et al. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J Clin Oncol. 2009;27(21):3437–44. doi:10.1200/jco.2008.18.9068.
Bosco JL, Antonsen S, Sorensen HT, Pedersen L, Lash TL. Metformin and incident breast cancer among diabetic women: a population-based case-control study in Denmark. Cancer Epidemiol Biomark Prev. 2011;20(1):101–11. doi:10.1158/1055-9965.EPI-10-0817.
Goodwin PJ, Stambolic V. Obesity and insulin resistance in breast cancer—chemoprevention strategies with a focus on metformin. Breast. 2011;20(Suppl 3):S31–5. doi:10.1016/S0960-9776(11)70291-0.
DeCensi A, Puntoni M, Gandini S, Guerrieri-Gonzaga A, Johansson HA, Cazzaniga M, et al. Differential effects of metformin on breast cancer proliferation according to markers of insulin resistance and tumor subtype in a randomized presurgical trial. Breast Cancer Res Treat. 2014;148(1):81–90. doi:10.1007/s10549-014-3141-1.
Wensveen FM, Valentic S, Sestan M, Turk Wensveen T, Polic B. The “Big Bang” in obese fat: events initiating obesity-induced adipose tissue inflammation. Eur J Immunol. 2015;45(9):2446–56. doi:10.1002/eji.201545502.
Britton KA, Massaro JM, Murabito JM, Kreger BE, Hoffmann U, Fox CS. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol. 2013;62(10):921–5. doi:10.1016/j.jacc.2013.06.027.
Katzmarzyk PT, Bray GA, Greenway FL, Johnson WD, Newton Jr RL, Ravussin E, et al. Racial differences in abdominal depot-specific adiposity in white and African American adults. Am J Clin Nutr. 2010;91(1):7–15. doi:10.3945/ajcn.2009.28136.
Hunter GR, Chandler-Laney PC, Brock DW, Lara-Castro C, Fernandez JR, Gower BA. Fat distribution, aerobic fitness, blood lipids, and insulin sensitivity in African-American and European-American women. Obesity (Silver Spring). 2010;18(2):274–81. doi:10.1038/oby.2009.229.
Liu J, Coady S, Carr JJ, Hoffmann U, Taylor HA, Fox CS. Differential associations of abdominal visceral, subcutaneous adipose tissue with cardiometabolic risk factors between African and European Americans. Obesity (Silver Spring). 2014;22(3):811–8. doi:10.1002/oby.20307.
Bruno E, Gargano G, Villarini A, Traina A, Johansson H, Mano MP, et al. Adherence to WCRF/AICR cancer prevention recommendations and metabolic syndrome in breast cancer patients. Int J Cancer. 2016;138(1):237–44. doi:10.1002/ijc.29689.
Acknowledgments
We would like to thank the women who participated in the Moving Forward weight loss intervention for their commitment to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no conflict of interests to disclose regarding the conduct and report of this work.
Funding
National Institute on Aging, Midwest Roybal Center for Health Promotion and Translation (P30AG022849); National Cancer Institute, Moving Forward (R01CA154406); National Cancer Institute, Cancer Education and Career Development Program (R25CA057699).
Rights and permissions
About this article
Cite this article
Sheean, P., Liang, H., Schiffer, L. et al. Examining the prevalence of metabolic syndrome among overweight/obese African-American breast cancer survivors vs. matched non-cancer controls. J Cancer Surviv 11, 102–110 (2017). https://doi.org/10.1007/s11764-016-0566-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-016-0566-z