Abstract
Purpose
The purpose of this study is to investigate provider specialty, care coordination, and cancer survivors’ comorbid condition care.
Methods
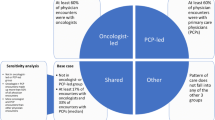
This retrospective cross-sectional Surveillance, Epidemiology, and End Results (SEER)-Medicare study included cancer survivors diagnosed in 2004, 2–3 years post-cancer diagnosis, in fee-for-service Medicare. We examined (1) provider specialties (primary care providers (PCPs), oncology specialists, other specialists) visited post-hospitalization, (2) role of provider specialties in chronic and acute condition management, and (3) an ambulatory care coordination measure. Outcome measures covered (1) visits post-hospitalization for nine conditions, (2) chronic disease management (lipid profile, diabetic eye exam, diabetic monitoring), and (3) acute condition management (electrocardiogram (EKG) for congestive heart failure (CHF), imaging for CHF, EKG for transient ischemic attack, cholecystectomy, hip fracture repair).
Results
Among 8661 cancer survivors, patients were more likely to visit PCPs than oncologists or other specialists following hospitalizations for 8/9 conditions. Patients visiting a PCP (vs. not) were more likely to receive recommended care for 3/3 chronic and 1/5 acute condition indicators. Patients visiting a nother specialist (vs. not) were more likely to receive recommended care for 3/3 chronic and 2/5 acute condition indicators. Patients visiting an oncology specialist (vs. not) were more likely to receive recommended care on 2/3 chronic indicators and less likely to receive recommended care on 1/5 acute indicators. Patients at greatest risk for poor coordination were more likely to receive appropriate care on 4/6 indicators.
Conclusions
PCPs are central to cancer survivors’ non-cancer comorbid condition care quality.
Implications for Cancer Survivors
PCP involvement in cancer survivors’ care should be promoted.


Similar content being viewed by others
References
American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2012–2013. Atlanta, GA: American Cancer Society; 2012.
Rowland JH, Mariotto A, Alfano CM, Pollack LA, Weir HK, White A. Cancer survivors—United States, 2007. MMWR. 2011;60:269–72.
Institute of Medicine. From cancer patient to cancer survivor: lost in transition. Washington, DC: National Academy Press; 2006.
Armes J, Crowe M, Colbourne L, et al. Patients’ supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009 20;27:6172–9.
Aaronson NK, Mattioli V, Minton O, et al. Beyond treatment—psychosocial and behavioural issues in cancer survivorship research and practice. Eur J Cancer Suppl. 2014;12:54–64.
Earle CC, Burstein HJ, Winer EP, Weeks JC. Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003;21:1447–51.
Earle CC, Neville BA. Under use of necessary care among cancer survivors. Cancer. 2004;101:1712–9.
Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Trends in follow-up and preventive care for colorectal cancer survivors. J Gen Intern Med. 2008;23:254–9.
Snyder CF, Frick KD, Peairs KS, et al. Comparing care for breast cancer survivors to non-cancer controls: a five-year longitudinal study. J Gen Intern Med. 2009;24:469–74.
Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Preventive care for colorectal cancer survivors: a 5-year longitudinal study. J Clin Oncol. 2008;26:1073–9.
Snyder CF, Frick KD, Kantsiper ME, et al. Prevention, screening, and surveillance care for breast cancer survivors compared with controls: changes from 1998 to 2002. J Clin Oncol. 2009;27:1054–61.
Snyder CF, Frick KD, Herbert RJ, et al. Preventive care in prostate cancer patients: following diagnosis and for five-year survivors. J Cancer Surviv. 2011;5:283–91.
Khan NF, Mant D, Rose PW. Quality of care for chronic diseases in a British cohort of long-term cancer survivors. Ann Fam Med. 2010;8:418–24.
Salz T, Weinberger M, Ayanian JZ, et al. Variation in use of surveillance colonoscopy among colorectal cancer survivors in the United States. BMC Health Services Research. 2010;10:256.
Cheung WY, Neville BA, Cameron DB, Cook EF, Earle CC. Comparison of patient and physician expectations for cancer survivorship care. J Clin Oncol. 2009;27:2489–95.
Hudson SV, Miller SM, Hemler J, et al. Adult cancer survivors discuss follow-up in primary care: ‘not what I want, but maybe what I need.’. Ann Fam Med. 2012;10:418–27.
Kantsiper M, McDonald EL, Geller G, Shockney L, Snyder C, Wolff AC. Transitioning to breast cancer survivorship: perspectives of patients, cancer specialists, and primary care providers. J Gen Intern Med. 2009;24:459–66.
Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: findings from a population-based sample. J Natl Cancer Inst. 2004;96:1322–30.
Hanrahan EO, Gonzalez-Angulo AM, Giordano SH, et al. Overall survival and cause-specific mortality of patients with stage T1a, bN0M0 breast carcinoma. J Clin Oncol. 2007;25:4952–60.
Patnaik JL, Byers T, DiGuiseppi C, Denberg TD, Dabelea D. The influence of comorbidities on overall survival among older women diagnosed with breast cancer. J Natl Cancer Inst. 2011;103:1101–11.
Kaiser Family Foundation. Medicare: A Primer, 2007. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/7615lp.pdf. Accessed February 4, 2015.
Kaiser Family Foundation. Medicare: A Primer, 2010. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/7615-03.pdf. Accessed February 4, 2015.
Asch SM, Sloss EM, Hogan C, Brook RH, Kravitz RL. Measuring underuse of necessary care among elderly Medicare beneficiaries using inpatient and outpatient claims. JAMA. 2000;284:2325–33.
National Cancer Institute. SEER-Medicare: brief description of the SEER-Medicare database. http://healthservices.cancer.gov/seermedicare/overview/brief.html. Accessed November 21, 2014.
The Johns Hopkins ACG® System. Technical Reference Guide. Version 10.0. http://acg.jhsph.org/public-docs/ACGv10.0TechRefGuide.pdf. Accessed November 21, 2014.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–67.
Rosenblatt RA, Hart LG, Baldwin L-M, Chan L, Schneeweiss R. The generalist role of specialty physicians: is there a hidden system of primary care? JAMA. 1998;279:1364–70.
Snyder CF, Frick KD, Herbert RJ, et al. Quality of care for comorbid conditions during the transition to survivorship: differences between cancer survivors and non-cancer controls. J Clin Oncol. 2013;31:1140–8.
McDonald KM, Sundaram V, Bravata DM, et al. Closing the quality gap: a critical analysis of quality improvement strategies. Technical Review 9 (prepared by the Stanford University-UCSF Evidence-based Practice Center under contract 290-02-0017). AHRQ Publication No. 04(07)-0051-7. Rockville, MD: Agency for Healthcare Research and Quality; 2007.
Sarfati D. Review of methods used to measure comorbidity in cancer populations: no gold standard exists. J Clin Epidemiol. 2012;65:924–33.
Acknowledgment
The project described was supported by Award Number R01CA149616 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. The findings have been presented in part at the 2012 Annual Meeting of the Society for General Internal Medicine, the 2012 Annual Meeting of the American Society of Clinical Oncology, and the 2012 Biennial Cancer Survivorship Conference. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database. The collection of the California cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract N01-PC-35136 awarded to the Northern California Cancer Center, contract N01-PC-35139 awarded to the University of Southern California, and contract N02-PC-15105 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement #U55/CCR921930-02 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health, the National Cancer Institute, and the Centers for Disease Control and Prevention, or their contractors and subcontractors are not intended nor should be inferred.
Conflict of interest
Dr. Lemke is a member of a group of faculty and staff at The Johns Hopkins University who develop and maintain the Adjusted Clinical Group (ACG) method. The Johns Hopkins University holds the copyright to the ACG software. To help support research and development, The Johns Hopkins University receives royalties from health plans and other organizations that license the ACG software. Dr. Frick consulted for and sits on a medical advisory board for eviti, a company that provides a service to determine whether a recommended cancer treatment regiment is consistent with evidence as reported in the literature or other guidelines and is consistent with insurers’ payment plans. No other authors have relevant conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Snyder, C.F., Frick, K.D., Herbert, R.J. et al. Comorbid condition care quality in cancer survivors: role of primary care and specialty providers and care coordination. J Cancer Surviv 9, 641–649 (2015). https://doi.org/10.1007/s11764-015-0440-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-015-0440-4