Abstract
Purpose
This study sought to evaluate the accuracy of vacuum-assisted biopsy (VAB) in the diagnosis of atypical ductal hyperplasia (ADH) by determining the rate of VAB underestimation compared with definitive histology. In addition, an attempt was made to identify parameters that could help determine the most appropriate patient management.
Materials and methods
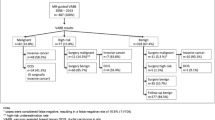
We retrospectively reviewed 1,776 VAB procedures performed between November 1999 and January 2008 for suspicious subclinical breast lesions visible only at mammography. A total of 177 patients with a VAB diagnosis of pure ADH were studied. Patients with a diagnosis of ADH associated with other lesions (lobular intraepithelial neoplasia, papilloma), atypical lobular hyperplasia, lobular carcinoma in situ and any lesions with a microhistological diagnosis other than ADH were excluded. Mammographic appearance of lesions was as follows: 152 mostly clustered microcalcifications (86%); five opacities with microcalcifications (3%); 12 single opacities (3%); and eight parenchymal distortions (4%), of which five were without and three were with microcalcifications. In cases underestimated by VAB, we evaluated the extent of ADH within ducts and lobules. Based on results, patients were subdivided into two groups: ≤2 ADH foci; >2 ADH foci. Patients were subdivided into two groups: one was referred for surgery and the other for follow-up care. The decision to either perform or not perform surgery was based on combined analysis of the following parameters: patient age; risk factors in the patient’s history; mammographic extent of microcalcifications; complete excision of microcalcifications at VAB; and final Breast Imaging Reporting and Data System (BI-RADS) assessment.
Results
In the first group (n=98), comparison of microhistology with final histology revealed that 19 cases of ADH had been underestimated by VAB. In the second group (n=79), six cases of ADH showed progression of the mammographic abnormality, which was subsequently confirmed by surgical biopsy.
Conclusions
The most relevant parameters affecting the decision to proceed to surgical excision were lesion diameter >7 mm on mammography, >2 ADH foci, incomplete removal of the calcifications and a family and/or personal history of breast cancer. Although there are no definite mammographic predictors of malignancy, a radiological assessment of suspicious lesion in the presence of an additional equivocal parameter always warrants surgical management.
Riassunto
Obiettivo
Scopo del nostro lavoro è stato valutare l’accuratezza della vaccum assisted biopsy (VAB) nella diagnosi di iperplasia duttale atipica (ADH), individuando le sottostime della metodica rispetto all’esame istologico definitivo ed identificare parametri utili al corretto management delle pazienti.
Materiali e metodi
È stata effettuata un’analisi retrospettiva di 1776 VAB per lesioni mammarie sospette infracliniche, visibili solo alla mammografia, eseguite da novembre 1999 a gennaio 2008. Sono state incluse nel nostro studio 177 pazienti con diagnosi VAB di ADH pura; sono state escluse le pazienti con diagnosi di ADH associata ad altre lesioni (neoplasia intraepiteliale lobulare [LIN], papilloma), iperplasia lobulare atipica (ALH), carcinoma lobulare in situ (LCIS) e tutti le lesioni con diagnosi microistologiche differenti. La tipologia mammografica di tali lesioni è stata la seguente: 152 microcalcificazioni per la maggior parte in cluster (86%); 5 opacità con microcalcificazioni (3%); 12 opacità singole (3%); infine, 8 distorsioni parenchimali (4%) di cui 5 senza microcalcificazioni e 3 con microcalcificazioni. Nei casi sottostimati è stata valutata l’estensione dell’ADH all’interno dei dotti e dei lobuli dividendo le pazienti in due gruppi: ADH≤2 foci, ADH>2 foci. Le pazienti sono state suddivise in due gruppi: uno inviato ad intervento chirurgico e l’altro monitorato nel tempo. La decisione d’inviare o meno la paziente ad intervento chirurgico si è basata sull’analisi combinata dei seguenti parametri: età della paziente, eventuali fattori di rischio anamnestici, estensione mammografica delle microcalcificazioni, completa exeresi delle microcalcificazioni alla VAB e giudizio breast imaging reporting and data system (BIRADS) radiologico espresso.
Risultati
Nel primo gruppo (n=98), il confronto tra microistologia bioptica e istologia definitiva ha individuato 19 casi di ADH sottostimati dalla VAB. Nel secondo gruppo (n=79), 6 casi di ADH hanno mostrato un’evoluzione del quadro mammografico, poi confermato dalla biopsia chirurgica.
Conclusioni
Dai dati emersi nel nostro studio i parametri più rilevanti per la decisione all’exeresi della lesione sono stati: diametro mammografico>7 mm, estensione dell’ADH>2 foci, incompleta rimozione delle calcificazioni ed anamnesi familiare e/o personale di neoplasia. Sebbene non vi siano caratteristiche mammografiche predittive di malignità certa, un giudizio radiologico sospetto, in presenza di un ulteriore parametro dubbio, dovrebbe comunque indirizzare all’exeresi.
Similar content being viewed by others
References/Bibliografia
Ciatto S, Cataliotti L, Distante V (1987) Non palpable lesions detected with mammography: review of 52 consecutive cases. Radiology 65:99–102
Cosmo C (2007) Recenti acquisizioni terapeutiche sul carcinoma iniziale della mammella. L’internistica 15:107–117
Lagios MD (1990) Ductal carcinoma in situ: pathology and treatment. Surg Clin N Am 70:853–871
Tavassoli FA (2000) Ductal Intraepithelial neoplasia (IDH, AIDH and DCIS). Breast Cancer 7:315–320
Kettritz U, Morach G, Decker T (2004) Stereotassic vacuum-assisted breast biopsies in 500 women with microcalcifications: radiological and pathological correlations. Eur J Radiol 55:270–276
Orel SG, Kay N, Reynolds C et al (1999) BI-RADS categorization as a predictor of malignancy. Radiology 211:845–850
Heywang-Kobrunner SH, Schaumloffel U, Viehweg P et al (1998) Minimally invasive stereotaxic vacuum core breast biopsy. Eur Rad 8:377–385
Lippman M (2002) Why study ductal carcinoma in-situ? In: Silverstein MJ, Recht A, Lagios M (eds) Ductal carcinoma in-situ of the breast, 2nd edn. Lippincott, William and Wilkins, Philadelphia, pp 12–16
Veronesi U (1999) Senologia oncologica. Masson Editore, Milano
Philpotts LE, Shaheen NA, Carter D et al (1999) Analysis of cancer not diagnosed at stereotactic core needle biopsy of the breast with 11-gauge vacuum suction probe versus 14-gauge needle automatic gun. Am J Roentgenol 172:683–687
Burbank F, Parker SH, Fogarty TJ (1996) Stereotactic breast biopsy: improved tissue harvesting with the Mammotome. Am Surg 62:738–744
Dalstrom JE, Sutton S, Jain S (1996) Histological precision of stereotactic core biposy in diagnosis of malignant and premalignant breast lesions. Histopathology 28:537–541
Jackman RJ, Nowels KW, Rodriguez-Soto J et al (1999) Stereotassic, automated, large-core needle biopsy of nonpalpable breast lesionS: falsenegative and histologic inderstimation rates after long-term follow-up. Radiology 210:799–805
Jackaman RJ, Nowels KW, Shepard MJ et al (1994) Stereotaxic large-core needle biopsy of 450 nonpalpable breast lesions with surgical corerlation in lesion with cancer or atipica hyperplasia. Radiology 193:91–95
Liberman L, Cohen MA, Deshaw DD et al (1995) Atypical ductal hyperplasia diagnosed at stereotaxic core biopsy of breast lesions: an indication for surgical biopy. AJR Am J Roentgenol 164:1111–1113
Darling ML, Smith DN, Lester SC et al (2000) Atypical ductal hyperplasia and ductal carcinoma in situ as revealed by large-core needle breast biopsy: results of surgical excision. AJR Am J Roentgenol 175:1341–1346
Moore MM, Hargett CW, Hanks JB et al (1997) Association of breast with the finding of atipica ductal hyperplasia at core biopsy. Ann Surg 225:726–731
Jackaman RJ, Birdwell RL, Ikeda DM (2002) Atipica ductal hyperplasia: can some lesions be defined as probably benign after stereotactic 11-gauge vaccum-assisted biopsy, eliminating the raccomandation for surgical excision? Radiology 224:548–554
Plantade R, Hammou JC, Fighera M et al (2004) Understimation of breast carcinoma with 11-gauge stereotactically guided directional vacuum-assisted biopsy. J Radiol 85:391–401
Sneige N, Lim SC, Whitman GJ et al (2003) Atypical ductal hyperplasia: diagnosis by directional vacuumassisted stereotactic biopsy of breast microcalcifications. Considerations for surgical excision. Am J Clin Pathol 119:248–253
Adrales G, Turk P, Wallace T et al (2000) Is surgical excision necessary for ductal hyperplasia of the breast diagnosed by Mammotome? Am J Surg 180:33–35
Kettritz U, Rotter K, Schreer I et al (2004) Stereotactic vacuum-assisted breast biopsy in 2874 patients: a multi center study. Cancer 100:245–251
Megha J, Audrey DF, Ram P et al (2001) Atypical ductal hyperplasia in steretactic breast biopsies: enhanced accuracy of diagnosis with the Mammotome. Breast J 4:207–213
Winchester DJ, Bernestein JR, Jeske JM et al (2003) Upstaging of atypical ductal hyperplasia after vacuumassisted 11-gauge stereotactic core needle biopsy. Arch Surg 138:619–622
Burak WE Jr, Owens KE, Tighe MB et al (2000) Vacuum-assisted stereotactic breast biopsy: histologic understimation of malignant lesions. Arch Surg 135:700–703
Pandelidis S, Heiland D, Jones D et al (2003) Accuracy of 11-gauge vacuumassisted core biopsy of mammographics breast lesions. Ann Surg Oncol 10:43–47
Vance S, Zachary A, Garth H et al (2007) Atypical ductal hyperplasia: improved accuracy with the 11-gauge vacuum-assisted versus the 14-gauge core biopsy needle. Breast Oncology 14:2497–2501
Tonegutti M, Girardi V (2008) Stereotactic vacuum-assisted breast biopsy in 268 non palpable lesions. Radiol Med 113:65–75
Travade A, Isnard A, Bouchet F et al (2006) Non-palpable breast lesions and core needle biopsy with Mammotome 11 G: is surgery required in patients with atypical ductal hyperplasia? J Radiol 87:307–310
Ely KA, Carter BA, Jensen RA et al (2001) Core biopsy of the breast with atypical ductal hyperplasia: a probabilistic approach to reporting. Am J Surg Pathol 25:1017–1021
Philpotts LE, Lee CH, Horvath LJ et al (2000) Understimation of breast cancer with II-gauge vacuum suction biopsy. AJR Am J Roentgenol 175:1047–1050
Liberman L, Smolkin JH, Dershaw DD et al (1998) Calcification retrieval at stereotactic, 11-gauge, directtional, vacuum-assisted breast biopsy. Radiology 208:251–260
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ancona, A., Capodieci, M., Galiano, A. et al. Vacuum-assisted biopsy diagnosis of atypical ductal hyperplasia and patient management. Radiol med 116, 276–291 (2011). https://doi.org/10.1007/s11547-011-0626-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-011-0626-9