Abstract
Purpose
The content validity of patient-reported outcomes (PROs) commonly used to measure postoperative recovery is unknown. The objective of this study was to develop a conceptual framework for recovery after abdominal surgery and to analyze the content of PRO instruments against this conceptual framework.
Methods
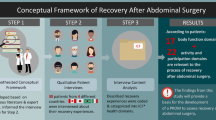
Qualitative methods were used to develop a conceptual framework for recovery. Patients undergoing abdominal surgery and healthcare professionals were interviewed. Recovery-related concepts were identified using a thematic analysis, and concepts were then linked to the International Classification of Functioning, Disability and Health (ICF). The contents of eight PRO instruments that have been used to measure recovery were then examined using this conceptual framework.
Results
A total of 17 patients and 15 healthcare professionals were interviewed. A total of 22 important recovery-related concepts were identified and linked to the ICF. The four most important concepts were “Energy level,” “Sensation of pain,” “General physical endurance,” and “Carrying out daily routine.” The number of important recovery-related concepts covered by each instrument ranged from 1 to 22 (mean 7.3 concepts). The SF36 (n = 22), European Organization for the Treatment and Research of Cancer Quality-of-Life Questionnaire-C30 (n = 20), and the Gastrointestinal Quality-of-Life Index (n = 19) covered the greatest number of important recovery concepts. No instrument covered all of the important concepts.
Conclusions
The comparison of the contents of PRO instruments commonly used to measure postoperative recovery after abdominal surgery demonstrated major gaps in the representation of concepts that are important to patients and healthcare professionals.
Similar content being viewed by others
References
Lee, L., Tran, T., Mayo, N. E., Carli, F., & Feldman, L. S. (2014). What does it really mean to “recover” from an operation? Surgery, 155(2), 211–216.
Neville, A., Lee, L., Antonescu, I., Mayo, N. E., Vassiliou, M. C., Fried, G. M., & Feldman, L. S. (2014). Systematic review of outcomes used to evaluate enhanced recovery after surgery. British Journal of Surgery, 101(3), 159–171.
Miller, T. E., Thacker, J. K., White, W. D., Mantyh, C., Migaly, J., Jin, J., et al. (2014). Reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesthesia and Analgesia, 118(5), 1052–1061.
Ljungqvist, O., & Rasmussen, L. S. (2014). Recovery after anaesthesia and surgery. Acta Anaesthesiologica Scandinavica, 58(6), 639–641.
Patrick, D. L., Burke, L. B., Powers, J. H., Scott, J. A., Rock, E. P., Dawisha, S., et al. (2007). Patient-reported outcomes to support medical product labeling claims: FDA perspective. Value Health, 10(Suppl 2), S125–S137.
Dowson, H. M., Cowie, A. S., Ballard, K., Gage, H., & Rockall, T. A. (2008). Systematic review of quality of life following laparoscopic and open colorectal surgery. Colorectal Disease, 10(8), 757–768.
Khan, S., Wilson, T., Ahmed, J., Owais, A., & MacFie, J. (2010). Quality of life and patient satisfaction with enhanced recovery protocols. Colorectal Disease, 12(12), 1175–1182.
Bartels, S. A., Vlug, M. S., Ubbink, D. T., & Bemelman, W. A. (2010). Quality of life after laparoscopic and open colorectal surgery: A systematic review. World Journal of Gastroenterology, 16(40), 5035–5041.
Strauss, A. L. (1987). Qualitative analysis for social scientists. New York: Cambridge University Press.
Glaser, B. G., & Strauss, A. L. (1967). The discovery of grounded theory: Strategies for qualitative research. New York: Aldine Press.
World Health Organization. (2001). International classification of functioning, disability and health: ICF. Geneva: WHO.
Stucki, G., Cieza, A., Ewert, T., Kostanjsek, N., Chatterji, S., & Ustun, T. B. (2002). Application of the international classification of functioning, disability and health (ICF) in clinical practice. Disability and Rehabilitation, 24(5), 281–282.
Weigl, M., Cieza, A., Harder, M., Geyh, S., Amann, E., Kostanjsek, N., & Stucki, G. (2003). Linking osteoarthritis-specific health-status measures to the international classification of functioning, disability, and health (ICF). Osteoarthritis Cartilage, 11(7), 519–523.
Geyh, S., Cieza, A., Kollerits, B., Grimby, G., & Stucki, G. (2007). Content comparison of health-related quality of life measures used in stroke based on the international classification of functioning, disability and health (ICF): A systematic review. Quality of Life Research, 16(5), 833–851.
Tschiesner, U., Rogers, S. N., Harreus, U., Berghaus, A., & Cieza, A. (2008). Content comparison of quality of life questionnaires used in head and neck cancer based on the international classification of functioning, disability and health: A systematic review. European Archives of Oto-Rhino-Laryngology, 265(6), 627–637.
Cieza, A., Brockow, T., Ewert, T., Amman, E., Kollerits, B., Chatterji, S., et al. (2002). Linking health-status measurements to the international classification of functioning, disability and health. Journal of Rehabilitation Medicine, 34(5), 205–210.
Cieza, A., Geyh, S., Chatterji, S., Kostanjsek, N., Ustun, B., & Stucki, G. (2005). ICF linking rules: An update based on lessons learned. Journal of Rehabilitation Medicine, 37(4), 212–218.
Spitzer, W. O., Dobson, A. J., Hall, J., Chesterman, E., Levi, J., Shepherd, R., et al. (1981). Measuring the quality of life of cancer patients: A concise QL-index for use by physicians. Journal of Chronic Diseases, 34(12), 585–597.
Myles, P. S., Hunt, J. O., Nightingale, C. E., Fletcher, H., Beh, T., Tanil, D., et al. (1999). Development and psychometric testing of a quality of recovery score after general anesthesia and surgery in adults. Anesthesia and Analgesia, 88(1), 83–90.
Fazio, V. W., O’Riordain, M. G., Lavery, I. C., Church, J. M., Lau, P., Strong, S. A., & Hull, T. (1999). Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Annals of Surgery, 230(4), 575–584.
Ware, J. E, Jr, & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Eypasch, E., Williams, J. I., Wood-Dauphinee, S., Ure, B. M., Schmulling, C., Neugebauer, E., & Troidl, H. (1995). Gastrointestinal quality of life index: Development, validation and application of a new instrument. British Journal of Surgery, 82(2), 216–222.
EuroQol Group. (1990). EuroQol—A new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208.
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European organization for research and treatment of cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85(5), 365–376.
Paddison, J. S., Sammour, T., Kahokehr, A., Zargar-Shoshtari, K., & Hill, A. G. (2011). Development and validation of the surgical recovery scale (SRS). Journal of Surgical Research, 167(2), e85–e91.
Dindo, D., Demartines, N., & Clavien, P. A. (2004). Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery, 240(2), 205–213.
Rothman, M., Burke, L., Erickson, P., Leidy, N. K., Patrick, D. L., & Petrie, C. D. (2009). Use of existing patient-reported outcome (PRO) instruments and their modification: The ISPOR good research practices for evaluating and documenting content validity for the use of existing instruments and their modification PRO task force report. Value Health, 12(8), 1075–1083.
Lee, L., Elfassy, N., Li, C., Latimer, E., Liberman, A. S., Charlebois, P., et al. (2013). Valuing postoperative recovery: Validation of the SF-6D health-state utility. Journal of Surgical Research, 184(1), 108–114.
Urbach, D. R., Harnish, J. L., & Long, G. (2005). Short-term health-related quality of life after abdominal surgery: A conceptual framework. Surgical Innovation, 12(3), 243–247.
Allvin, R., Berg, K., Idvall, E., & Nilsson, U. (2007). Postoperative recovery: A concept analysis. Journal of Advanced Nursing, 57(5), 552–558.
Mayo, N. E., Moriello, C., Asano, M., van der Spuy, S., & Finch, L. (2011). The extent to which common health-related quality of life indices capture constructs beyond symptoms and function. Quality of Life Research, 20(5), 621–627.
Kluivers, K. B., Riphagen, I., Vierhout, M. E., Brolmann, H. A., & de Vet, H. C. (2008). Systematic review on recovery specific quality-of-life instruments. Surgery, 143(2), 206–215.
Food and Drug Administration. (2009). Guidance for industry—Patient-reported outcome measures: Use in medical product development to support labeling claims. U.S. Department of Health and Human Services. http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf. Accessed October 11, 2013.
Lee, L., Mata, J., Augustin, B. R., Carli, F., Morin, N., Latimer, E., & Feldman, L. S. (2014). A comparison of the validity of two indirect utility instruments as measures of postoperative recovery. Journal of Surgical Research, 190(1), 79–86.
Hobart, J. C., Cano, S. J., Zajicek, J. P., & Thompson, A. J. (2007). Rating scales as outcome measures for clinical trials in neurology: Problems, solutions, and recommendations. Lancet Neurology, 6(12), 1094–1105.
Acknowledgments
LL is supported by the Quebec Health Sciences Research Fund (FRQS) and the Fast Foundation.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, L., Dumitra, T., Fiore, J.F. et al. How well are we measuring postoperative “recovery” after abdominal surgery?. Qual Life Res 24, 2583–2590 (2015). https://doi.org/10.1007/s11136-015-1008-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-1008-5