Abstract
Background
It is unclear whether the quality of bowel preparation affects colonoscopic detection of non-polypoid colorectal neoplasms (NP-CRNs).
Aim
To evaluate the impact of bowel-cleansing quality on detection of NP-CRNs.
Methods
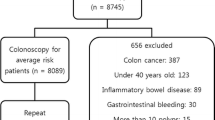
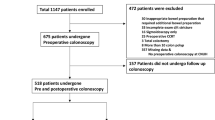
We performed a retrospective analysis of asymptomatic screening colonoscopy cases after standardized bowel preparation at an academic teaching hospital between June 2011 and May 2013. Primary outcome was a comparison of the adenoma detection rate (ADR) of non-polypoid morphology according to quality of bowel preparation. Secondary outcomes included detection prevalence of non-polypoid adenomas.
Results
Of the enrolled 6097 screening examinations, the preparation quality was rated as adequate (excellent or good) in 5224 (85.7 %), fair in 615 (10.1 %), and poor in 258 (4.2 %) patients. The prevalence of NP-CRNs was 40.5 % (1962/4847) of all CRNs. The overall ADR of non-polypoid morphology was 12.3 % (747/6097) of all colonoscopies, but it significantly differed among participating endoscopists (all P < 0.05). The ADR of non-polypoid morphology was significantly lower with fair- or poor-quality preparation, versus adequate-quality preparation (adjusted odds ratio [aOR] 0.55, 95 % confidence interval [CI] 0.41–0.75; aOR 0.49, 95 % CI 0.30–0.79, respectively). Poor-quality preparation was also associated with impaired detection of polypoid, proximal colon, and sub-centimeter adenomas (all P < 0.05).
Conclusions
Suboptimal (fair or poor) bowel preparation significantly impairs colonoscopic detection of NP-CRNs. Given that the prevalence of NP-CRNs is substantial in our average-risk screening cohort, ongoing efforts to improve the preparation quality are practically valuable in increasing the detection of NP-CRNs, thereby improving the efficacy of screening colonoscopies.

Similar content being viewed by others
References
Baxter NN, Warren JL, Barrett MJ, Stukel TA, Doria-Rose VP. Association between colonoscopy and colorectal cancer mortality in a US cohort according to site of cancer and colonoscopist specialty. J Clin Oncol. 2012;30:2664–2669.
Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154:22–30.
Nishihara R, Wu K, Lochhead P, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095–1105.
Ness RM, Manam R, Hoen H, Chalasani N. Predictors of inadequate bowel preparation for colonoscopy. Am J Gastroenterol. 2001;96:1797–1802.
Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003;58:76–79.
Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005;61:378–384.
le Clercq CM, Bouwens MW, Rondagh EJ, et al. Postcolonoscopy colorectal cancers are preventable: a population-based study. Gut. 2014;63:957–963.
Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Am J Gastroenterol. 2015;110:72–90.
Soetikno RM, Kaltenbach T, Rouse RV, et al. Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults. JAMA. 2008;299:1027–1035.
Ignjatovic A, Saunders BP. Non-polypoid colorectal neoplasms are relatively common worldwide. Gastrointest Endosc Clin N Am. 2010;20:417–429.
Kim HN, Raju GS. Bowel preparation and colonoscopy technique to detect non-polypoid colorectal neoplasms. Gastrointest Endosc Clin N Am. 2010;20:437–448.
Rondagh EJ, Bouwens MW, Riedl RG, et al. Endoscopic appearance of proximal colorectal neoplasms and potential implications for colonoscopy in cancer prevention. Gastrointest Endosc. 2012;75:1218–1225.
Tadepalli US, Feihel D, Miller KM, et al. A morphologic analysis of sessile serrated polyps observed during routine colonoscopy (with video). Gastrointest Endosc. 2011;74:1360–1368.
Rex DK, Hewett DG, Snover DC. Editorial: detection targets for colonoscopy: from variable detection to validation. Am J Gastroenterol. 2010;105:2665–2669.
Kudo SE, Kashida H. Flat and depressed lesions of the colorectum. Clin Gastroenterol Hepatol. 2005;3:S33–S36.
Kubota O, Kino I, Kimura T, Harada Y. Nonpolypoid adenomas and adenocarcinomas found in background mucosa of surgically resected colons. Cancer. 1996;77:621–626.
Lee SK, Kim TI, Shin SK, Kim WH, Kim H, Kim NK. Comparison of the clinicopathologic features between flat and polypoid adenoma. Scand J Gastroenterol. 2008;43:1116–1121.
Park DH, Kim HS, Kim WH, et al. Clinicopathologic characteristics and malignant potential of colorectal flat neoplasia compared with that of polypoid neoplasia. Dis Colon Rectum. 2008;51:43–49.
Jaramillo E, Slezak P, Watanabe M, Rubio C. Endoscopic detection and complete removal of a micro-invasive carcinoma present in a flat colonic adenoma. Gastrointest Endosc. 1994;40:369–371.
Fujii T, Rembacken BJ, Dixon MF, Yoshida S, Axon AT. Flat adenomas in the United Kingdom: are treatable cancers being missed? Endoscopy. 1998;30:437–443.
Rembacken BJ, Fujii T, Cairns A, et al. Flat and depressed colonic neoplasms: a prospective study of 1000 colonoscopies in the UK. Lancet. 2000;355:1211–1214.
Tsuda S, Veress B, Toth E, Fork FT. Flat and depressed colorectal tumours in a southern Swedish population: a prospective chromoendoscopic and histopathological study. Gut. 2002;51:550–555.
Lanspa SJ, Rouse J, Smyrk T, Watson P, Jenkins JX, Lynch HT. Epidemiologic characteristics of the flat adenoma of Muto. A prospective study. Dis Colon Rectum. 1992;35:543–546.
Saitoh Y, Waxman I, West AB, et al. Prevalence and distinctive biologic features of flat colorectal adenomas in a North American population. Gastroenterology. 2001;120:1657–1665.
Kahi CJ, Hewett DG, Rex DK. Relationship of non-polypoid colorectal neoplasms to quality of colonoscopy. Gastrointest Endosc Clin N Am. 2010;20:407–415.
Aronchick CA, Lipshutz WH, Wright SH, Dufrayne F, Bergman G. A novel tableted purgative for colonoscopic preparation: efficacy and safety comparisons with Colyte and Fleet Phospho-Soda. Gastrointest Endosc. 2000;52:346–352.
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58:S3–S43.
Bosman FTCF, Hruban RH, Theise ND. WHO Classification of Tumours of the Digestive System. 4th ed. Berlin: Springer; 2010.
Sherer EA, Imler TD, Imperiale TF. The effect of colonoscopy preparation quality on adenoma detection rates. Gastrointest Endosc. 2012;75:545–553.
Anderson JC, Butterly LF, Robinson CM, Goodrich M, Weiss JE. Impact of fair bowel preparation quality on adenoma and serrated polyp detection: data from the New Hampshire Colonoscopy Registry by using a standardized preparation-quality rating. Gastrointest Endosc. 2014;80:463–470.
Lebwohl B, Kastrinos F, Glick M, Rosenbaum AJ, Wang T, Neugut AI. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc. 2011;73:1207–1214.
Menees SB, Kim HM, Elliott EE, Mickevicius JL, Graustein BB, Schoenfeld PS. The impact of fair colonoscopy preparation on colonoscopy use and adenoma miss rates in patients undergoing outpatient colonoscopy. Gastrointest Endosc. 2013;78:510–516.
MacPhail ME, Hardacker KA, Tiwari A, Vemulapalli KC, Rex DK. Intraprocedural cleansing work during colonoscopy and achievable rates of adequate preparation in an open-access endoscopy unit. Gastrointest Endosc. 2015;81:525–530.
Leung FW, Harker JO, Jackson G, et al. A proof-of-principle, prospective, randomized controlled trial (RCT) demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700.
Hsieh YH, Koo M, Leung FW. A patient-blinded randomized, controlled trial (RCT) comparing air insufflation (AI), water immersion (WI) and water exchange (WE) during minimally sedated colonoscopy. Am J Gastroenterol. 2014;109:1390–1400.
Bucci C, Rotondano G, Hassan C, et al. Optimal bowel cleansing for colonoscopy: split the dose! A series of meta-analyses of controlled studies. Gastrointest Endosc. 2014;80:566–576.
Matro R, Shnitser A, Spodik M, et al. Efficacy of morning-only compared with split-dose polyethylene glycol electrolyte solution for afternoon colonoscopy: a randomized controlled single-blind study. Am J Gastroenterol. 2010;105:1954–1961.
Wexner SD, Beck DE, Baron TH, et al. A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Gastrointest Endosc. 2006;63:894–909.
Hassan C, Bretthauer M, Kaminski MF, et al. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy.. 2013;45:142–150.
Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US multi-society task force on colorectal cancer. Gastroenterology. 2014;147:903–924.
Reinhart K, Bannert C, Dunkler D, et al. Prevalence of flat lesions in a large screening population and their role in colonoscopy quality improvement. Endoscopy. 2013;45:350–356.
Chiu HM, Lin JT, Chen CC, et al. Prevalence and characteristics of nonpolypoid colorectal neoplasm in an asymptomatic and average-risk Chinese population. Clin Gastroenterol Hepatol. 2009;7:463–470.
Sanduleanu S, Rondagh EJ, Masclee AA. Development of expertise in the detection and classification of non-polypoid colorectal neoplasia: experience-based data at an academic GI unit. Gastrointest Endosc Clin N Am. 2010;20:449–460.
de Wijkerslooth TR, Stoop EM, Bossuyt PM, et al. Differences in proximal serrated polyp detection among endoscopists are associated with variability in withdrawal time. Gastrointest Endosc. 2013;77:617–623.
Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69:620–625.
Calderwood AH, Jacobson BC. Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc. 2010;72:686–692.
Conflict of interest
The authors disclosed no financial relationships relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oh, C.H., Lee, C.K., Kim, JW. et al. Suboptimal Bowel Preparation Significantly Impairs Colonoscopic Detection of Non-polypoid Colorectal Neoplasms. Dig Dis Sci 60, 2294–2303 (2015). https://doi.org/10.1007/s10620-015-3628-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3628-6