Abstract
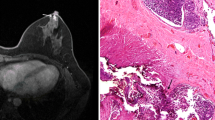
The sub-nipple tissue (SNT) examination has been used by surgeons to preserve, or not, the nipple in nipple-sparing mastectomy. However, it is uncertain whether SNT evaluation can predict nipple involvement. The aim of this study was to evaluate the accuracy, sensitivity, specificity, PPV, and NPV of the intraoperative frozen section and imprint cytology, and permanent histology of SNT to predict the involvement of the nipple in breast carcinoma and to compare the three exams. A prospective study was performed with 68 consecutive breast carcinoma women who had undergone mastectomy or central segmentectomy (removing nipple-areolar complex). After surgery, the nipple-areolar complex was dissected simulating a nipple-sparing flap (ex vivo). The SNT was subsequently removed and submitted to frozen section, imprint cytology, and permanent histology. The nipple was examined separately by paraffin histopathology and was considered the gold standard. The occult nipple involvement rate was 11.7 %. The frozen section, cytology, and permanent histology of SNT presented accuracy 86.8, 76.5, and 86.8 %; sensitivity 50, 37.5, and 62.5 %; specificity 91.7, 81.7, and 90 %; PPV 44.4, 21.4, and 45.5 %; and NPV 93.2, 90.7, and 94.7 %, respectively. The accuracy of the frozen section was similar to that of permanent histology (p = 0.77) and both were better than cytology (p = 0.01). False negative rates were 6.8 % for frozen section, 9.3 % for cytology and 5.3 % for paraffin. SNT evaluation is a good method for predicting occult nipple involvement; the outcomes showed a good accuracy and low false negative rate for the frozen section, cytology, and permanent histology exams. When we compared the exams, the frozen section was similar to permanent histology and more accurate than imprint cytology.


Similar content being viewed by others
References
Gradishar JW, Anderson BO et al (2015) National Comprehensive Cancer Network—NCCN clinical practice guideline in oncology—breast cancer, version 2.2015, 20th edn. http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 1 April 2015
Freeman BS (1962) Subcutaneous mastectomy for benign breast lesions with immediate or delayed prosthetic replacement. Plast Reconstr Surg Transplant Bull 30:676–682
Toth BA, Lappert P (1991) Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg 87(6):1048–1053
Losken A, Carlson GW, Bostwick J, Jones GE, Culbertson JH, Schoemann M (2002) Trends in unilateral breast reconstruction and management of the contralateral breast: the Emory experience. Plast Reconstr Surg 110:89–97
Gerber B, Krause A, Reimer T, Muller H, Kuchenmeiser I, Makovitzky J et al (2003) Skin-sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction is an oncologically safe procedure. Ann Surg 238:102–107
Wilikins EG, Cederna PS, Lowery JC, Davis JA, Kim HM, Roth RS et al (2002) Prospective analysis of psychosocial outcomes in breast reconstruction: one year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 106:1014–1022
Petit JY, Veronesi U, Orecchia R, Rey P, Martella S, Didier F et al (2009) Nipple sparing mastectomy with nipple areola intraoperative radiotherapy: one thousand and one cases of a five years experience at the European institute of oncology of Milan (EIO). Breast Cancer Res Treat 117(2):333–338. doi:10.1007/s10549-008-0304-y
Cense HA, Rutgers EJ, Lopes Cardozo M, Van Lanschot JJ (2001) Nipple-sparing mastectomy in breast cancer: a viable option? Eur J Surg Oncol 27:521–526
Petit JY, Veronesi U, Orecchia R, Luini A, Rey P, Intra M et al (2006) Nipple-sparing mastectomy in association with intra operative radiotherapy (ELIOT): a new type of mastectomy for breast cancer treatment. Breast Cancer Res Treat 96:47–51
Munhoz AM, Aldrighi CM, Montag E, Arruda EG, Aldrighi JM, Gemperli R et al (2013) Clinical outcomes following nipple-areola-sparing mastectomy with immediate implant-based breast reconstruction: a 12-year experience with an analysis of patient and breast-related factors for complications. Breast Cancer Res Treat 140:545–555
Babiera G, Simmons R (2010) Nipple-areolar complex-sparing mastectomy: feasibility, patient selection, and technique. Ann Surg Oncol 17(Suppl 3):245–248
Stolier A, Stone JC, Moroz K, Hanemann CW, McNabb L, Jones SD, Lacey M (2013) A comparison of clinical and pathologic assessments for the prediction of occult nipple involvement in nipple-sparing mastectomies. Ann Surg Oncol 20(1):128–132. doi:10.1245/s10434-012-2511-3
Luo D, Ha J, Latham B, Ingram D, Connell T, Hastrich D et al (2010) The accuracy of intraoperative subareolar frozen section in nipple-sparing mastectomies. Ochsner J 10(3):188–192
Brachtel EF, Rusby JE, Michaelson JS, Chen LL, Muzikansky A, Smith BL, Koerner FC (2009) Occult nipple involvement in breast cancer: clinicopathologic findings in 316 consecutive mastectomy specimens. J Clin Oncol 27(30):4948–4954. doi:10.1200/JCO.2008.20.8785
Becker H, Billington ME (2014) A novel approach to the management of margin-positive DCIS in nipple-sparing mastectomy. Plast Reconstr Surg Global Open 2(11):e253. doi:10.1097/GOX.0000000000000189
Tomasović-Loncarić C, Milanović R, Lambasa S, Krizanac S, Stoos-Veić T, Kaić G, Ostović KT (2010) Intraoperative imprint cytological assessment of the subareolar tissue of the nipple areola complex (NAC). Coll Antropol 34(2):431–435
Li Weidong, Wang Shuling, Guo Xiaojing, Ronggang Lang Yu, Fan Feng Gu et al (2011) Nipple involvement in breast cancer: retrospective analysis of 2323 consecutive mastectomy specimens. Int J Surg Pathol 19(3):328–334. doi:10.1177/1066896911399279
Santini D, Taffurelli M, Gelli MC, Grassigli A, Giosa F, Marrano D, Martinelli G (1989) Neoplastic involvement of nipple-areolar complex in invasive breast cancer. Am J Surg 158:399–403
Wang J, Xiao X, Wang J, Iqbal N, Baxter L, Skinner KA et al (2012) Predictors of nipple-areolar complex involvement by breast carcinoma: histopathologic analysis of 787 consecutive therapeutic mastectomy specimens. Ann Surg Oncol 19:1174–1180
Pirozzi PR, Rossetti C, Carelli I, Ruiz CA, Pompei LM, Piato S (2010) Clinical and morphological factors predictive of occult involvement of the nipple-areola complex in mastectomy specimens. Eur J Obstet Gynecol Reprod Biol 148(2):177–181. doi:10.1016/j.ejogrb.2009.10.021
Byon W, Kim E, Kwon J, Park YL, Park C (2014) Magnetic resonance imaging and clinicopathological factors for the detection of occult nipple involvement in breast cancer patients. J Breast Cancer 17(4):386–392
Benediktsson KP, Perbeck L (2008) Survival in breast cancer after nipple-sparing subcutaneous mastectomy and immediate reconstruction with implants: a prospective trial with 13 years median follow-up in 216 patients. Eur J Surg Oncol 34:143–148
Camp MS, Coopey SB, Tang R, Colwell A, Specht M, Greenup RA et al (2014) Management of positive sub-areolar/nipple duct margins in nipple-sparing mastectomies. Breast J 20(4):402–407
Acknowledgments
This study was supported by São Paulo Research Foundation (FAPESP # 2013/03019-4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Duarte, G.M., Tomazini, M.V., Oliveira, A. et al. Accuracy of frozen section, imprint cytology, and permanent histology of sub-nipple tissue for predicting occult nipple involvement in patients with breast carcinoma. Breast Cancer Res Treat 153, 557–563 (2015). https://doi.org/10.1007/s10549-015-3568-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3568-z