Abstract
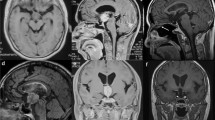
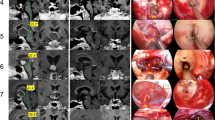
The third ventricle has historically represented one of the most challenging areas to access surgically, so that lesions directly harboring into the ventricular chamber or secondarily extending into it from adjacent areas have been approached by means of different transcranial routes. The aim of this work is to report our experience with the endoscopic endonasal approach in the management of a series of patients affected by craniopharyngiomas, extending into or arising from the third ventricle, evaluating pros and cons of this technique, also in regards of the anatomy and the pathology dealt with. During the period between January 2001 and February 2011, 12 patients, 9 male and 3 female (mean age 50.4 years; range 12-68) underwent an endoscopic endonasal approach for the treatment of a craniopharyngioma involving or arising from the third ventricle. According to the grade of involvement of the third ventricle, we identified three main ventricular growth patterns: (1) stalk–infundibulum; (2) infundibulum–ventricular chamber; (3) stalk–infundibulum–ventricular chamber. Though gross total removal was achieved in eight patients (66.7 %), in three patients (25 %) was possible a near total removal (>95 %) and only in one case (8.3 %) tumor removal has been partial (<50 %). The overall analysis revealed a rate of 77.8 % improvement of post-operative visual defects. Concerning the complications, we reported an overall CSF rate of 16.7 %; two patients developed a subdural hematoma that has been treated with a surgical drainage. One patient died after the occurrence of a brainstem hemorrhage. The endoscopic endonasal route provides a good exposure, especially of the sub- and retro-chiasmatic areas, as well as of the stalk–infundibulum axis, which represents, when directly involved by a lesion, a gate to access the third ventricle chamber. Despite this study reporting only a preliminary experience, it seems that in properly selected cases—namely tumors growing mostly along the pituitary stem–infundibulum–third ventricle axis—this approach could be advocated as a valid route among the wide kaleidoscope of surgical approaches to the third ventricle.







Similar content being viewed by others
References
Amar AP, Ghosh S, Apuzzo MLJ (2004) Ventricular tumors. In: Winn HR (ed) Youmans neurological surgery. WB Saunders, Philadelphia, pp 1237–1263
Apuzzo ML (1988) Surgery of masses affecting the third ventricular chamber: techniques and strategies. Clin Neurosurg 34:499–522
Apuzzo ML, Chikovani OK, Gott PS, Teng EL, Zee CS, Giannotta SL, Weiss MH (1982) Transcallosal, interfornicial approaches for lesions affecting the third ventricle: surgical considerations and consequences. Neurosurgery 10(5):547–554
Apuzzo MLJ, Litofsky NS (1993) Surgery in and aound the anterior third ventricle. In: Apuzzo MLJ (ed) Brain surgery. Churchill Livingstone, New York, pp 541–579
Cai R, Di X (2010) Combined intra- and extra-endoscopic techniques for aggressive resection of subependymal giant cell astrocytomas. World Neurosurg 73(6):713–718. doi:10.1016/j.wneu.2010.02.068
Cappabianca P, Cavallo LM, Esposito F, de Divitiis O, Messina A, de Divitiis E (2008) Extended endoscopic endonasal approach to the midline skull base: the evolving role of transsphenoidal surgery. In: Pickard JD, Akalan N, Di Rocco C et al (eds) Advances and technical standards in neurosurgery. Springer, Wien, pp 152–199
Cappabianca P, Cinalli G, Gangemi M, Brunori A, Cavallo LM, de Divitiis E, Decq P, Delitala A, Di Rocco F, Frazee J, Godano U, Grotenhuis A, Longatti P, Mascari C, Nishihara T, Oi S, Rekate H, Schroeder HW, Souweidane MM, Spennato P, Tamburrini G, Teo C, Warf B, Zymberg ST (2008) Application of neuroendoscopy to intraventricular lesions. Neurosurgery 62(Suppl 2):575–597. doi:10.1227/01.neu.0000316262.74843.dd, discussion 597–578
Cappabianca P, de Divitiis E (2004) Endoscopy and transsphenoidal surgery. Neurosurgery 54(5):1043–1048, discussions 1048–1050
Cappabianca P, Esposito F, Magro F, Cavallo LM, Solari D, Stella L, de Divitiis O (2010) Natura abhorret a vacuo—use of fibrin glue as a filler and sealant in neurosurgical "dead spaces". Technical note. Acta Neurochir (Wien) 152(5):897–904. doi:10.1007/s00701-009-0580-2
Cappabianca P, Frank G, Pasquini E, de Divitiis O, Calbucci F (2003) Extended endoscopic endonasal transsphenoidal approaches to the suprasellar region, planum sphenoidale and clivus. In: de Divitiis E, Cappabianca P (eds) Endoscopic endonasal transsphenoidal surgery. Springer, Wien, pp 176–187
Carmel PW (1985) Tumours of the third ventricle. Acta Neurochir (Wien) 75(1–4):136–146
Carrau RL, Jho HD, Ko Y (1996) Transnasal–transsphenoidal endoscopic surgery of the pituitary gland. Laryngoscope 106(7):914–918
Castelnuovo P, Locatelli D, Mauri S (2003) Extended endoscopic approaches to the skull base. Anterior cranial base CSF leaks. In: de Divitiis E, Cappabianca P (eds) Endoscopic endonasal transsphenoidal surgery. Springer, Wien, pp 137–158
Cavallo LM, de Divitiis O, Aydin S, Messina A, Esposito F, Iaconetta G, Talat K, Cappabianca P, Tschabitscher M (2007) Extended endoscopic endonasal transsphenoidal approach to the suprasellar area: anatomic considerations—part 1. Neurosurgery 61:ONS-24–ONS-34
Cavallo LM, Messina A, Esposito F, de Divitiis O, Dal Fabbro M, de Divitiis E, Cappabianca P (2007) Skull base reconstruction in the extended endoscopic transsphenoidal approach for suprasellar lesions. J Neurosurg 107(4):713–720
Cinalli G, Cappabianca P, de Falco R, Spennato P, Cianciulli E, Cavallo LM, Esposito F, Ruggiero C, Maggi G, de Divitiis E (2005) Current state and future development of intracranial neuroendoscopic surgery. Expert Rev Med Devices 2(3):351–373
Couldwell WT, Weiss MH, Rabb C, Liu JK, Apfelbaum RI, Fukushima T (2004) Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: surgical experience in 105 cases. Neurosurgery 55(3):539–550
de Divitiis E, Cappabianca P, Cavallo LM, Esposito F, de Divitiis O, Messina A (2007) Extended endoscopic transsphenoidal approach for extrasellar craniopharyngiomas. Neurosurgery 61(5 Suppl 2):219–227. doi:10.1227/01.neu.0000303220.55393.73, discussion 228
de Divitiis E, Cavallo LM, Cappabianca P, Esposito F (2007) Extended endoscopic endonasal transsphenoidal approach for the removal of suprasellar tumors: part 2. Neurosurgery 60(1):46–58, discussion 58-59
Delitala A, Brunori A, Chiappetta F (2004) Purely neuroendoscopic transventricular management of cystic craniopharyngiomas. Childs Nerv Syst 20(11–12):858–862. doi:10.1007/s00381-004-0943-1
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90(2):237–250
Fortes FS, Carrau RL, Snyderman CH, Kassam A, Prevedello D, Vescan A, Mintz A, Gardner P (2007) Transpterygoid transposition of a temporoparietal fascia flap: a new method for skull base reconstruction after endoscopic expanded endonasal approaches. Laryngoscope 117(6):970–976. doi:10.1097/MLG.0b013e3180471482
Fraioli B, Pastore FS, Floris R, Vagnozzi R, Simonetti G, Liccardo G, Giuffre R (1997) Computed tomography-guided transsphenoidal closure of postsurgical cerebrospinal fluid fistula: a transmucosal needle technique. Surg Neurol 48(4):409–412, discussion 412-403
Frank G, Pasquini E, Doglietto F, Mazzatenta D, Sciaretta V, Farneti G, Calbucci F (2006) The endoscopic extended transsphenoidal approach for craniopharyngiomas. Neurosurgery 59(suppl 1):ONS75–ONS83
Fukushima T, Hirakawa K, Kimura M, Tomonaga M (1990) Intraventricular craniopharyngioma: its characteristics in magnetic resonance imaging and successful total removal. Surg Neurol 33(1):22–27
Fukushima T, Ishijima B, Hirakawa K, Nakamura N, Sano K (1973) Ventriculofiberscope: a new technique for endoscopic diagnosis and operation. Technical note. J Neurosurg 38(2):251–256. doi:10.3171/jns.1973.38.2.0251
Gardner PA, Kassam AB, Snyderman CH, Carrau RL, Mintz AH, Grahovac S, Stefko S (2008) Outcomes following endoscopic, expanded endonasal resection of suprasellar craniopharyngiomas: a case series. J Neurosurg 109(1):6–16. doi:10.3171/JNS/2008/109/7/0006
Gardner PA, Prevedello DM, Kassam AB, Snyderman CH, Carrau RL, Mintz AH (2008) The evolution of the endonasal approach for craniopharyngiomas. J Neurosurg 108(5):1043–1047. doi:10.3171/JNS/2008/108/5/1043
Geffen G, Walsh A, Simpson D, Jeeves M (1980) Comparison of the effects of transcortical and transcallosal removal of intraventricular tumours. Brain 103(4):773–788
Gore PA, Nakaji P, Deshmukh V, Rekate HL (2006) Synchronous endoscopy and microsurgery: a novel strategy to approach complex ventricular lesions. Report of three cases. J Neurosurg 105(6 Suppl):485–489. doi:10.3171/ped.2006.105.6.485
Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A, Snyderman CH, Mintz A (2006) A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 116(10):1882–1886
Harris AE, Hadjipanayis CG, Lunsford LD, Lunsford AK, Kassam AB (2005) Microsurgical removal of intraventricular lesions using endoscopic visualization and stereotactic guidance. Neurosurgery 56(1 Suppl):125–132, discussion 125-132
Hori T, Kawamata T, Amano K, Aihara Y, Ono M, Miki N (2010) Anterior interhemispheric approach for 100 tumors in and around the anterior third ventricle. Neurosurgery 66(3 Suppl Operative):65–74. doi:10.1227/01.NEU.0000365550.84124.BB
Jane JA Jr, Prevedello DM, Alden TD, Laws ER Jr (2010) The transsphenoidal resection of pediatric craniopharyngiomas: a case series. J Neurosurg Pediatr 5(1):49–60. doi:10.3171/2009.7.PEDS09252
Jho HD (2001) The expanding role of endoscopy in skull-base surgery. Indications and instruments. Clin Neurosurg 48:287–305
Kasowski HJ, Nahed BV, Piepmeier JM (2005) Transcallosal transchoroidal approach to tumors of the third ventricle. Neurosurgery 57(4 Suppl):361–366, discussion 361-366
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL (2005) Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus 19(1):E3:1–E3:12
Kassam A, Thomas AJ, Snyderman C, Carrau R, Gardner P, Mintz A, Kanaan H, Horowitz M, Pollack IF (2007) Fully endoscopic expanded endonasal approach treating skull base lesions in pediatric patients. J Neurosurg 106(2 Suppl):75–86
Kassam AB, Gardner PA, Snyderman CH, Carrau RL, Mintz AH, Prevedello DM (2008) Expanded endonasal approach, a fully endoscopic transnasal approach for the resection of midline suprasellar craniopharyngiomas: a new classification based on the infundibulum. J Neurosurg 108(4):715–728. doi:10.3171/JNS/2008/108/4/0715
Kassam AB, Prevedello DM, Carrau RL, Snyderman CH, Thomas A, Gardner P, Zanation A, Duz B, Stefko ST, Byers K, Horowitz MB (2011) Endoscopic endonasal skull base surgery: analysis of complications in the authors' initial 800 patients. J Neurosurg 114(6):1544–1568. doi:10.3171/2010.10.JNS09406
Kassam AB, Prevedello DM, Thomas A, Gardner P, Mintz A, Snyderman C, Carrau R (2008) Endoscopic endonasal pituitary transposition for a transdorsum sellae approach to the interpeduncular cistern. Neurosurgery 62(3 Suppl 1):57–72. doi:10.1227/01.neu.0000317374.30443.23, discussion 72–74
Kassam AB, Thomas A, Carrau RL, Snyderman CH, Vescan A, Prevedello D, Mintz A, Gardner P (2008) Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap. Neurosurgery 63(1 Suppl 1):ONS44–ONS52. doi:10.1227/01.neu.0000335010.53122.75, discussion ONS52–ONS53
Konovalov AN, Gorelyshev SK (1992) Surgical treatment of anterior third ventricle tumours. Acta Neurochir (Wien) 118(1–2):33–39
Kunwar S (2003) Endoscopic adjuncts to intraventricular surgery. Neurosurg Clin N Am 14(4):547–557
Laws ER Jr (1994) Transsphenoidal removal of craniopharyngioma. Pediatr Neurosurg 21(Suppl 1):57–63
Laws ER, Kanter AS, Jane JA Jr, Dumont AS (2005) Extended transsphenoidal approach. J Neurosurg 102(5):825–827, discussion 827-828
Leng LZ, Brown S, Anand VK, Schwartz TH (2008) "Gasket-seal" watertight closure in minimal-access endoscopic cranial base surgery. Neurosurgery 62(5 Suppl 2):ONSE342–ONSE343. doi:10.1227/01.neu.0000326017.84315.1f, discussion ONSE343
Lewis AI, Crone KR, Taha J, van Loveren HR, Yeh HS, Tew JM Jr (1994) Surgical resection of third ventricle colloid cysts. Preliminary results comparing transcallosal microsurgery with endoscopy. J Neurosurg 81(2):174–178. doi:10.3171/jns.1994.81.2.0174
Locatelli D, Massimi L, Rigante M, Custodi V, Paludetti G, Castelnuovo P, Di Rocco C (2010) Endoscopic endonasal transsphenoidal surgery for sellar tumors in children. Int J Pediatr Otorhinolaryngol 74(11):1298–1302. doi:10.1016/j.ijporl.2010.08.009
Maira G, Anile C, Albanese A, Cabezas D, Pardi F, Vignati A (2004) The role of transsphenoidal surgery in the treatment of craniopharyngiomas. J Neurosurg 100(3):445–451
Prevedello DM, Doglietto F, Jane JA Jr, Jagannathan J, Han J, Laws ER Jr (2007) History of endoscopic skull base surgery: its evolution and current reality. J Neurosurg 107(1):206–213
Rhoton AL Jr (2002) The lateral and third ventricles. Neurosurgery 51(4 Suppl):S207–S271
Rosenfeld JV (2011) The evolution of treatment for hypothalamic hamartoma: a personal odyssey. Neurosurg Focus 30(2):E1
Rutka JT (2008) Endonasal resection of craniopharyngiomas. J Neurosurg 109(1):1. doi:10.3171/JNS/2008/109/7/0001, reply 3–5
Sainte-Rose C, Puget S, Wray A, Zerah M, Grill J, Brauner R, Boddaert N, Pierre-Kahn A (2005) Craniopharyngioma: the pendulum of surgical management. Childs Nerv Syst 21(8–9):691–695. doi:10.1007/s00381-005-1209-2
Samii M, Bini W (1991) Surgical treatment of craniopharyngiomas. Zentralbl Neurochir 52(1):17–23
Samii M, Samii A (2000) Surgical management of craniopharyngiomas. In: Schmidek HH (ed) Schmidek & Sweet operative neurosurgical techniques. Indications, methods and results, vol 1. WB Saunders, Philadelphia, pp 489–502
Seeger W (2006) Endoscopic anatomy of the third ventricle. Microsurgical and endoscopic approaches. Springer, Wien
Souweidane MM, Sandberg DI, Bilsky MH, Gutin PH (2000) Endoscopic biopsy for tumors of the third ventricle. Pediatr Neurosurg 33(3):132–137
Spaziante R, de Divitiis E (1997) Drainage techniques for cystic craniopharyngiomas. Neurosurg Quart 7:183–208
Steno J, Malacek M, Bizik I (2004) Tumor-third ventricular relationships in supradiaphragmatic craniopharyngiomas: correlation of morphological, magnetic resonance imaging, and operative findings. Neurosurgery 54(5):1051–1058, discussion 1058-1060
Wait SD, Abla AA, Killory BD, Nakaji P, Rekate HL (2011) Surgical approaches to hypothalamic hamartomas. Neurosurg Focus 30(2):E2
Weiss MH (1987) The transnasal transsphenoidal approach. In: Apuzzo MLJ (ed) Surgery of the third ventricle. Williams & Wilkins, Baltimore, pp 476–494
Wen HT, Rhoton AL Jr, de Oliveira E (1998) Transchoroidal approach to the third ventricle: an anatomic study of the choroidal fissure and its clinical application. Neurosurgery 42(6):1205–1217, discussion 1217–1209
Winkler PA, Ilmberger J, Krishnan KG, Reulen HJ (2000) Transcallosal interforniceal-transforaminal approach for removing lesions occupying the third ventricular space: clinical and neuropsychological results. Neurosurgery 46(4):879–888, discussion 888-890
Winkler PA, Weis S, Buttner A, Raabe A, Amiridze N, Reulen HJ (1997) The transcallosal interforniceal approach to the third ventricle: anatomic and microsurgical aspects. Neurosurgery 40(5):973–981, discussion 981–972
Woiciechowsky C, Vogel S, Lehmann R, Staudt J (1995) Transcallosal removal of lesions affecting the third ventricle: an anatomic and clinical study. Neurosurgery 36(1):117–122, discussion 122-113
Yasargil MG (1996) Craniopharyngiomas. In: Yasargil MG (ed) Microneurosurgery: microneurosurgery of CNS tumors, vol IV B. Thieme, Stuttgart
Yasargil MG, Abdulrauf SI (2008) Surgery of intraventricular tumors. Neurosurgery 62(6 Suppl 3):1029–1040. doi:10.1227/01.neu.0000333768.12951.9a, discussion 1040-1021
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Alvaro Campero and Abraham Agustín Campero, Tucumán, Argentina
The paper “The endoscopic endonasal approach for the management of craniopharyngiomas involving the third ventricle” is indeed well related to present day treatment of a very difficult surgical pathology: craniopharyngiomas affecting the third ventricle. Abstract is well summarized. Introduction guides us to a brief, as should be, historical background, pointing out differences between craniotomy, endonasal microscopic and endonasal endoscopic approaches; all of them are, of course, microsurgical in nature. Review of surgical operations carried out in a span of 10 years, with a total of 12 patients with craniopharyngiomas involved at different degrees the third ventricle, operated is large enough and really very comprehensive for what authors call a preliminary experience; besides, the technique applied was basically the same in every patient and lesions had different types of extensions in those areas. We find relevant to this kind of surgery the mention by the authors of Kassam very useful classification based upon the presence of craniopharyngiomas somewhere within the infundibulum, rather behind this most important structure either with rostral or caudal expansions, or even inside the third ventricle including its optic recess. Anatomy of the operating zone with emphasis on optic chiasm, pituitary stalk and mammillary bodies is well synthesized. Explanations regarding surgical anatomy, as observed after changes provoked by the expanding process, are also properly explained. Surgical technique has been expressed quite well including modern ways of avoiding CSF fistula among other complications. Conclusions are short, with each paragraph being self-explanatory and pointing out the anatomical limits as seen in the various pre-operative images for the strategy of this treatment. We consider this paper well written, easy to read, with every necessary detail properly explained which no doubt will be useful for both neurosurgeons and trainees; it is therefore an article worth publishing.
Giannantonio Spena and Marco Maria Fontanella, Brescia, Italy
In this paper, Cavallo et al. describe their experience with the endoscopic transsphenoidal resection of craniopharyngiomas (CPs). In these 12 patients, the authors achieved very good results in terms of extent of resection with a very large percentage of near total or gross total resection. Clinically, more than two thirds of the subjects improved their visual acuity. Although small, this series gives us the opportunity to make some surgical and technical consideration. First, the extensive experience of the authors in the field of transsphenoidal surgery made it possible to face such a complex and somewhat rare pathology. In fact, the “conditio sine qua non” to extirpate these CPs is that they must be located predominantly on the midline. In 2008, Kassam proposed a classification of these tumors (used in the current paper too) based on the relationship of the craniopharyngiomas with the infundibulum and indicating the transsphenoidal approach for the purely midline suprasellar craniopharyngiomas. Actually, the presence of a parasellar extension would make unsafe a single endonasal endoscopic approach, which rather would be better employed as the perfection of a transcranial route. Moreover, a favorable anatomy (a tumor that pushes the third ventricle toward the sella, a pre-fixed or anteriorly displaced chiasm, a very good pneumatization of the sphenoidal sinus in children) is mandatory for the safety and efficacy of such an approach. Taken together, all these conditions are rarely found and hence transsphenoidal route cannot be proposed routinely for CPs and selected Centers have to be detected in order to collect an increasing number of cases.
Concerning the complication rate, CSF fistulas are reported in 16.7 % of patients that globally seems not negligible. In that sense, the authors describe a technique of closure by using fibrin glue and other synthetic materials.
Cerebrospinal fluid leakage is an important problem in extended endoscopic approaches. In our opinion, most important points in closing the defect are using autogenic material such as fascia lata and mucosal flaps.
Deanna Sasaki-Adams, University of North Carolina in Chapel Hill, NC
Drs. Cavallo, Cappabianca, et al. have outlined their experience with the expanded endoscopic endonasal transphenoidal surgery for resection of craniopharyngiomas extending into the third ventricle over the past 10 years. Craniopharyngiomas are notoriously difficult tumors to treat with respect to embryology and intimate association with the pituitary neurohypophysis. Lesions residing within the third ventricle also pose a significant surgical challenge due to the close association with essential neurovascular structures and fiber tracts. In their series, gross total resection was achieved in two thirds of patients and near total resection in a quarter of patients. A near 80 % improvement was seen in visual defects and a CSF leak was identified in 16.7 % of patients. The sample size is small and so firm conclusions cannot be cemented. However, these tumors are challenging entities and the presented manuscript provides a welcome addition to the literature outlining the potential pitfalls as well as the benefits offered by this surgical route. As the endoscope becomes more firmly established in the neurosurgeon's armamentarium, reflecting on surgical outcomes and technique as the above paper describes will allow further advancement of this cadre of neurosurgery.
Rights and permissions
About this article
Cite this article
Cavallo, L.M., Solari, D., Esposito, F. et al. The endoscopic endonasal approach for the management of craniopharyngiomas involving the third ventricle. Neurosurg Rev 36, 27–38 (2013). https://doi.org/10.1007/s10143-012-0403-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0403-4