Abstract
Purpose
Although recommended as an essential part of cancer care, there is limited evidence regarding the optimum approach to psychosocial health care needs assessment in this setting. To address this gap, the Cancer Journey Action Group of the Canadian Partnership Against Cancer (CPAC) and the Canadian Association of Psychosocial Oncology (CAPO) partnered to develop consensus-based recommendations regarding the routine assessment of psychosocial and supportive care needs. The purpose of this paper is to summarize the evidence that informed the guideline and disseminate the recommendations developed by the expert panel.
Methods
Clinical practice recommendations were developed by a panel comprised of psychosocial and interdisciplinary experts. Recommendations were informed by a review of oncology clinical practice guidelines, systematic reviews, and primary research, through to May 2008. Following expert consensus on the recommendations, the clinical practice guideline was externally reviewed by a purposively selected sample of national and international interdisciplinary experts.
Results
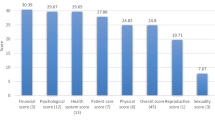
A total of nine clinical practice guidelines, three systematic reviews, and 14 primary studies were included in the review. Overall, this body of literature suggested that routine collection of psychosocial health care data has an influence on communication with oncologists and other study specific outcomes, but the evidence was limited by heterogeneity and methodological limitations. Based on the interpretation of this body of evidence by clinical experts, research methodologists, and external reviewers, 12 substantive recommendations were developed regarding the process and parameters of psychosocial needs assessment in adult cancer patients.
Conclusion
Given the limitations in the current body of evidence, there remains a need for rigorous empirical research regarding the optimal approach to psychosocial needs assessment, including the specific characteristics that influence effectiveness on patient outcomes. This guideline fills an important gap in psychosocial care, regarding the routine assessment of psychosocial health care needs.
Similar content being viewed by others
References
Ashbury FD, Findlay H, Reynolds B, McKerracher K (1998) A Canadian survey of cancer patients’ experiences: are their needs being met? J Pain Symptom Manage 16(5):298–306
Boberg EW, Gustafson DH, Hawkins RP, Offord KP, Koch C, Wen KY, Kreutz K, Salner A (2003) Assessing the unmet information, support and care delivery needs of men with prostate cancer. Patient Educ Couns 49(3):233–242
Gustafson DH, Taylor JO, Thompson S, Chesney P (1993) Assessing the needs of breast cancer patients and their families. Qual Manag Health Care 2(1):6–17
Richardson A, Sitzia J, Brown V, Medina J, Richardson A (2005) Patients’ needs assessment tools in cancer care: principles and practice. King’s College, London
Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P (2000) The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer 88(1):226–237. doi:10.1002/(SICI)1097-0142(20000101)88:1<226::AID-CNCR30>3.0.CO;2-P
Fitch M (1994) Provincial Cancer Network Supportive Care Work Group: Report and Recommendations. Submission to Cancer Care Ontario, Toronto
Richardson A, Medina J, Brown V, Sitzia J (2007) Patients’ needs assessment in cancer care: a review of assessment tools. Support Care Cancer 15(10):1125–1144. doi:10.1007/s00520-006-0205-8
Vachon M (2006) Psychosocial distress and coping after cancer treatment. Cancer Nurs 29(2 Suppl):26–31
Vachon ML (1998) Psychosocial needs of patients and families. J Palliat Care 14(3):49–56
Adler NE, Page AEK (eds) (2008) Cancer care for the whole patient: meeting psychosocial health needs. The National Academies Press, Washington
Wen KY, Gustafson DH (2004) Needs assessment for cancer patients and their families. Health Qual Life Outcomes 2:11. doi:10.1186/1477-7525-2-11
Canada A (2008) Qmentum program 2009 standards: cancer care and oncology services (ver 2). Ottawa, ON
National Comprehensive Cancer Network (2007) Distress management (v.1.2008). National Comprehensive Care Network, Inc. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 6 June 2008
National Breast Cancer Centre and National Cancer Control Initiative (2003) Clinical practice guidelines for the psychosocial care of adults with cancer. National Breast Cancer Centre, Camperdown
Fitch MI (2008) Supportive care framework: theoretical underpinnings. In: Fitch MI, Porter HB, Page BD (eds) Supportive care framework: a foundation for person-centred care. Pappin Communications, Pembroke
Holland JC, Alici Y (2010) Management of distress in cancer patients. J Support Oncol 8(1):4–12
Jacobsen PB, Ransom S (2007) Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw 5(1):99–103
Canadian Association of Psychosocial Oncology (1999) National Psychosocial Oncology Standards of Canada Canadian Association of Psychosocial Oncology. http://www.capo.ca. Accessed 8 June 2008
Gerteis M, Edgman-Levitan S, Daley J, Delbanco TL (eds) (1993) Through the patient’s eyes: understanding and promoting patient-centred care. Jossey-Bass, San Francisco
National Institute for Clinical Evidence (2004) Improving supportive and palliative care for adults with cancer: executive summary. National Institute for Clinical Evidence, London
ADAPTE Collaboration ADAPTE Framework. http://www.adapte.org/rubrique/adapte-framework.php. Accessed 22 July 2008
Appraisal of Guidelines for Research and Evaluation (AGREE) Collaboration Appraisal of guidelines for research and evaluation (AGREE) instrument. http://www.agreetrust.org/docs/AGREE_Instrument_English.pdf. Accessed 22 July 2008
Kristeller JL, Rhodes M, Cripe LD, Sheets V (2005) Oncologist Assisted Spiritual Intervention Study (OASIS): patient acceptability and initial evidence of effects. Int J Psychiatry Med 35(4):329–347
Bramsen I, van der Linden MH, Eskens FJ, Bijvank EM, van Groeningen CJ, Kaufman HJ, Aaronson NK (2008) Evaluation of a face-to-face psychosocial screening intervention for cancer patients: acceptance and effects on quality of life. Patient Educ Couns 70(1):61–68. doi:10.1016/j.pec.2007.09.010
Boyes A, Newell S, Girgis A, McElduff P, Sanson-Fisher R (2006) Does routine assessment and real-time feedback improve cancer patients’ psychosocial well-being? Eur J Cancer Care (Engl) 15(2):163–171. doi:10.1111/j.1365-2354.2005.00633.x
Detmar SB, Muller MJ, Schornagel JH, Wever LD, Aaronson NK (2002) Health-related quality-of-life assessments and patient-physician communication: a randomized controlled trial. JAMA 288(23):3027–3034
McLachlan SA, Allenby A, Matthews J, Wirth A, Kissane D, Bishop M, Beresford J, Zalcberg J (2001) Randomized trial of coordinated psychosocial interventions based on patient self-assessments versus standard care to improve the psychosocial functioning of patients with cancer. J Clin Oncol 19(21):4117–4125
Sarna L (1998) Effectiveness of structured nursing assessment of symptom distress in advanced lung cancer. Oncol Nurs Forum 25(6):1041–1048
Taenzer P, Bultz BD, Carlson LE, Speca M, DeGagne T, Olson K, Doll R, Rosberger Z (2000) Impact of computerized quality of life screening on physician behaviour and patient satisfaction in lung cancer outpatients. Psychooncology 9(3):203–213. doi:10.1002/1099-1611(200005/06)9:3<203::AID-PON453>3.0.CO;2-Y
Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM, Selby PJ (2004) Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol 22(4):714–724. doi:10.1200/JCO.2004.06.078
Rosenbloom SK, Victorson DE, Hahn EA, Peterman AH, Cella D (2007) Assessment is not enough: a randomized controlled trial of the effects of HRQL assessment on quality of life and satisfaction in oncology clinical practice. Psychooncology 16(12):1069–1079. doi:10.1002/pon.1184
Kirkova J, Davis MP, Walsh D, Tiernan E, O’Leary N, LeGrand SB, Lagman RL, Russell KM (2006) Cancer symptom assessment instruments: a systematic review. J Clin Oncol 24(9):1459–1473. doi:10.1200/JCO.2005.02.8332
Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Lo SK, Wain G (2007) The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (Cancer Survivors’ Unmet Needs measure). Psychooncology 16(9):796–804. doi:10.1002/pon.1137
Hodgkinson K, Butow P, Hobbs KM, Hunt GE, Lo SK, Wain G (2007) Assessing unmet supportive care needs in partners of cancer survivors: the development and evaluation of the Cancer Survivors’ Partners Unmet Needs measure (CaSPUN). Psychooncology 16(9):805–813. doi:10.1002/pon.1138
Shelby RA, Lamdan RM, Siegel JE, Hrywna M, Taylor KL (2006) Standardized versus open-ended assessment of psychosocial and medical concerns among African American breast cancer patients. Psychooncology 15(5):382–397. doi:10.1002/pon.959
Wright EP, Kiely M, Johnston C, Smith AB, Cull A, Selby PJ (2005) Development and evaluation of an instrument to assess social difficulties in routine oncology practice. Qual Life Res 14(2):373–386
Wright P, Smith A, Roberts K, Selby P, Velikova G (2007) Screening for social difficulties in cancer patients: clinical utility of the Social Difficulties Inventory. Br J Cancer 97(8):1063–1070. doi:10.1038/sj.bjc.6604006
Veach TA, Nicholas DR, Barton MA (2002) Cancer and the family life cycle: a practitioner’s guide. Brunner–Routledge, New York
Hutchison SD, Steginga SK, Dunn J (2006) The tiered model of psychosocial intervention in cancer: a community based approach. Psychooncology 15(6):541–546. doi:10.1002/pon.973
Greenhalgh J, Long AF, Flynn R (2005) The use of patient reported outcome measures in routine clinical practice: lack of impact or lack of theory? Soc Sci Med 60(4):833–843. doi:10.1016/j.socscimed.2004.06.022
Howell D (2009) Literature review and environmental scan: psychosocial, supportive and palliative care standards and guidelines. Technical Document, Addendum 2009. The Cancer Journey Action Group, Canadian Partnership Against Cancer
Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, Whitty P, Eccles MP, Matowe L, Shirran L, Wensing M, Dijkstra R, Donaldson C (2004) Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 8 (6):iii-iv, 1-72. doi:94-08-29 [pii]
Fraser Health Hospice Palliative Care Program (2006) Depression in the terminally ill. http://www.fraserhealth.ca/Services/HomeandCommunityCare/HospicePalliativeCare/Pages/SymptomGuidelines.aspx. Accessed 22 July 2008
National Consensus Project for Quality Palliative Care (2004) Clinical Practice Guidelines for Quality Palliative Care. National Consensus Project for Quality Palliative Care, Pittsburgh
Qaseem A, Snow V, Shekelle P, Casey DE Jr, Cross JT Jr, Owens DK, Dallas P, Dolan NC, Forciea MA, Halasyamani L, Hopkins RH Jr (2008) Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: a clinical practice guideline from the American College of Physicians. Ann Intern Med 148(2):141–146
Registered Nurses’ Association of Ontario (2002) Crisis intervention. Registered Nurses’ Association of Ontario, Toronto
Rodin G, Katz M, Lloyd N, Green E, Mackay JA, Wong R and members of the Supportive Care Guidelines Group (2006) Evidence-based series #13-6: Section 1: the management of depression in cancer patients: a clinical practice guideline. http://www.cancercare.on.ca. Accessed 8 June 2008
Scottish Intercollegiate Guidelines Network (2005) Management of breast cancer in women: a national clinical guideline. Scottish Intercollegiate Guidelines Network, Edinburgh
Scottish Intercollegiate Guidelines Network (2008) Management of cervical cancer: a national clinical guideline. Scottish Intercollegiate Guidelines Network, Edinburgh
Acknowledgments
We acknowledge Health Canada and the BC Cancer Foundation for supporting an initial review of psychosocial guidelines; Mary Johnson, Carol Digout, and Patricia Oakley for their technical expertise and contributions to this project; Margaret B. Harrison, RN, PhD, and Joan van den Hoek for their consultation regarding the ADAPTE process; Fay Bennie for administrative support; and the expert clinicians and other stakeholders who provided valuable feedback prior to the finalization of the guideline.
Research Support
Production of this guideline has been made possible through a financial contribution from Health Canada, through the Canadian Partnership Against Cancer.
Authors’ disclosures of potential conflicts of interest
All authors and expert panel members completed a disclosure declaration regarding any conflicts of interest and none indicated a financial interest or conflict of interest due to any other reason.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer
The views expressed herein represent the views of the National Guideline Expert Panel, a sub-group of the Standards, Guidelines and Indicators Working Group of The Cancer Journey Action Group, Canadian Partnership Against Cancer. Care has been taken in the preparation of the information contained in this document. Nonetheless, any person seeking to apply or consult the practice guideline is expected to use independent clinical judgment in the context of individual clinical circumstances or seek out the supervision of a qualified clinician. The Canadian Association of Psychosocial Oncology makes no representation or warranties of any kind whatsoever regarding their content or use or application and disclaims any responsibility for their application or use in any way.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 39 kb)
Rights and permissions
About this article
Cite this article
Howell, D., Mayo, S., Currie, S. et al. Psychosocial health care needs assessment of adult cancer patients: a consensus-based guideline. Support Care Cancer 20, 3343–3354 (2012). https://doi.org/10.1007/s00520-012-1468-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1468-x