Abstract
Background
By virtue of the benefits associated with minimally invasive approaches, laparoscopic splenectomy (LS) is believed to have better patient-related outcomes compared to open splenectomy (OS). However, there are limited data directly comparing the two techniques.
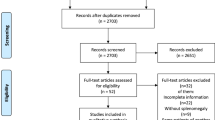
Methods
Patients who underwent elective LS and OS between 2005 and 2010 were identified from the public use file of the ACS-NSQIP database using the Current Procedural Terminology codes 38120 and 38100. Patients who had concomitant procedures were excluded. Because of the nonrandom assignment of surgical techniques, a selection bias could have been responsible for the differences in patient outcomes. Therefore, patient characteristics and comorbidities that were available and could have been potential confounders were compared and regression analysis was performed to determine independent risk factors associated with serious and overall morbidity as well as mortality.
Results
During the study period 1,644 and 851 patients underwent LS and OS, respectively. Compared to patients who underwent LS, patients who had OS had a longer median length of hospital stay (3 vs. 6 days, P < 0.0001) and higher incidences of serious (7 vs. 17 %, P < 0.0001) and overall morbidity (12 vs. 25 %, P < 0.0001) and mortality (1.4 vs. 3.3 %, P = 0.02). However, there were certain significant differences in the characteristics and comorbidities of the patients that could have confounded outcomes. On regression analysis, OS was not associated with higher mortality (OR = 1.43, 95 % CI 0.7–2.7, P = 0.28) but was associated with higher serious morbidity (OR = 1.8, 95 % CI 1.4–2.3, P = 0.001) and overall morbidity (OR = 2.0, 95 % CI 1.6–2.4, P = 0.0001).
Conclusion
After adjusting for available confounders, patients who underwent LS had lower morbidity and similar mortality rates. Although certain confounders such as previous surgical history, underlying pathology, and spleen size could still have potentially influenced outcomes, the data suggest that patient outcomes after LS are excellent and when technically possible a minimally invasive technique should be the preferred approach for splenectomy.
Similar content being viewed by others
References
Feldman LS (2011) Laparoscopic splenectomy: standardized approach. World J Surg 35:1487–1495
Glasgow RE, Yee LF, Mulvihill SJ (1997) Laparoscopic splenectomy. The emerging standard. Surg Endosc 11:108–112
Park A, Marcaccio M, Sternbach M, Witzke D, Fitzgerald P (1999) Laparoscopic vs. open splenectomy. Arch Surg 134:1263–1269
Katkhouda N, Hurwitz MB, Rivera RT, Chandra M, Waldrep DJ, Gugenheim J, Mouiel J (1998) Laparoscopic splenectomy: outcome and efficacy in 103 consecutive patients. Ann Surg 228:568–578
Friedman RL, Fallas MJ, Carroll BJ, Hiatt JR, Phillips EH (1996) Laparoscopic splenectomy for ITP. The gold standard. Surg Endosc 10:991–995
Vecchio R, Cacciola E, Lipari G, Privitera V, Polino C, Cacciola R (2005) Laparoscopic splenectomy reduces the need for platelet transfusion in patients with idiopathic thrombocytopenic purpura. J Soc Laparoendosc Surg 9:415–418
Tanoue K, Okita K, Akahoshi T, Konishi K, Gotoh N, Tsutsumi N, Tomikawa M, Hashizume M (2002) Laparoscopic splenectomy for hematologic diseases. Surgery 131:660–667
Park AE, Birgisson G, Mastrangelo MJ, Marcaccio MJ, Witzke DB (2000) Laparoscopic splenectomy for hematologic diseases. Surgery 131:S318–S323
Winslow ER, Brunt LM (2003) Perioperative outcomes of laparoscopic versus open splenectomy: a metaanalysis with an emphasis of complications. Surgery 134:647–653 discussion 654-655
Berends FJ, Schep N, Cuesta MA, Bonjer HJ, Kappers-Klunne MC, Huijgens P, Kazemier G (2004) Hematological long-term results of laparoscopic splenectomy for patients with idiopathic thrombocytopenic purpura: a case control study. Surg Endosc 18:766–770
Kucuk C, Souzuer E, Ok E, Altuntas F, Yilmaz Z (2005) Laparoscopic versus open splenectomy in the management of benign and malignant hematologic diseases. A ten-year single center experience. J Laparoendosc Adv Surg Tech 15:135–139
Patel AG, Parker JE, Wallwork B, Kau KB, Donaldson N, Rhodes MR, O’Rourke N, Nathanson L, Fielding G (2003) Massive splenomegaly is associated with significant morbidity after laparoscopic splenectomy. Ann Surg 238:235–240
Smith L, Luna G, Merg AR, McNevin MS, Moore MR, Bax TW (2004) Laparoscopic splenectomy for treatment of splenomegaly. Am J Surg 187:618–620
Koshenkov VP, Nemeth ZH, Carter MS (2012) Laparoscopic splenectomy: outcome and efficacy for massive and supramassive spleens. Am J Surg 203:517–522
Grahn SW, Alveraz J 3rd, Kirkwood K (2006) Trends in laparoscopic splenectomy for massive splenomegaly. Arch Surg 141:755–761 discussion 761-762
Habermalz B, Sauerland S, Decker G, Deltaire B, Gigot JF, Leandros E, Lechner K, Rhodes M, Silecchia G, Szold A, Targarona E, Torelli P, Neugebuer E (2008) Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc 22:821–848
Crawford RS, Cambria RP, Abularrage CJ, Conrad MF, Lancaster RT, Watkins MT, LaMuraglia GM (2010) Preoperative functional status predict perioperative outcomes after infrainguinal bypass surgery. J Vasc Surg 51:351–358 discussion 358-359
Causey MW, Maykel JA, Hatch Q, Miller S, Steele SR (2011) Identifying risk factors for renal failure and myocardial infarction following colorectal surgery. J Surg Res 170:32–37
Hollenbeck BK, Miller DC, Taub D, Dunn RL, Khuri SF, Henderson WG, Montie JE, Underwood W 3rd, Wei JT (2005) Identifying risk factors for potentially avoidable complications following radical cystectomy. J Urol 174:1231–1237 discussion 1237
Belmont PJ Jr, Davey S, Orr JD, Ochoa LM, Bader JO, Schoenfeld AJ (2011) Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the National Surgical Quality Improvement Program. J Am Coll Surg 213:370–378
Disclosures
S. Ahad, C. Gonczy, V. Advani, S. Markwell, and I. Hassan have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahad, S., Gonczy, C., Advani, V. et al. True benefit or selection bias: an analysis of laparoscopic versus open splenectomy from the ACS-NSQIP. Surg Endosc 27, 1865–1871 (2013). https://doi.org/10.1007/s00464-012-2727-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2727-0