Abstract
Background
Dementia patients often present with coexisting medical conditions and potentially face higher risk of complications during hospitalization. Because the general features of postoperative adverse outcomes among surgical patients with dementia are unknown, we conducted a nationwide, retrospective cohort study to characterize surgical complications among dementia patients compared with sex- and age-matched nondementia controls.
Methods
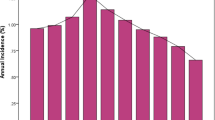
Reimbursement claims from the Taiwan National Health Insurance Research Database were studied. A total of 18,923 surgical patients were enrolled with preoperative diagnosis of dementia for 207,693 persons aged 60 years or older who received inpatient major surgeries between 2004 and 2007. Their preoperative comorbidities were adjusted and risks for major surgical complications were analyzed.
Results
Dementia patients who underwent surgery had a significantly higher overall postoperative complication rate, adjusted odds ratio (OR) 1.79 (95 % confidence interval [CI] 1.72–1.86), with higher medical resources use, and in-hospital expenditures. Compared with controls, dementia patients had a higher incidence of certain postoperative complications that are less likely to be identified in their initial stage, such as: acute renal failure, OR = 1.32 (1.19–1.47); pneumonia, OR = 2.18 (2.06–2.31); septicemia, OR = 1.8 (1.69–1.92); stroke, OR = 1.51 (1.43–1.6); and urinary tract infection, OR = 1.62 (1.5–1.74).
Conclusions
These findings have specific implications for postoperative care of dementia patients regarding complications that are difficult to diagnose in their initial stages. Acute renal failure, pneumonia, septicemia, stroke, and urinary tract infection are the top priorities for prevention, early recognition, and intervention of postoperative complications among surgical patients with dementia. Further efforts are needed to determine specific protocols for health care teams serving this population.
Similar content being viewed by others
References
Ritchie K, Lovestone S (2002) The dementias. Lancet 360:1759–1766
Morris JC, Heyman A, Mohs RC et al (1989) The consortium to establish a registry for Alzheimer’s disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 39:1159–1165
Schwam E, Xu Y (2010) Cognition and function in Alzheimer’s disease: identifying the transitions from moderate to severe disease. Dement Geriatr Cogn Disord 29:309–316
Chung JA, Cummings JL (2000) Neurobehavioral and neuropsychiatric symptoms in Alzheimer’s disease: characteristics and treatment. Neurol Clin 18:829–846
Etters L, Goodall D, Harrison BE (2008) Caregiver burden among dementia patient caregivers: a review of the literature. J Am Acad Nurse Pract 20:423–428
Jönsson L, Wimo A (2009) The cost of dementia in Europe: a review of the evidence, and methodological considerations. Pharmacoeconomics 27:391–403
Rothschild JM, Bates DW, Leape LL (2000) Preventable medical injuries in older patients. Arch Intern Med 160:2717–2728
Sansur CA, Reames DL, Smith JS et al (2010) Morbidity and mortality in the surgical treatment of 10,242 adults with spondylolisthesis. J Neurosurg Spine 13:589–593
Guijarro R, San Román CM, Gómez-Huelgas R et al (2010) Impact of dementia on hospitalization. Neuroepidemiology 35:101–108
Rowland KJ, Kodner IJ, Cashen M et al (2009) Surgical futility: “aggressive” surgery on the severely demented. Surgery 145:351–354
Cheng CL, Kao YH, Lin SJ et al (2011) Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf 20:236–242
Khuri SF, Henderson WG, DePalma RG et al (2005) Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 242:326–341
Lyketsos CG, Sheppard JM, Rabins PV (2000) Dementia in elderly persons in a general hospital. Am J Psychiatry 157:704–707
Wolfe M, Almond A, Robertson S et al (2010) Chronic kidney disease presenting acutely: presentation, clinical features and outcome of patients with irreversible chronic kidney disease who require dialysis immediately. Postgrad Med J 86:405–408
Chong CP, Street PR (2008) Pneumonia in the elderly: a review of the epidemiology, pathogenesis, microbiology, and clinical features. South Med J 101:1141–1145
Yaffe K, Kanaya A, Lindquist K et al (2004) The metabolic syndrome, inflammation, and risk of cognitive decline. J Am Med Assoc 292:2237–2242
Mitchell SL, Teno JM, Kiely DK et al (2009) The clinical course of advanced dementia. N Engl J Med 361:1529–1538
Sue Eisenstadt E (2010) Dysphagia and aspiration pneumonia in older adults. J Am Acad Nurse Pract 22:17–22
Horner J, Alberts MJ, Dawson DV et al (1994) Swallowing in Alzheimer’s disease. Alzheimer Dis Assoc Disord 8:177–189
Jones DR, Lee HT (2008) Perioperative renal protection. Best Pract Res Clin Anaesthesiol 22:193–208
Brienza N, Giglio MT, Marucci M (2010) Preventing acute kidney injury after noncardiac surgery. Curr Opin Crit Care 16:353–358
Rock P, Rich PB (2003) Postoperative pulmonary complications. Curr Opin Anaesthesiol 16:123–131
Lo IL, Siu CW, Tse HF et al (2010) Preoperative pulmonary assessment for patients with hip fracture. Osteoporos Int 21:S579–S586
Ferreyra G, Long Y, Ranieri VM (2009) Respiratory complications after major surgery. Curr Opin Crit Care 15:342–348
Pendlebury ST, Rothwell PM (2009) Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol 8:1006–1018
Ehlenbach WJ, Hough CL, Crane PK et al (2010) Association between acute care and critical illness hospitalization and cognitive function in older adults. J Am Med Assoc 303:763–770
Morrison RS, Siu AL (2000) Survival in end-stage dementia following acute illness. J Am Med Assoc 284:47–52
Wolff JL, Starfield B, Anderson G (2002) Prevalence, expenditures and complications of multiple chronic conditions in the elderly. Arch Intern Med 162:2269–2276
World Alzheimer Report 2009. http://www.alz.co.uk/research/files/WorldAlzheimerReport.pdf
Bagger JP, Zindrou D, Taylor KM (2004) Postoperative infection with meticillin-resistant Staphylococcus aureus and socioeconomic background. Lancet 363:706–708
Agabiti N, Cesaroni G, Picciotto S et al (2008) The association of socioeconomic disadvantage with postoperative complications after major elective cardiovascular surgery. J Epidemiol Community Health 62:882–889
Acknowledgments
This research was supported by a Foundation for Anesthesia Education and Research fellowship grant, Taipei Medical University Hospital, without conflict of interest to be disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hu, CJ., Liao, CC., Chang, CC. et al. Postoperative Adverse Outcomes in Surgical Patients with Dementia: A Retrospective Cohort Study. World J Surg 36, 2051–2058 (2012). https://doi.org/10.1007/s00268-012-1609-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1609-x