Abstract
Purpose
We examined the prevalence, correlates, comorbidities, and suicidal tendencies of premenstrual dysphoric disorder (PMDD) according to the DSM-IV criteria in a nationwide sample of Korean women.
Methods
A total of 2,499 women aged 18–64 years participated in this study. Diagnostic assessments were based on the Korean version of the Composite International Diagnostic Interview (CIDI) 2.1 and its 12-month PMDD diagnostic module, which were administered by lay interviewers. The frequencies of DSM-IV psychiatric disorders, insomnia, and suicidal tendency were analyzed among PMDD cases and compared with non-PMDD cases, and both odds ratios and significance levels were calculated.
Results
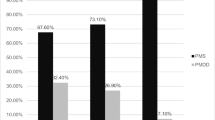
The 12-month prevalence rate of DSM-IV-diagnosed PMDD was 2.4 %. Among subjects with PMDD, 59.3 % had at least one psychiatric illness; in comparison, the control frequency was 21.8 %. Associations between PMDD and alcohol abuse/dependence, major depressive disorder, post-traumatic stress disorder, social phobia, specific phobia, somatoform disorder, insomnia, and suicidality were overwhelmingly positive and significant (p < 0.05), after controlling for age. Physical illness and being underweight were associated with increased risks of PMDD (p < 0.05).
Conclusions
PMDD was prevalent in the nationwide sample of Korean women and was frequently associated with other psychiatric disorders, insomnia, and suicidality, suggesting the need to detect and treat women who experience PMDD.
Similar content being viewed by others
References
American Psychiatric Association (1997) Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychiatric Association, Washington, DC
American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychiatric Association, Washington, DC
American Psychiatric Association (2011) DSM-V proposed revision. American Psychiatric Association, Washington, DC
Angst J, Sellaro R, Merikangas KR, Endicott J (2001) The epidemiology of perimenstrual psychological symptoms. Acta Psychiatr Scand 104:110–116
Baca-Garcia E, Diaz-Sastre C, Ceverino A, Garcia Resa E, Oquendo MA, Saiz-Ruiz J, de Leon J (2004) Premenstrual symptoms and luteal suicide attempts. Eur Arch Psychiatr Clin Neurosci 254:326–329
Baker FC, Kahan TL, Trinder J, Colrain IM (2007) Sleep quality and the sleep electroencephalogram in women with severe premenstrual syndrome. Sleep 30:1283–1291
Barnhart KT, Freeman EW, Sondheimer SJ (1995) A clinician’s guide to the premenstrual syndrome. Med Clin N Am 79:1457–1472
Basoglu C, Cetin M, Semiz UB, Agargun MY, Ebrinc S (2000) Premenstrual exacerbation and suicidal behavior in patients with panic disorder. Compr Psychiatr 41:103–105
Bertone-Johnson ER, Hankinson SE, Johnson SR, Manson JE (2009) Timing of alcohol use and the incidence of premenstrual syndrome and probable premenstrual dysphoric disorder. J Womens Health (Larchmt) 18:1945–1953
Chaturvedi SK, Chandra PS, Gururaj G, Pandian RD, Beena MB (1995) Suicidal ideas during premenstrual phase. J Affect Disord 34:193–199
Cho MJ, Chang SM, Lee YM, Bae A, Ahn JH, Son J, Hong JP, Bae JN, Lee DW, Cho SJ, Park JI, Lee JY, Kim JY, Jeon HJ, Sohn JH, Kim BS (2010) Prevalence of DSM-IV major mental disorders among Korean adults: a 2006 National Epidemiologic Survey (KECA-R). Asian J Psychiatr 3:26–30
Cho MJ, Hahm BJ, Suh DW, Hong JP, Bae JN, Kim JK, Lee DW, Cho SJ (2002) Development of a Korean version of the Composite International Diagnostic Interview (K-CIDI). J Korean Neuropsychiatr Assoc 41:123–137
Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, Bae JN, Lee DW, Park JI, Cho SJ, Lee CK, Hahm BJ (2007) Lifetime and 12 month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis 195:203–210
Choi D, Lee DY, Lehert P, Lee IS, Kim SH, Dennerstein L (2010) The impact of premenstrual symptoms on activities of daily life in Korean women. J Psychosom Obstet Gynaecol 31:10–15
Cohen LS, Soares CN, Otto MW, Sweeney BH, Liberman RF, Harlow BL (2002) Prevalence and predictors of premenstrual dysphoric disorder (PMDD) in older premenopausal women. The Harvard Study of Moods and Cycles. J Affect Disord 70:125–132
Dennerstein L, Lehert P, Keung LS, Pal SA, Choi D (2010) A population-based survey of Asian women’s experience of premenstrual symptoms. Menopause Int 16:139–145
Deuster PA, Adera T, South-Paul J (1999) Biological, social, and behavioral factors associated with premenstrual syndrome. Arch Fam Med 8:122–128
Duenas JL, Lete I, Bermejo R, Arbat A, Perez-Campos E, Martinez-Salmean J, Serrano I, Doval JL, Coll C (2011) Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in a representative cohort of Spanish women of fertile age. Eur J Obstet Gynecol Reprod Biol 156(1):72–77
Frank RT (1931) The hormonal cause of premenstrual tension. Arch Neurol Psychiatr 26:61–66
Gehlert S, Song IH, Chang CH, Hartlage SA (2009) The prevalence of premenstrual dysphoric disorder in a randomly selected group of urban and rural women. Psychol Med 39:129–136
Kessler RC, Ustun TB (2004) The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 13:93–121
Korea National Statistical Office (2006) National Statistics Report. Korea National Statistical Office
Li ZB, Ho SY, Chan WM, Ho KS, Li MP, Leung GM, Lam TH (2004) Obesity and depressive symptoms in Chinese elderly. Int J Geriatr Psychiatr 19:68–74
Mauri M, Reid RL, MacLean AW (1988) Sleep in the premenstrual phase: a self-report study of PMS patients and normal controls. Acta Psychiatr Scand 78:82–86
Mortola JF, Girton L, Beck L, Yen SS (1990) Diagnosis of premenstrual syndrome by a simple, prospective, and reliable instrument: the calendar of premenstrual experiences. Obstet Gynecol 76:302–307
Park S, Cho MJ, Chang SM, Bae JN, Jeon HJ, Cho SJ, Kim BS, Chung IW, Ahn JH, Lee HW, Hong JP (2010) Relationships of sleep duration with sociodemographic and health-related factors, psychiatric disorders and sleep disturbances in a community sample of Korean adults. J Sleep Res 19:567–577
Park S, Cho MJ, Chang SM, Jeon HJ, Cho SJ, Kim BS, Bae JN, Wang HR, Ahn JH, Hong JP (2011) Prevalence, correlates, and comorbidities of adult ADHD symptoms in Korea: Results of the Korean epidemiologic catchment area study. Psychiatry Res 186(2–3):378–383
Park S, Cho MJ, Jeon HJ, Lee HW, Bae JN, Park JI, Sohn JH, Lee YR, Lee JY, Hong JP (2010) Prevalence, clinical correlations, comorbidities, and suicidal tendencies in pathological Korean gamblers: results from the Korean Epidemiologic Catchment Area Study. Soc Psychiatr Psychiatr Epidemiol 45:621–629
Perkonigg A, Yonkers KA, Pfister H, Lieb R, Wittchen HU (2004) Risk factors for premenstrual dysphoric disorder in a community sample of young women: the role of traumatic events and posttraumatic stress disorder. J Clin Psychiatr 65:1314–1322
Potter J, Bouyer J, Trussell J, Moreau C (2009) Premenstrual syndrome prevalence and fluctuation over time: results from a French population-based survey. J Womens Health (Larchmt) 18:31–39
Scott KM, McGee MA, Wells JE, Oakley Browne MA (2008) Obesity and mental disorders in the adult general population. J Psychosom Res 64:97–105
Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC (2006) Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatr 63:824–830
Skrzypulec-Plinta V, Drosdzol A, Nowosielski K, Plinta R (2010) The complexity of premenstrual dysphoric disorder: risk factors in the population of Polish women. Reprod Biol Endocrinol 8:141
Stout AL, Steege JF, Blazer DG, George LK (1986) Comparison of lifetime psychiatric diagnoses in premenstrual syndrome clinic and community samples. J Nerv Ment Dis 174:517–522
Strine TW, Chapman DP, Ahluwalia IB (2005) Menstrual-related problems and psychological distress among women in the United States. J Womens Health (Larchmt) 14:316–323
Sunwoo YK, Bae JN, Hahm BJ, Lee DW, Park JI, Cho SJ, Lee JY, Kim JY, Chang SM, Jeon HJ, Cho MJ (2011) Relationships of mental disorders and weight status in the Korean adult population. J Korean Med Sci 26:108–115
Takeda T, Tasaka K, Sakata M, Murata Y (2006) Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in Japanese women. Arch Womens Ment Health 9:209–212
Tschudin S, Bertea PC, Zemp E (2010) Prevalence and predictors of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample. Arch Womens Ment Health 13:485–494
Widholm O, Kantero RL (1971) A statistical analysis of the menstrual patterns of 8,000 Finnish girls and their mothers. Acta Obstet Gynecol Scand Suppl 14(Suppl 14):11–36
Wittchen HU, Becker E, Lieb R, Krause P (2002) Prevalence, incidence and stability of premenstrual dysphoric disorder in the community. Psychol Med 32:119–132
Woods NF, Most A, Dery GK (1982) Prevalence of perimenstrual symptoms. Am J Public Health 72:1257–1264
World Health Organization (1997a) CIDI, core version 2.1 Interviewer’s manual. World Health Organization, Geneva
World Health Organization (1997b) CIDI, Core version 2.1 Trainer’s manual. World Health Organization, Geneva
World Health Organization Western Pacific Region (2000) International Association for the Study of Obesity, and International Obesity Task Force. The Asian-Pacific perspective: redefining obesity and its treatment. WHO Western Pacific Region, Geneva, Switzerland
World Health Organization. (1990) Composite International Diagnostic Interview (CIDI), Version 1.0. World Health Organization, Geneva
World Health Organization. (1997) Procedures for the Development of New Language Versions of the WHO Composite International Diagnostic Interview (WHO-CIDI). World Health Organization, Geneva
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hong, J.P., Park, S., Wang, HR. et al. Prevalence, correlates, comorbidities, and suicidal tendencies of premenstrual dysphoric disorder in a nationwide sample of Korean women. Soc Psychiatry Psychiatr Epidemiol 47, 1937–1945 (2012). https://doi.org/10.1007/s00127-012-0509-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-012-0509-6