Abstract
Background
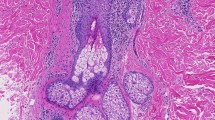
Folliculitis decalvans (FD) is a form of primary neutrophilic scarring alopecia that is characterized clinically by chronic suppurative folliculitis and often associated with pruritus or even pain. Treatment of FD is often difficult. Herein, we report a case of recalcitrant and painful folliculitis decalvans refractory to antibiotic and anti-inflammatory therapies, which was successfully treated by intensity-modulated radiotherapy (IMRT) in order to irreversibly eliminate hair follicles that prove to be one etiological trigger.
Case presentation
A 45-year-old male patient with a refractory FD presented with a crusting suppurative folliculitis and atrophic scarring patches on the scalp associated with pain and pruritus. We attempted relief of symptoms by reducing scalp inflammation and eliminating hair follicles through radiation. We delivered 11.0 Gy in two radiation series using tomotherapy, 5.0 Gy in 5 equivalent fractions as a first radiation course. The symptoms markedly decreased but did not totally disappear. Therefore, we delivered a second radiation series 4 months later with an additional 6 Gy. This led to almost complete epilation on the scalp and abolished pain and pruritus on the capillitium. The patient was regularly followed up until 26 months after radiotherapy. Draining lesions or exudation did not recur. He only experienced discrete hair regrowth in the occipital region with folliculitis 12 months after radiotherapy. These residual lesions are currently treated with laser epilation therapy.
Conclusion
A radical approach to eliminating hair follicles by repeated radiation therapy may induce lasting relief of symptoms in chronic suppurative FD associated with persistent trichodynia.
Zusammenfassung
Hintergrund
Die Folliculitis decalvans (FD) ist eine Form der primär neutrophilen Alopezie, welche klinisch durch Schmerzen und eitrige Follikel gekennzeichnet ist. Da es bisher kein einheitliches Behandlungskonzept gibt, wird hier über eine FD berichtet, welche trotz mehrfacher antibiotischer- und antiinflammatorischer Therapie rezidivierte. Die Behandlung erfolgte mit intensitätsmodulierter Radiotherapie (IMRT), um eine dauerhafte Schädigung der Haarfollikel zu erzielen.
Fallbericht
Beschrieben wird der Fall eines 45-jährigen Patienten, der sich mit rezidivierender, chronisch-eitriger Alopezie sowie Schmerzen und Pruritus vorstellte. Die Autoren entschieden sich, eine Radiotherapie (RT) durchzuführen, welche eine Verringerung der Entzündung im Bereich der Kopfhaut sowie eine dauerhafte Schädigung der Haarfollikel erzielen sollte, um somit die Symptome der FD zu lindern. Es wurden 11,0 Gy in 2 Bestrahlungsserien unter Einsatz der Tomotherapie durchgeführt. Bei der ersten Serie wurde eine Gesamtreferenzdosis (GRD) von 5 Gy in 5 gleichwertigen Fraktionen appliziert. Aufgrund weiterhin bestehender Beschwerden, erfolgte 4 Monate später erneut die Applikation einer RT-Serie mit einer GRD von 6 Gy. Damit wurden eine komplette Epilation und Beschwerdefreiheit erreicht. Der Patient nimmt regelmäßig Nachsorgekontrollen wahr und befindet sich aktuell in einem Follow-up von 26 Monaten. Im weiteren Verlauf traten keine neuen Exsudate auf. Lediglich in der Okzipitalregion kam es zu einem diskreten Haarwuchs, welcher mit einer leichten Follikulitis einherging. Aktuell wird eine Haarentfernung mittels Laser durchgeführt.
Schlussfolgerung
Bei einer chronisch-eitrigen FD mit anhaltender Trichodynie können wiederholte RT-Serien zu einer dauerhaften Entfernung der Haarfollikel mit langfristiger Besserung der Symptome eingesetzt werden.




Similar content being viewed by others
References
Bernárdez C, Molina-Ruiz AM, Requena L (2015) Histopatología de las alopecias. Parte II. Alopecias cicatriciales. Actas Dermo-Sifiliográficas 106:260–270. doi:10.1016/j.ad.2014.06.016
Olsen EA, Bergfeld WF, Cotsarelis G et al (2003) Summary of North American Hair Research Society (NAHRS)-sponsored workshop on cicatricial Alopecia, Duke University Medical Center, February 10 and 11, 2001. J Am Acad Dermatol 48:103–110. doi:10.1067/mjd.2003.68
Otberg N, Kang H, Alzolibani AA et al (2008) Folliculitis decalvans. Dermatol Ther 21:238–244. doi:10.1111/j.1529-8019.2008.00204.x
Chiarini C, Torchia D, Bianchi B et al (2008) Immunopathogenesis of folliculitis Decalvans. Clues in early lesions. Am J Clin Pathol 130:526–534. doi:10.1309/NG60Y7V0WNUFH4LA
Bogg A (1963) Folliculitis decalvans. Acta Dermatovenereol 43:14-24
Sillani C, Bin Z, Ying Z et al (2010) Effective treatment of folliculitis decalvans using selected antimicrobial agents. Int J Trichology 2:20–23. doi:10.4103/0974-7753.66908
Vañó-Galván S, Molina-Ruiz AM, Fernández-Crehuet P et al (2015) Folliculitis decalvans. A multicentre review of 82 patients. J Eur Acad Dermatol Venereol 29:1750–1757. doi:10.1111/jdv.12993
Sunderkötter C, Brehler R, Becker K (2014) Systemtherapie mit Antiinfektiva. Hautarzt 65:106–112. doi:10.1007/s00105-013-2653-7
Sunderkötter C, Becker K (2015) Frequent bacterial skin and soft tissue infections. Diagnostic signs and treatment. J Dtsch Dermatol Ges 13:501–526. doi:10.1111/ddg.12721
Rödel F, Keilholz L, Herrmann M et al (2007) Radiobiological mechanisms in inflammatory diseases of low-dose radiation therapy. Int J Radiat Biol 83:357–366. doi:10.1080/09553000701317358
Manda K, Glasow A, Paape D et al (2012) Effects of ionizing radiation on the immune system with special emphasis on the interaction of dendritic and T cells. Front Oncol 2:102. doi:10.3389/fonc.2012.00102
Arenas M, Sabater S, Hernández V et al (2012) Anti-inflammatory effects of low-dose radiotherapy. Strahlenther Onkol 188(11):975–981. doi:10.1007/s00066-012-0170-8
Hawker GA, Mian S, Kendzerska T et al (2011) Measures of Adult Pain Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res 63:S240–S252. doi:10.1002/acr.20543
Balter S, Hopewell JW, Miller DL et al (2010) Fluoroscopically guided interventional procedures. A review of radiation effects on patients’ skin and hair. Radiology 254:326–341. doi:10.1148/radiol.2542082312
Schiel RO, Herzog W, Hof H et al (2013) Effekte systematischer Informationen über psychosoziale Angebote während der ambulanten Strahlentherapie. Strahlenther Onkol 189:579–585. doi:10.1007/s00066-013-0366-6
Kirchheiner K, Czajka A, Ponocny-Seliger E et al (2013) Physical and psychosocial support requirements of 1,500 patients starting radiotherapy. Strahlenther Onkol 189:424–429. doi:10.1007/s00066-013-0329-y
Seegenschmiedt MH, Micke O, Niewald M et al (2015) DEGRO guidelines for the radiotherapy of non-malignant disorders. Strahlenther Onkol 191:541–548. doi:10.1007/s00066-015-0818-2
Seegenschmiedt MH, Micke O, Willich N (2004) Radiation therapy for Nonmalignant diseases in Germany. Strahlenther Onkol 180:718–730. doi:10.1007/s00066-004-9197-9
McMULLAN FH (1956) Perifolliculitis capitis abscedens et suffodiens. AMA Arch Derm 73:256. doi:10.1001/archderm.1956.01550030058005
Elsayad K, Kriz J, Bauch J et al (2015) Radiation therapy as part of the therapeutic regimen for extensive multilocular myxedema in a patient with exophthalmos, myxedema and osteoarthropathy syndrome. A case report. Oncol Lett 9:2404–2408. doi:10.3892/ol.2015.2990
Smith EP, Hardaway CA, Graham BS et al (2006) Folliculitis decalvans treated with radiation therapy. Cutis 78:162–164
Guskova AK (2001) Medical Characteristics of different types of radiation accidents. In: Mettler FA, Gusev IA, Guskova AK (eds) In medical management of radiation accidents, 2nd edn. CRC Press, Boca Raton, pp 15–22 (Print ISBN: 978-0-8493-7004-5, eBook ISBN: 978-1-4200-3719-7, DOI:10.1201/9781420037197.ch2)
Trott K, Kamprad F (2006) Estimation of cancer risks from radiotherapy of Benign diseases. Strahlenther Onkol 182:431–436. doi:10.1007/s00066-006-1542-8
RON E, MODAN B, PRESTON D et al (1991) Radiation-induced skin carcinomas of the head and neck. Rad Res 125:318–325
Shore RE, Moseson M, Xue X et al (2002) Skin cancer after X-ray treatment for scalp ringworm. Radiat Res 157:410–418
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Elsayad, J. Kriz, U. Haverkamp, K-M. Plachouri, A. Jeskowiak, C. Sunderkötter, and H.T. Eich state that there are no conflicts of interest.
Consent was obtained from all patients identifiable from images or other information within the manuscript. In the case of underage patients, consent was obtained from a parent or legal guardian. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Additional information
This case was presented at the Annual Meeting of the German Society for Radiation Oncology, July 3–6, 2014, Düsseldorf, Germany.
Rights and permissions
About this article
Cite this article
Elsayad, K., Kriz, J., Haverkamp, U. et al. Treatment of folliculitis decalvans using intensity-modulated radiation via tomotherapy. Strahlenther Onkol 191, 883–888 (2015). https://doi.org/10.1007/s00066-015-0891-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-015-0891-6