Abstract
Total hip arthroplasty and total knee arthroplasty (THA and TKA) are surgeries to replace severely damaged hip and knee joints in the human body by artificial joints. THA and TKA can significantly alleviate the pain of the patient’s joints, improve function and the quality of life. As China is gradually becoming an aging society, according to the figures published by the National Bureau of Statistics of China, as of 2019, the data on the elderly population in our country is: the population over 60 years old account for 17.9% of the total population, and is growing rapidly at a rate of nine million per year; the population over 65 years old account for 12.6% of the total population. In 2022, it will become a deep aging society with the percentage of more than 14%, a super-aging society with the percentage of more than 20% in 2033, and then continue to rapidly increase to about 35% in 2060. Due to the large basic population, China has a huge number of the elderly population, and the number of elderly patients suffering from bone and joint diseases is increasing year by year, and the demand for THA and TKA is also gradually increasing. Kurtz et al. (J Bone Joint Surg Am 89(4):780–785, 2007) predicted in 2007 that the demand for hip and knee arthroplasty in the United States in 2020 would reach 380,000 and 1,520,000, and by 2030, it would reach 570,000 and 3,480,000. According to statistics from Professor Weng Xisheng of Peking Union Medical College Hospital, the number of hip and knee arthroplasty in China in 2019 was 577,000 and 375,000 respectively, an increase of 31% and 50% compared with 2018.
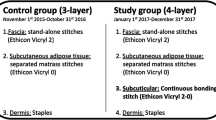
With the increase THA and TKA, surgical complications also receive increasing attention, one of which is incision complications. Common incision complications after THA and TKA include drainage, swelling, ecchymosis, blisters, dehiscence, superficial and deep infections, etc. The incidence reported in the literature ranges from 0.2%–21% (Saleh et al., J Orthop Res 20(3):506–515, 2002; Patel et al., J Bone Joint Surg Am 89(1):33–38, 2007; Adelani et al., Bone Joint J 96–B(5):619–621, 2014; Wagenaar et al., J Arthroplast 34(1):175–182, 2019). Once there is surgical incision complication, more dressing changes, debridement, and even repeated surgeries may be indicated, which will prolong the patient’s hospital stay and treatment time, delay early functional exercise, increase the incidence of periprosthetic joint infection (PJI) (Atkins et al., J Arthroplast 34(2S):S85–S92, 2019), lead to lower patient satisfaction, medical resource consumption, lower hospital operation efficiency, increased workload of doctors and increased risk of medical disputes. On the contrary, good incision healing can also shorten the patient’s hospital stay and reduce medical expenses. At the same time, a beautiful incision can also significantly increase the patient’s satisfaction with the surgical effect. Therefore, in artificial joint arthroplasty surgeries, we need to pay attention to the incision and suturing technique of the surgical incision and select the appropriate materials to close the incision to obtain the best incision healing and reduce complications.
This chapter will focus on the incision and closure in hip and knee arthroplasty surgeries, taking the commonly used posterolateral approach, lateral approach, anterior approach of the hip arthroplasty, and medial parapatellar approach of the knee arthroplasty as examples, and introduce the techniques of the surgical incision, soft tissue closure, and related precautions, as well as the prevention and treatment of complications.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg (Br). 1950;32:183–6.
Moore AT. The Moore self-locking vitallium prosthesis in fresh femoral neck fractures: a new low posterior approach (the southern exposure). AAOS Instr Course Lect. 1959;16:309.
Smith-Petersen MN. Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am. 1949;31A(1):40–6.
Lavernia C, Contreras Raygoza J, Alcerro J. The peel in total knee revision: exposure in the difficult knee. Clin Orthop Relat Res. 2011;469:146–53.
Weiss AP, Krackow KA. Persistent wound drainage after primary total knee arthroplasty. J Arthroplast. 1993;8(3):285–9.
Jaberi FM, et al. Procrastination of wound drainage and malnutrition affect the outcome of joint arthroplasty. Clin Orthop Relat Res. 2008;466(6):1368–71.
Al-Houraibi RK, et al. General assembly, prevention, wound management: proceedings of international consensus on orthopedic infections. J Arthroplast. 2019;34(2S):S157–68.
Hansen E, et al. Negative pressure wound therapy is associated with resolution of incisional drainage in most wounds after hip arthroplasty. Clin Orthop Relat Res. 2013;471(10):3230–6.
Galat DD, et al. Surgical treatment of early wound complications following primary total knee arthroplasty. J Bone Joint Surg Am. 2009;91(1):48–54.
Abdel Karim M, Andrawis J, Bengoa F, Bracho C, Compagnoni R, Cross M, et al. Hip and knee section, diagnosis, algorithm: proceedings of international consensus on orthopedic infections. J Arthroplasty. 2019;34(2S):S339–S50 (Proceedings of the International Consensus Meeting on Periprosthetic Joint Infection. Foreword. J Orthop Res. 2014;32 Suppl 1:S2–3).
Patel VP, et al. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(1):33–8.
Ares O, et al. General assembly, prevention, host related local: proceedings of international consensus on orthopedic infections. J Arthroplast. 2019;34(2S):S3–S12.
Shohat N, et al. Serum fructosamine: a simple and inexpensive test for assessing preoperative glycemic control. J Bone Joint Surg Am. 2017;99(22):1900–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chai, W. et al. (2021). Incision Suture Technique After Total Hip and Knee Arthroplasty. In: Tang, P., Wu, K., Fu, Z., Chen, H., Zhang, Y. (eds) Tutorials in Suturing Techniques for Orthopedics. Springer, Singapore. https://doi.org/10.1007/978-981-33-6330-4_10
Download citation
DOI: https://doi.org/10.1007/978-981-33-6330-4_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-33-6329-8
Online ISBN: 978-981-33-6330-4
eBook Packages: MedicineMedicine (R0)