Abstract
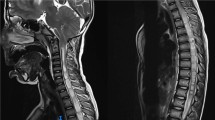
There are ample number of neurosurgical conditions that have associated genetic disorders. Neurosurgical conditions include craniosynostosis, craniopagus twins, and craniovertebral anomalies like atlantoaxial instability, meningomyelocele, and other neural tube defects. Some of the commonly associated genetic disorders are Down’s syndrome, Klippel-Feil syndrome, Goldenhar syndrome, Apert syndrome, and Muenke syndrome. Findings vary from airway changes to bony changes and from cardiac to renal anomalies. Depending upon the type and severity of the lesions, possible complications may vary from neurologic sequelae, respiratory complications, ventilatory and weaning issues, coagulation abnormalities, positioning problems to common problems like venous air embolism, temperature and acid-base changes, and fluid and electrolyte abnormalities to postoperative pain management. Dedicated neuroanesthesia care is the key to a successful perioperative management and positive outcome of these patients.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Singh GP. Neuroembryology. In: Prabhakar H, editor. Essentials of neuroanesthesia. Amsterdam: Elsevier Publications; 2017. pages 41-50.
Derderian C, Seaward J, editors. Syndromic craniosynostosis. Seminars in plastic surgery. New York, NY: Thieme Medical Publishers; 2012.
Kruszka P, Addissie YA, Yarnell CM, Hadley DW, Guillen Sacoto MJ, Platte P, et al. Muenke syndrome: an international multicenter natural history study. Am J Med Genet A. 2016;170:918–29.
Koca TT. Apert syndrome: a case report and review of the literature. North Clin Istanbul. 2016;3:135.
Kumar A, Goel N, Sinha C, Singh A. Anesthetic implications in a child with crouzon syndrome. Anesth Essays Res. 2017;11:246.
Vogels A, Fryns J-P. Pfeiffer syndrome. Orphanet J Rare Dis. 2006;1:19.
Kadakia S, Helman SN, Healy NJ, Saman M, Wood-Smith D. Carpenter syndrome: a review for the craniofacial surgeon. J Craniofac Surg. 2014;25:1653–7.
Sharma A, Patel N, Arora S, Ramachandran R. Child with Saethre-Chotzen syndrome: anesthetic management and literature review. Acta Anaesthesiol Belg. 2014;65:179–82.
Roudneshin F, Agah M. Management of anesthesia in Goldenhar syndrome: case-series study. 2009.
Goel L, Bennur SK, Jambhale S. Treacher-collins syndrome–a challenge for anaesthesiologists. Indian J Anaesth. 2009;53:496.
Cladis F, Kumar A, Grunwaldt L, Otteson T, Ford M, Losee JE. Pierre Robin Sequence: a perioperative review. Anesth Analg. 2014;119:400–12.
Gençay I, Vargel I, Büyükkoçak Ü, Yazc I, Apan A. Anesthetic risks associated with Antley-Bixler syndrome. J Craniofac Surg. 2013;24:e21–e3.
Upmeyer S, Bothwell M, Tobias JD. Perioperative care of a patient with Beare–Stevenson syndrome. Pediat Anesth. 2005;15:1131–6.
Cohen MM. Jackson‐Weiss syndrome. Am J Med Genet A. 2001;100:325–9.
Thomas K, Hughes C, Johnson D, Das S. Anesthesia for surgery related to craniosynostosis: a review. Part 1. Pediat Anesth. 2012;22:1033–41.
Macfarlane F. Paediatric anatomy and physiology and the basics of paediatric anaesthesia. Anaesthesia UK [diunduh 6 Oktober 2006]. Tersedia dari: http://www.frca.co.uk/article.aspx. 2006
Rath GP, Dash HH. Anaesthesia for neurosurgical procedures in paediatric patients. Indian J Anaesth. 2012;56:502.
Pearson A, Matava C. Anaesthetic management for craniosynostosis repair in children. BJA Educ. 2016;16:410–6.
Furay C, Howell T. Paediatric neuroanaesthesia. Contin Educ Anaesth Crit Care Pain. 2010;10:172–6.
Bagheri SC, Jo C. Clinical review of oral and maxillofacial surgery - e-book. St. Louis, MO: Mosby; 2013.
Shands JA, Bundens W. Congenital deformities of the spine; an analysis of the roentgenograms of 700 children. Bull Hosp Joint Dis. 1956;17:110–33.
Kaddoum RN, Ahmed Z, D’Augsutine AA, Zestos MM. Guidelines for elective pediatric fiberoptic intubation. J Vis Exp. 2011;(47):2364.
Walker RW, Ellwood J. The management of difficult intubation in children. Pediat Anesth. 2009;19:77–87.
Blum RH, McGowan FX. Chronic upper airway obstruction and cardiac dysfunction: anatomy, pathophysiology and anesthetic implications. Pediat Anesth. 2004;14:75–83.
Thornhill MH, Dayer M, Lockhart PB, Prendergast B. Antibiotic prophylaxis of infective endocarditis. Curr Infect Dis Rep. 2017;19:9.
Stone JL, Goodrich JT. The craniopagus malformation: classification and implications for surgical separation. Brain. 2006;129:1084–95.
Browd SR, Goodrich JT, Walker ML. Craniopagus twins. J Neurosurg Pediatr. 2008;1:1.
Walker M, Browd SR. Craniopagus twins: embryology, classification, surgical anatomy, and separation. Childs Nerv Syst. 2004;20:554–66.
Parameswari A, Vakamudi M, Raghupathy V, Siddhartha R. Anaesthetic management of total craniopagus twins for magnetic resonance imaging and cerebral angiography. Br J Anaesth. 2010;105:368–70.
Chalam KS. Anaesthetic management of conjoined twins’ separation surgery. Indian J Anaesth. 2009;53:294.
Staffenberg DA, Goodrich JT. Separation of craniopagus conjoined twins with a staged approach. J Craniofac Surg. 2012;23:S62–S8.
Greene ND, Copp AJ. Neural tube defects. Annual review of neuroscience, vol. 37; 2014. p. 221–42.
Salih MA, Murshid WR, Seidahmed MZ. Classification, clinical features, and genetics of neural tube defects. Saudi Med J. 2014;35:S5.
BELL JE, Gordon A, Maloney A. The association of hydrocephalus and arnold‐chiari malformation with spina bifida in the fetus. Neuropathol Appl Neurobiol. 1980;6:29–39.
Soundararajan N, Cunliffe M. Anaesthesia for spinal surgery in children. Br J Anaesth. 2007;99:86–94.
Brown RH, Hamilton RG, Mintz M, Jedlicka AE, Scott AL, Kleeberger SR. Genetic predisposition to latex allergyrole of interleukin 13 and interleukin 18. Anesthesiology. 2005;102:496–502.
McKay SD, Al-Omari A, Tomlinson LA, Dormans JP. Review of cervical spine anomalies in genetic syndromes. Spine. 2012;37:E269–E77.
Ali FE, Al-Bustan MA, Al-Busairi WA, Al-Mulla FA, Esbaita EY. Cervical spine abnormalities associated with Down syndrome. Int Orthop. 2006;30:284–9.
Hata T, Todd MM. Cervical spine considerations when anesthetizing patients with Down syndrome. Anesthesiology. 2005;102:680–5.
Hamidi M, Nabi S, Husein M, Mohamed ME, Tay KY, McKillop S. Cervical spine abnormalities in 22q11. 2 deletion syndrome. Cleft Palate Craniofac J. 2014;51:230–3.
Malik P, Choudhry DK. Larsen syndrome and its anaesthetic considerations. Pediat Anesth. 2002;12:632–6.
Bonafé L, Mittaz-Crettol L, Ballhausen D, Superti-Furga A. Diastrophic dysplasia. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews®. Seattle, WA: University of Washington; 2004. 1993-2018.
Dixit N, George B, Manjuladevi M, Varghese V, Kalaichelvam A. Morquio syndrome with acute cord compression: an anesthetic challenge. Karnataka Anaesth J. 2015;1:143–5.
Gupta AK, Kharde V, Gawer V, Sidhaye R, Divekar D. Hurler’s syndrome: anaesthetic challenges and management. Anest Pediat Neonat. 2010;8:1.
Shetty GM, Song HR, Unnikrishnan R, Suh SW, Lee S-H, Hur CY. Upper cervical spine instability in pseudoachondroplasia. J Pediatr Orthop. 2007;27:782–7.
Breik O, Mahindu A, Moore MH, Molloy CJ, Santoreneos S, David DJ. Central nervous system and cervical spine abnormalities in Apert syndrome. Childs Nerv Syst. 2016;32:833–8.
Healey D, Letts M, Jarvis JG. Cervical spine instability in children with Goldenhar’s syndrome. Can J Surg. 2002;45:341.
Gupta K, Subharti N, Subhartipuram N. Goldenhar syndrome: airway and anesthetic management-a case report. J Pioneeri Med Sci. 2011;1:56–9.
Liu J-X, Hu R, Sun Y, Jiang H. General anesthesia in fibrodysplasia ossificans progressive: a case report and clinical review. Int J Clin Exp Med. 2014;7:1474.
Hsieh M-H, Yeh K-T, Chen H, Yu T-C, Peng C-H, Liu K-L, et al. Cervical Klippel-Feil syndrome progressing to myelopathy following minor trauma. Tzu Chi Med J. 2014;26:47–50.
Araújo MR, Marques C, Freitas S, Santa-Bárbara R, Alves J, Xavier C. Marfan Syndrome: new diagnostic criteria, same anesthesia care? Case report and review. Brazilian J Anesth. 2016;66:408–13.
Wiesmann T, Castori M, Malfait F, Wulf H. Recommendations for anesthesia and perioperative management in patients with Ehlers-Danlos syndrome (s). Orphanet J Rare Dis. 2014;9:109.
Ain MC, Shirley ED. Spinal manifestations of the skeletal dysplasias. The growing spine. New York, NY: Springer; 2011. p. 177–86.
Ghandhari H, Tari HV, Ameri E, Safari MB, Fouladi DF. Vertebral, rib, and intraspinal anomalies in congenital scoliosis: a study on 202 Caucasians. Eur Spine J. 2015;24:1510–21.
Shen J, Wang Z, Liu J, Xue X, Qiu G. Abnormalities associated with congenital scoliosis: a retrospective study of 226 Chinese surgical cases. Spine. 2013;38:814–8.
Xue X, Shen J, Zhang J, Zhao H, Li S, Wang Y, et al. An analysis of thoracic cage deformities and pulmonary function tests in congenital scoliosis. Eur Spine J. 2015;24:1415–21.
Schievink WI. Genetics of Intracranial Aneurysms. Neurosurgery. 1997;40:651–63.
Collins V. Brain tumours: classification and genes. J Neurol Neurosurg Psychiatry. 2004;75:ii2–ii11.
Al-Otibi M, Rutka JT. Neurosurgical implications of neurofibromatosis Type I in children. Neurosurg Focus. 2006;20:1–6.
Zadnik PL, Gokaslan ZL, Burger PC, Bettegowda C. Spinal cord tumours: advances in genetics and their implications for treatment. Nat Rev Neurol. 2013;9:257.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Moningi, S., Raju, S. (2019). Neuroanesthesia and Coexisting Genetic Problems. In: Prabhakar, H., Singhal, V., Gupta, N. (eds) Co-existing Diseases and Neuroanesthesia. Springer, Singapore. https://doi.org/10.1007/978-981-13-2086-6_13
Download citation
DOI: https://doi.org/10.1007/978-981-13-2086-6_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2085-9
Online ISBN: 978-981-13-2086-6
eBook Packages: MedicineMedicine (R0)