Abstract
The short supply of donor organs has been one of the most critical problems in the area of lung transplantation (LTx), and this is especially serious in Japan. One approach to attempt to address this limitation is the use of extended criteria donor (ECD) lungs. The currently accepted criteria for suitable donor lungs (Table 7.1) were instituted in the mid-1980s during the early development of clinical LTx [1]. These criteria were chosen by early transplant physicians and surgeons based on prevailing knowledge of pulmonary physiology, but were not based upon strict scientific evidence [2]. Afterward the ever-increasing number of recipients on waiting lists compelled lung transplant doctors to consider the use of ECD lungs. Liberalization of the donor selection criteria has been gradually accepted worldwide since the mid-1990s [2]. A recent large registry study of more than ten thousand LTxs performed in the USA from 1999 to 2008 revealed that at least one variance from the criteria occurred in more than a half of transplants [3]. Although results have varied among studies, outcomes of LTx using ECD lungs have generally been acceptable [4–18]. However, proper judgment is still difficult if multiple factors are defined extended and if ECD lungs are used in high-risk recipients especially who are rapidly deteriorating on the waiting list. To properly assess and optimize ECD lungs in such circumstances, a new strategy utilizing normothermic ex vivo lung perfusion (EVLP) system has been developed, and the impact of the system on LTx has been explored in several high-flow transplant centers [19, 20].
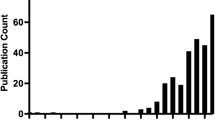
In Japan, 124 LTxs from deceased donors have been successfully performed as of the end of 2012 [21]. These transplantations achieved a 5-year patient survival rate of 72.0 % and a 10-year survival of 57.3 % [21]. To maximize the lung utilization rate in multiorgan donors, Japan Organ Transplant Network has operated a system involving the partnership of well-trained transplant consultant doctors and local doctors in assessing donor lungs and providing intensive care to donors since 2002 [22]. These consultant doctors tirelessly performed bronchial toileting for donors and provided advice on respiratory therapy, mechanical ventilation, infection controls, and circulatory management of donors. Since such sustained efforts by the consultant doctors in cooperation with local doctors have been made to effectively utilize ECD lungs, the lungs were used for transplantation in more than 60 % of brain-dead donors [22].
This chapter reviews definition and assessment methods of ECD lungs, studies showing outcomes of LTx using ECDs, and progress in recent research regarding ECD lungs.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Sundaresan S, Trachiotis G, Aoe M, Patterson G, Cooper J. Donor lung procurement: assessment and operative technique. Ann Thorac Surg. 1993;56:1409–13.
Gabbay E, Williams TJ, Griffiths AP, Macfarlane LM, Kotsimbos TC, Esmore DS, Snell GI. Maximizing the utilization of donor organs offered for lung transplantation. Am J Respir Crit Care Med. 1999;160(1):265–71.
Reyes KG, Mason DP, Thuita L, Nowicki ER, Murthy SC, Pettersson GB, Blackstone EH. Guidelines for donor lung selection: time for revision? Ann Thorac Surg. 2010;89(6):1756–64.
Kron IL, Tribble CG, Kern JA, Daniel TM, Rose CE, Truwit JD, Blackbourne LH, Bergin JD. Successful transplantation of marginally acceptable thoracic organs. Ann Surg. 1993;217(5):518–22.
Sundaresan S, Semenkovich J, Ochoa L, Richardson G, Trulock EP, Cooper JD, Patterson GA. Successful outcome of lung transplantation is not compromised by the use of marginal donor lungs. J Thorac Cardiovasc Surg. 1995;109(6):1075–9.
Bhorade SM, Vigneswaran W, McCabe MA, Garrity ER. Liberalization of donor criteria may expand the donor pool without adverse consequence in lung transplantation. J Heart Lung Transplant. 2000;19(12):1199–204.
Oto T, Griffiths AP, Levvey B, Pilcher DV, Whitford H, Koshimbos TC, Rabinov M, Esmore DS, Williams TJ, Snell GI. A donor history of smoking affects early but not late outcomes in lung transplantation. Transplantation. 2004;78:599–606.
Thabut G, Mal H, Cerrina J, Dartevelle P, Dromer C, Velly JF, Stern M, Loirat P, Bertocchi M, Mornex JF, Haloun A, Despins P, Pison C, Blin D, Simonneau G, Reynaud-Gaubert M. Influence of donor characteristics on outcome after lung transplantation: a multicenter study. J Heart Lung Transplant. 2005;24(9):1347–53.
Lardinois D, Banysch M, Korom S, Hillinger S, Rousson V, Boehler A, Speich R, Weder W. Extended donor lungs: eleven years experience in a consecutive series. Eur J Cardiothorac Surg. 2005;27(5):762–7.
Aigner C, Winkler G, Jaksch P, Seebacher G, Lang G, Taghavi S, Wisser W, Klepetko W. Extended donor criteria for lung transplantation–a clinical reality. Eur J Cardiothorac Surg. 2005;27(5):757–61.
Kawut SM, Reyentovich A, Wilt JS, Anzeck R, Lederer DJ, O'Shea MK, Sonett JR, Arcasoy SM. Outcomes of extended donor lung recipients after lung transplantation. Transplantation. 2005;79(3):310–6.
Luckraz H, White P, Sharples LD, Hopkins P, Wallwork J. Short- and long-term outcomes of using pulmonary allograft donors with low Po2. J Heart Lung Transplant. 2005;24(4):470–3.
Botha P, Trivedi D, Weir CJ, Searl CP, Corris PA, Dark JH, Schueler SV. Extended donor criteria in lung transplantation: impact on organ allocation. J Thorac Cardiovasc Surg. 2006;131(5):1154–60.
De Perrot M, Waddell TK, Shargall Y, Pierre AF, Fadel E, Uy K, Chaparro C, Hutcheon M, Singer LG, Keshavjee S. Impact of donors aged 60 years or more on outcome after lung transplantation: results of an 11-year single-center experience. J Thorac Cardiovasc Surg. 2007;133(2):525–31.
Meers C, Van Raemdonck D, Verleden GM, Coosemans W, Decaluwe H, De Leyn P, Nafteux P, Lerut T. The number of lung transplants can be safely doubled using extended criteria donors; a single-center review. Transpl Int. 2010;23(6):628–35.
Berman M, Goldsmith K, Jenkins D, Sudarshan C, Catarino P, Sukumaran N, Dunning J, Sharples LD, Tsui S, Parmar J. Comparison of outcomes from smoking and nonsmoking donors: thirteen-year experience. Ann Thorac Surg. 2010;90(6):1786–92.
Zafar F, Khan MS, Heinle JS, Adachi I, McKenzie ED, Schecter MG, Mallory GB, Morales DL. Does donor arterial partial pressure of oxygen affect outcomes after lung transplantation? A review of more than 12,000 lung transplants. J Thorac Cardiovasc Surg. 2012;143(4):919–25.
Bonser RS, Taylor R, Collett D, Thomas HL, Dark JH, Neuberger J, Cardiothoracic Advisory Group to NHS Blood and Transplant and the Association of Lung Transplant Physicians (UK). Effect of donor smoking on survival after lung transplantation: a cohort study of a prospective registry. Lancet. 2012;380(9843):747–55.
Steen S, Sjoerg T, Pierre L, Liao Q, Eriksson L, Algotsson L. Transplantation of lungs from a non-heart-beating donor. Lancet. 2001;357(9259):825–9.
Cypel M, Yeung JC, Liu M, et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med. 2011;364(15):1431–40.
Registry Report. 2013. http://www2.idac.tohoku.ac.jp/dep/surg/shinpai/pg185.html
Egawa H, Tanabe K, Fukushima N, Date H, Sugitani A, Haga H. Current status of organ transplantation in Japan. Am J Transplant. 2012;12(3):523–30.
Orens JB, Boehler A, Perrot M, Estenne M, Glanville AR, Keshavjee S, Kotloff R, Morton J, Studer SM, Van Raemdonck D, Waddel T, Snell GI. A review of lung transplant donor acceptability criteria. J Heart Lung Transplant. 2003;22:1183–200.
Pierre AF, Sekine Y, Hutcheon MA, Waddell TK, Keshavjee SH. Marginal donor lungs: a reassessment. J Thorac Cardiovasc Surg. 2002;123(3):421–7.
Steen S, Sjoerg T, Ingemansson R, Lindberg L. Efficacy of topical cooling in lung preservation: is a reappraisal due? Ann Thorac Surg. 1994;58(6):1657–63.
Fisher AJ, Donnelly SC, Hirani N, Haslett C, Strieter RM, Dark JH, Corris PA. Elevated levels of interleukin-8 in donor lungs is associated with early graft failure after lung transplantation. Am J Respir Crit Care Med. 2001;163(1):259–65.
Kaneda H, Waddell TK, de Perrot M, Bai XH, Gutierrez C, Arenovich T, Chaparro C, Liu M, Keshavjee S. Pre-implantation multiple cytokine mRNA expression analysis of donor lung grafts predicts survival after lung transplantation in humans. Am J Transplant. 2006;6(3):544–51.
Meyer DM, Bennett LE, Novick RJ, Hosenpud JD. Effect of donor age and ischemic time on intermediate survival and morbidity after lung transplantation. Chest. 2000;118(5):1255–562.
Pizanis N, Heckmann J, Tsagakis K, Tossios P, Massoudy P, Wendt D, Jakob H, Kamler M. Lung transplantation using donors 55 years and older: is it safe or just a way out of organ shortage? Eur J Cardiothorac Surg. 2010;38(2):192–7.
Stewart S, Ciulli F, Wells F, Wallwork J. Pathology of unused donor lungs. Transplant Proc. 1993;25:1167–8.
Ware LB, Fang X, Wang Y, Babcock WD, Jones K, Matthay MA. High prevalence of pulmonary arterial thrombi in donor lungs rejected for transplantation. J Heart Lung Transplant. 2005;24:1650–6.
Oto T, Rabinov M, Griffiths AP, Whitford H, Levvey BJ, Esmore DS, Williams TJ, Snell GI. Unexpected donor pulmonary embolism affects early outcomes after lung transplantation: a major mechanism of primary graft failure? J Thorac Cardiovasc Surg. 2005;130:1446–52.
Ware LB, Fang X, Wang Y, Sakuma T, Hall TS, Matthay MA. Selected contribution: mechanisms that may stimulate the resolution of alveolar edema in the transplanted human lung. J Appl Physiol. 2002;93:1869–74.
Motoyama H, Chen F, Ohsumi A, Hijiya K, Okita K, Nakajima D, Sakamoto J, Yamada T, Sato M, Aoyama A, Bando T, Date H. Protective effect of plasmin in marginal donor lungs in an ex vivo lung perfusion model. J Heart Lung Transplant. 2013;32(5):505–10.
Warnecke G, Moradiellos J, Tudorache I, Kühn C, Avsar M, Wiegmann B, Sommer W, Ius F, Kunze C, Gottlieb J, Varela A, Haverich A. Normothermic perfusion of donor lungs for preservation and assessment with the organ care system lung before bilateral transplantation: a pilot study of 12 patients. Lancet. 2012;380(9856):1851–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Japan
About this chapter
Cite this chapter
Hoshikawa, Y., Okada, Y., Watanabe, T., Kondo, T. (2014). ECD for Lung Transplantation. In: Asano, T., Fukushima, N., Kenmochi, T., Matsuno, N. (eds) Marginal Donors. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54484-5_7
Download citation
DOI: https://doi.org/10.1007/978-4-431-54484-5_7
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54483-8
Online ISBN: 978-4-431-54484-5
eBook Packages: MedicineMedicine (R0)