Abstract
In October 1997, the Japanese Organ Transplant Act was issued and we needed to successfully start the first heart transplantation (HTx) in Japan. For this reason, very strict criteria for the donor heart were established by the task force committee for heart transplantation in the Ministry of Health, Labour and Welfare. These criteria were comparable to the so-called standard criteria for the donor heart in the world.
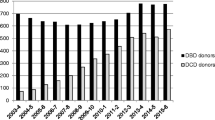
On February 28, 1999, the first HTx was successfully performed in Japan [1] and 227 HTx were done up to the end of August 2012. Although many efforts to shorten the transportation time of the heart were done, mean transportation and total ischemic time were about 2 and 3 h, respectively. On the other hand, as the Japanese Organ Transplant Act was very strict, brain-dead organ donation was extremely limited in Japan and only 184 brain-dead donors were available for 13 years after the Act was issued. In order to respond to the will of the donor and donor families, we needed to transplant the heart as much as possible. For these reasons, more hearts should be transplanted from the extended criteria donor (ECD) in Japan than other developed countries.
Since brain-dead organ transplantation was started in 1999, every organ procurement team has taken their own skillful physicians to the procurement hospital [2]. They evaluated the condition of donor organs by echocardiography and flexible bronchofiberscopy (BFS) by themselves in the intensive care unit (ICU), before procurement operation [2].
Since November of 2002, special transplant management doctors (a medical consultant, MC) have been sent to the procurement hospital. They assessed donor organ function and identified which organs were useful for transplantation. They also intensively cared for the donor, stabilized the donor hemodynamics by giving antidiuretic hormone (ADH) and reducing the dose of intravenous catecholamine as much as possible, and improved donor cardiac and lung function by preventing and treating lung infection before procurement teams arrived at the donor hospital.
Out of 184 brain-dead donors, 136 heart, 1 heart–lung, 143 lung, 159 liver, 1,311 pancreas, and 12 small bowel transplants were performed. Organs transplanted per one donor (OTPD) increased to 5.5 organs after these strategies were applied.
Although 83 of 136 heart donors were ECD, no recipient died of primary graft dysfunction (PGD).
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Matsuda H, Fukushima N, Sawa Y, Nishimura M, Matsumiya G, Shirakura R. First brain dead donor heart transplantation under new legislation in Japan. Jpn J Thorac Cardiovasc Surg. 1999;47:499–505.
Fukushima N, Ono M, Nakatani T, et al. Strategies for maximizing heart and lung transplantation opportunities in Japan. Transplant Proc. 2009;41(1):273–6.
Bailey LL, Razzouk AJ, Hasaniya NW, Chinnock RE. Pediatric transplantation using hearts refused on the basis of donor quality. Ann Thorac Surg. 2009;87(6):1902–8. discussion 1908–9.
Stehlik J, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for heart and lung transplantation: twenty-eighth official adult heart transplant report–2011. J Heart Lung Transplant. 2011;30(10):1071–132.
Fukushima N, Shirakura R, Nakata S, et al. Study of efficacies of leukocyte-depleted terminal blood cardioplegia in 24-hour preserved hearts. Ann Thorac Surg. 1994;58(6):1651–6.
Laks H, Gates RN, Ardehali A, et al. Orthotopic heart transplantation and concurrent coronary bypass. J Heart Lung Transplant. 1993;12:810–5.
Marelli D, Laks H, Bresson S, et al. Results after transplantation using donor hearts with preexisting coronary artery disease. J Thorac Cardiovasc Surg. 2003;126:821.
Russo MJ, Iribarne A, Hong KN, et al. Factors associated with primary graft failure after heart transplantation. Transplantation. 2010;90(4):444–50.
Mattner F, Kola A, Fischer S, et al. Impact of bacterial and fungal donor organ contamination in lung, heart–lung, heart and liver transplantation. Infection. 2008;36:207–12.
Pinney SP, Cheema FH, Hammond K, et al. Acceptable recipient outcomes with the use of hearts from donors with hepatitis-B core antibodies. J Heart Lung Transplant. 2005;24:34–7.
Grauhan O. Screening and assessment of the donor heart. Cardiopulm Pathophysiol. 2011;15:191–7.
Young JB, Naftel DC, Bourge RC, et al. Matching the heart donor and heart transplant recipient. Clues for successful expansion of the donor pool: a multivariable, multiinstitutional report. The Cardiac Transplant Research Database Group. J Heart Lung Transplant. 1994;13:353–65.
Grauhan O, Siniawski H, Dandel M, et al. Coronary atherosclerosis of the donor heart: impact on early graft failure. Eur J Cardiothorac Surg. 2007;32(4):634–8.
Musci M, Pasic M, Grauhan O, et al. Orthotopic heart transplantation with concurrent coronary artery bypass grafting or previous stent implantation. Z Kardiol. 2004;93:971–4.
Nilsson B, Berggren H, Ekroth R, et al. Glucose-insulin-potassium (GIK) prevents derangement of myocardial metabolism in brain-dead pigs. Eur J Cardiothorac Surg. 1994;8(8):442–6.
Wheeldon DR, Potter CD, Odura A, Wallwork J, Large SR. Transforming the “unacceptable” donor: outcomes from the adoption of a standardized donor management technique. J Heart Lung Transplant. 1995;14(4):734–42.
Zaroff JG, Rosengard B, Armstrong WF, et al. Maximizing use of organs recovered from the cadaver donor: cardiac recommendations. (Consensus Conference Report, March 28–29, 2001, Crystal City). J Heart Lung Transplant. 2002;21(11):1153–60.
Epinat JC, Gilmore TD. Diverse agents act at multiple levels to inhibit the Rel/NF-Kappa B signal transduction pathway. Oncogene. 1999;18:6896–909.
Sakaguchi T, Sawa Y, Fukushima N, et al. A novel strategy of decoy transfection against nuclear factor-kappaB in myocardial preservation. Ann Thorac Surg. 2001;71(2):624–9. discussion 629–30.
Reddy SP, Brockmann J, Friend PJ. Normothermic perfusion: a mini-review. Transplantation. 2009;87:631–2.
Sawa Y, Taniguchi K, Kadoba K, Nishimura M, et al. Leukocyte depletion attenuates reperfusion injury in patients with left ventricular hypertrophy. Circulation. 1996;93(9):1640–6.
Pearl J, Drinkwater DC, Laks H, Capouya ER, Gates RN. Leukocyte depleted reperfusion of transplanted human hearts: a randomized, double blind clinical trial. J Heart Lung Transplant. 1992;11:1082–92.
Sawa Y, Matsuda H, Shimazaki T, Kaneko M, Nishimura M, Amemiya A, et al. Evaluation of leukocyte depleted terminal blood cardioplegic solution in patients undergoing elective and emergency coronary artery bypass grafting. J Thorac Cardiovasc Surg. 1994;108(6):1125–31.
Fukushima N, Shirakura R, Nakata S, et al. Effects of terminal cardioplegia with leukocyte-depleted blood on heart grafts preserved for 24 hours. J Heart Lung Transplant. 1992;11(4 Pt 1):676–82.
Fukushima N, Miyamoto Y, Ohtake S, et al. Early result of heart transplantation in Japan: Osaka University experience. Asian Cardiovasc Thorac Ann. 2004;12(2):154–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Japan
About this chapter
Cite this chapter
Fukushima, N. (2014). ECD for Heart Transplantation. In: Asano, T., Fukushima, N., Kenmochi, T., Matsuno, N. (eds) Marginal Donors. Springer, Tokyo. https://doi.org/10.1007/978-4-431-54484-5_4
Download citation
DOI: https://doi.org/10.1007/978-4-431-54484-5_4
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-54483-8
Online ISBN: 978-4-431-54484-5
eBook Packages: MedicineMedicine (R0)