Abstract
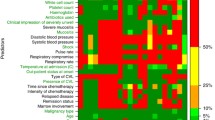
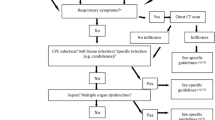
Although the risk of developing fever and infection is already increased when a patient’s neutrophil granulocyte counts fall below 1,000 per mm3, counts of less than 500 per mm3 have been demonstrated to be the most critical risk factor for the development of serious infectious complications. Expert groups of the Infectious Diseases Society of America (IDSA), the European Conference on Infections in Leukaemia (ECIL), the Multinational Association for Supportive Care in Cancer, the American Society of Clinical Oncology, and the German Society of Hematology and Oncology have categorized neutropenic patients into distinct subgroups with different risk profiles depending upon their duration of neutropenia (see also the chapter by Paesmans). While a strict prospective allocation of all patients to distinct risk groups is not possible in clinical practice, patients with neutropenia lasting for up to 7 days, who have no additional risk factors such as open wounds and tumor-associated obstruction of airways or bile ducts, e.g., patients with malignant lymphoma on standard chemotherapy, are regarded as low-risk patients. In contrast, patients with aggressive hematologic malignancies such as acute leukemias undergoing intensive chemotherapy, who have an expected duration of profound neutropenia of more than 7 days, represent a high-risk group. Sometimes, patients with an expected neutropenia of 7–10 days, e.g., those with lymphomas receiving dose-intensified treatment regimens, are regarded as a separate, so-called intermediate or standard risk group.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Bhusal Y, Mihu CN, Tarrand JJ, Rolston KV. Incidence of fluoroquinolone-resistant and extended-spectrum β-lactamase-producing Escherichia coli at a comprehensive cancer center in the United States. Chemotherapy. 2011;57:335–8.
Blijlevens NM, Donnelly JP, Meis JF, De Keizer MH, De Pauw BE. Procalcitonin does not discriminate infection from inflammation after allogeneic bone marrow transplantation. Clin Diagn Lab Immunol. 2000;7:889–92.
Cherif H, Johansson E, Björkholm M, Kalin M. The feasibility of early hospital discharge with oral antimicrobial therapy in low risk patients with febrile neutropenia following chemotherapy for hematologic malignancies. Haematologica. 2006;91:215–22.
Cometta A, Kern WV, De Bock R, Paesmans M, Vandenbergh M, Crokaert F, Engelhard D, Marchetti O, Akan H, Skoutelis A, Korten V, Vandercam M, Gaya H, Padmos A, Klastersky J, Zinner S, Glauser MP, Calandra T, Viscoli C, International Antimicrobial Therapy Group of the European Organization for Research Treatment of Cancer. Vancomycin versus placebo for treating persistent fever in patients with neutropenic cancer receiving piperacillin-tazobactam monotherapy. Clin Infect Dis. 2003;37:382–9.
Del Favero A, Menichetti F, Martino P, Bucaneve G, Micozzi A, Gentile G, Furno P, Russo D, D’Antonio D, Ricci P, Martino B, Mandelli F. A multicenter, double-blind, placebo-controlled trial comparing piperacillin-tazobactam with and without amikacin as empiric therapy for febrile neutropenia. Clin Infect Dis. 2001;33:1295–301.
Erjavec Z, de Vries-Hospers HG, Laseur M, Halie RM, Daenen S. A prospective, randomized, double-blinded, placebo-controlled trial of empirical teicoplanin in febrile neutropenia with persistent fever after imipenem monotherapy. J Antimicrob Chemother. 2000;45:843–9.
Flowers CR, Seidenfeld J, Bow EJ, Karten C, Gleason C, Hawley DK, Kuderer NM, Langston AA, Marr KA, Rolston KV, Ramsey SD. Antimicrobial prophylaxis and outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2013;31:794–810.
Freifeld A, Marchigiani D, Walsh T, Chanock S, Lewis L, Hiemenz J, Hiemenz S, Hicks JE, Gill V, Steinberg SM, Pizzo PA. A double-blind comparison of empirical oral and intravenous antibiotic therapy for low-risk febrile patients with neutropenia during cancer chemotherapy. N Engl J Med. 1999;341:305–11.
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR. Infectious Diseases Society of America. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52:e56–93.
Heussel CP, Kauczor HU, Heussel GE, Fischer B, Begrich M, Mildenberger P, Thelen M. Pneumonia in febrile neutropenic patients and in bone marrow and stem cell transplant recipients: use of high-resolution computed tomography. J Clin Oncol. 1999;17:796–805.
Ho DY, Lin M, Schaenman J, Rosso F, Leung AN, Coutre SE, Sista RR, Montoya JG. Yield of diagnostic procedures for invasive fungal infections in neutropenic febrile patients with chest computed tomography abnormalities. Mycoses. 2011;54:59–70.
Kern WV, Cometta A, DeBock R, Langenaeken J, Paesmans M, Gaya H. Oral versus intravenous empirical antimicrobial therapy for fever in patients with granulocytopenia who are receiving cancer chemotherapy. N Engl J Med. 1999;341:312–8.
Kern WV, Marchetti O, Drgona L, Akan H, Aoun M, Akova M, de Bock R, Paesmans M, Viscoli C, Calandra T. Oral antibiotics for fever in low-risk neutropenic patients with cancer: a double-blind, randomized, multicenter trial comparing single daily moxifloxacin with twice daily ciprofloxacin plus amoxicillin/clavulanic acid combination therapy – EORTC infectious diseases group trial X. J Clin Oncol. 2013;31:1149–56.
Klastersky J, Paesmans M, Georgala A, Muanza F, Plehiers B, Dubreucq L, Lalami Y, Aoun M, Barette M. Outpatient oral antibiotics for febrile neutropenic cancer patients using a score predictive for complications. J Clin Oncol. 2006;24:4129–34.
Klastersky J, Paesmans M. The Multinational Association for Supportive Care in Cancer (MASCC) risk index score: 10 years of use for identifying low-risk febrile neutropenic cancer patients. Support Care Cancer. 2013;21:1487–95.
Lehrnbecher T, Phillips R, Alexander S, Alvaro F, Carlesse F, Fisher B, Hakim H, Santolaya M, Castagnola E, Davis BL, Dupuis LL, Gibson F, Groll AH, Gaur A, Gupta A, Kebudi R, Petrilli S, Steinbach WJ, Villarroel M, Zaoutis T, Sung L. Guideline for the management of fever and neutropenia in children with cancer and/or undergoing hematopoietic stem-cell transplantation. J Clin Oncol. 2012;30:4427–38.
Link H, Maschmeyer G, Meyer P, Hiddemann W, Stille W, Helmerking M, Adam D. Interventional antimicrobial therapy in febrile neutropenic patients. Study group of the Paul Ehrlich society for chemotherapy. Ann Hematol. 1994;69:231–43.
Link H, Böhme A, Cornely OA, Höffken K, Kellner O, Kern WV, Mahlberg R, Maschmeyer G, Nowrousian MR, Ostermann H, Ruhnke M, Sezer O, Schiel X, Wilhelm M, Auner HW. Antimicrobial therapy of unexplained fever in neutropenic patients. Ann Hematol. 2003;82 Suppl 2:S105–17.
Maschmeyer G, Heinz WJ, Hertenstein B, Horst HA, Requadt C, Wagner T, Cornely OA, Löffler J, Ruhnke M, On Behalf of the IDEA Study Investigators. Immediate versus deferred empirical antifungal (IDEA) therapy in high-risk patients with febrile neutropenia: a randomized, double-blind, placebo-controlled, multicenter study. Eur J Clin Microbiol Infect Dis. 2013;32:679–89.
Meunier F, Zinner SH, Gaya H, Calandra T, Viscoli C, Klastersky J, Glauser M. Prospective randomized evaluation of ciprofloxacin versus piperacillin plus amikacin for empiric antibiotic therapy of febrile granulocytopenic cancer patients with lymphomas and solid tumors. The European Organization for Research on Treatment of Cancer International Antimicrobial Therapy Cooperative Group. Antimicrob Agents Chemother. 1991;35:873–8.
Pagano L, Girmenia C, Mele L, Ricci P, Tosti ME, Nosari A, Buelli M, Picardi M, Allione B, Corvatta L, D’Antonio D, Montillo M, Melillo L, Chierichini A, Cenacchi A, Tonso A, Cudillo L, Candoni A, Savignano C, Bonini A, Martino P, Del Favero A, GIMEMA Infection Program, Gruppo Italiano Malattie Ematologiche dell’Adulto. Infections caused by filamentous fungi in patients with hematologic malignancies. A report of 391 cases by GIMEMA Infection Program. Haematologica. 2001;86:862–70.
Paul M, Yahav D, Fraser A, Leibovici L. Empirical antibiotic monotherapy for febrile neutropenia: systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2006;57:176–89.
Robinson JO, Lamoth F, Bally F, Knaup M, Calandra T, Marchetti O. Monitoring procalcitonin in febrile neutropenia: what is its utility for initial diagnosis of infection and reassessment in persistent fever? PLoS One. 2011;6:e18886.
Rubenstein EB, Rolston K, Benjamin RS, Loewy J, Escalante C, Manzullo E, Hughes P, Moreland B, Fender A, Kennedy K, Holmes F, Elting L, Bodey GP. Outpatient treatment of febrile episodes in low-risk neutropenic patients with cancer. Cancer. 1993;71:3640–6.
Vehreschild MJ, Vehreschild JJ, Hübel K, Hentrich M, Schmidt-Hieber M, Christopeit M, Maschmeyer G, Schalk E, Cornely OA, Neumann S. Diagnosis and management of gastrointestinal complications in adult cancer patients: evidence-based guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Oncol. 2013;24:1189–202.
von Lilienfeld-Toal M, Dietrich MP, Glasmacher A, Lehmann L, Breig P, Hahn C, Schmidt-Wolf IG, Marklein G, Schroeder S, Stuber F. Markers of bacteremia in febrile neutropenic patients with hematologic malignancies: procalcitonin and IL-6 are more reliable than C-reactive protein. Eur J Clin Microbiol Infect Dis. 2004;23:539–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Maschmeyer, G. (2015). Fever of Unknown Origin: Treatment According to Risk Assessment. In: Maschmeyer, G., Rolston, K. (eds) Infections in Hematology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-44000-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-662-44000-1_9
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-43999-9
Online ISBN: 978-3-662-44000-1
eBook Packages: MedicineMedicine (R0)