Abstract
Infectious and noninfectious pulmonary diseases are commonly found on postmortem autopsy studies in patients with hematological malignancy. Despite the technological advances in diagnostic testing and imaging modalities, obtaining an accurate clinical diagnosis remains difficult and often not possible until autopsy. Major diagnostic discrepancies between clinical premortem diagnoses and postmortem autopsy findings have been reported in these patients. The most common missed diagnoses are due to opportunistic infections and cardiopulmonary complications. These findings underscore the importance of enhanced surveillance, monitoring and treatment of infections and cardiopulmonary disorders in these patients. Autopsies remain important in determining an accurate cause of death and for improved understanding of diagnostic deficiencies, as well as for medical education and quality assurance.
The authors state that they do not have any conflicts of interest.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Acute Myeloid Leukemia
- Hematopoietic Stem Cell Transplantation
- Invasive Candidiasis
- Immune Reconstitution Inflammatory Syndrome
- Invasive Pulmonary Aspergillosis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Infectious and noninfectious pulmonary complications occur in 30–60% of patients with hematological malignancy and recipients of hematopoietic stem cell transplantation (HSCT) and are associated with significant morbidity and mortality [1]. In allogeneic HSCT patients who develop respiratory failure requiring mechanical ventilation, the intensive care unit (ICU) and hospital mortality rates often exceed 80% and 85%, respectively [2–5]. The factors that contribute to the development of pulmonary complications in these patients include immunologic defects due to the underlying disease and its treatment, conditioning regimens, development of graft-versus-host disease (GVHD), and the type of HSCT [2, 6, 7]. The spectrum of pulmonary complications in patients with hematological malignancy and HSCT recipients is changing because of recent advances in antineoplastic therapies, such as the use of monoclonal antibodies and other targeted agents, increased application of HSCT for older patients, widespread use of prophylactic antibiotics and novel antimicrobial agents, and advances in supportive care [8].
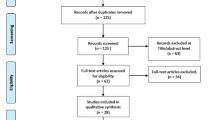
Prompt investigation and diagnosis of pulmonary complications in patients with hematological malignancies are essential to improving patient survival. Unfortunately, despite the technological advances in diagnostic testing and imaging modalities, obtaining an accurate clinical diagnosis in these patients remains difficult and at times is made only at the time of the postmortem autopsy examination. Autopsy rates in cancer patients are much lower (13–34%) as compared to general medical and surgical patients (53–64%) [7–9]. This probably reflects the unwillingness on the part of physicians and family members to subject the cancer patient to the same level of scrutiny applied to other major illnesses in determining the primary and contributory causes of death [9]. Additional concerns include legal issues regarding exposition of physicians’ errors and non-reimbursement for postmortem examinations [10].
This chapter will review the infectious and noninfectious pulmonary findings that have been described at autopsy in patients with hematological malignancies, including blood and bone marrow transplant recipients. In addition, we discuss the frequently noted diagnostic discrepancies between premortem clinical diagnoses and postmortem autopsy findings in these patients. Finally, we highlight the difficulties in diagnosing many of these conditions antemortem and emphasize the important role of the postmortem examination in accurately establishing the cause of death. Table 20.1 lists the infectious and non-infectious pulmonary disorders reported in autopsy studies of patients with hematologic malignancy, including HSCT recipients.
2 Infectious Findings
2.1 Invasive Fungal Infections
The incidence of invasive fungal infections in patients with hematologic malignancies has increased steadily over the past three decades [11]. This has been attributed to improvements in the prevention or preemptive treatment of bacterial infections and other opportunistic pathogens, particularly Candida and cytomegalovirus; increased administration of chemotherapies with profound and prolonged immunosuppressive effects on T-cell function (e.g., purine nucleoside analogs, anti-T-cell immunoglobulin, and monoclonal antibodies); and the growing number of allogeneic and nonmyeloablative transplantation procedures that carry a higher risk for chronic GVHD [12]. Patients with hematologic malignancies, especially in the neutropenic state after aggressive chemotherapy or HSCT and HSCT recipients with GVHD, are particularly susceptible to invasive fungal infections [13]. Approximately 20–50% of patients with hematological malignancies and HSCT recipients have evidence of invasive fungal infections at autopsy [8]. These include invasive aspergillosis and fungal infections due to Candida spp., Zygomycetes spp., Trichosporon spp., Fusarium spp., and various Chaetomium species.
In neutropenic patients with acute leukemia, the histopathological pattern of invasive pulmonary aspergillosis (IPA) is characterized by scant inflammation, hyphal angioinvasion with a high fungal burden, and extensive coagulative necrosis [12, 14]. In contrast, among HSCT recipients with GVHD, the histopathological findings consist of severe lung inflammation and less abundant Aspergillus burden. Several autopsy studies in HSCT recipients have shown that IPA is frequently not diagnosed antemortem or persistent despite diagnosis by sputum or bronchoalveolar lavage (BAL) cultures or by serum galactomannan assay and treatment with amphotericin B [8, 15–21]. In recent years, treatment of IPA with voriconazole has led to better responses, improved survival rates, and fewer side effects than amphotericin B [22].
Autopsy studies have assisted in describing and confirming the immune reconstitution inflammatory syndrome (IRIS) in patients with IPA who are recovering from the neutropenia [23]. When clinical and radiologic worsening coincides with neutrophil recovery, it is usually assumed that this deterioration is related to progressive aspergillosis, prompting changes in patient management. However, its temporal relation with neutrophil recovery suggests that it may be caused by IRIS. The patients who died during the first month had no evidence of aspergillosis at autopsy. Finally, autopsy studies have proved helpful in documenting the efficacy of systemic antifungal therapy and surgery for IPA [24].
Since the early 1990s, the incidence of invasive candidiasis (candidemia and/or hepatosplenic candidiasis) has continued to decrease due to effective antifungal prophylaxis and empirical treatment of high-risk patients with echinocandins and voriconazole [11]. Mucosal damage is a risk factor for invasive candidiasis among patients receiving antineoplastic therapy. HSCT recipients who received conditioning regimens with total body irradiation and patients treated with chemotherapy regimens containing high-dose cytarabine or an anthracycline have an increased risk of developing invasive disease. In recent years, there has been an increase in bloodstream infections caused by non-albicans Candida species such as Candida glabrata and C. krusei. The diagnosis of invasive candidiasis is difficult to prove due to the lack of specific clinical features and the low sensitivity of blood cultures to isolate Candida, especially in patients receiving fluconazole prophylaxis [25].
Difficult-to-treat opportunistic molds, such as Zygomycetes, Trichosporon spp., and various Chaetomium spp., including C. atrobrunneum, C. strumarium, C. globosum, C. perlucidum, and C. cinereus are being described with increasing frequency on autopsy studies in patients with hematologic malignancies [12, 26–31]. Pulmonary involvement with these mold infections is characterized by tissue necrosis from angioinvasion and subsequent thrombosis. As with many fungal infections, diagnosis of these infections is often not possible until autopsy. Treatment modalities usually involve lipid-based amphotericin B formulations and surgical debulking or debridement in selected cases [32].
2.2 Pneumocystis Jiroveci (Formerly Carinii) Pneumonia
Pneumocystis jiroveci pneumonia (PCP) remains a serious infection in patients with acute and chronic leukemias, myelodysplastic syndrome, and HSCT recipients [8]. However, diagnosis of PCP is frequently obtained by bronchoalveolar lavage with or without lung biopsy; thus, the diagnosis is made on autopsy in only a minority of cases.
2.3 Bacterial Infections
Bacterial pneumonias caused by Pseudomonas aeruginosa, Streptococcus spp., Staphylococcus aureus, Serratia spp., and Legionella pneumophila have been described on autopsy studies in patients with hematologic malignancy and HSCT recipients [33]. As the majority of these patients commonly receive empiric antimicrobial therapy during the initial diagnostic workup for infection, very few autopsy studies report unusual bacterial infections. A single center autopsy series of 15 patients with hematological malignancies found multidrug-resistant strains such as Enterococcus faecium to be very prevalent [34]. Two coagulase-negative Staphylococcus epidermidis strains were also noted. A few autopsy case reports have also described lethal pulmonary hemorrhage due to Stenotrophomonas maltophilia [35].
2.4 Viruses
The incidence of autopsy-proven cytomegalovirus (CMV) pneumonia in patients with hematologic malignancy and HSCT recipients has been decreasing in recent years as a result of improvements in early diagnosis and treatment and more effective preventive strategies [36]. However, it is also possible that the declining rate of autopsies may account for the decrease in the number of reported CMV pneumonias. Other etiologies of viral pneumonias that have been described in autopsy reports include infection due to herpes simplex virus, respiratory syncytial virus (RSV) [37], and measles virus [38].
2.5 Toxoplasmosis
Reactivation of latent Toxoplasmosis is a rare but well-recognized opportunistic infection in immunocompromised patients. Besides encephalitis, the other common presentation with Toxoplasma gondii infection is interstitial pneumonitis. Because of its non-specific clinical and radiological presentation and its lethal outcome, toxoplasmosis is often misdiagnosed and only revealed at autopsy [39]. Toxoplasmic pneumonitis follows the same pathogenetic mechanism, but occurs less frequently than either toxoplasmic encephalitis or other opportunistic pneumonias, such as PCP. Diagnosis is based upon a high degree of clinical suspicion and demonstration of T. gondii in BAL fluid and/or lung biopsy specimens. Widely disseminated necrotic areas with numerous cysts of Toxoplasma gondii are commonly reported in autopsy cases.
3 Noninfectious Pulmonary Findings
Noninfectious pulmonary complications account for up to 70% of autopsy findings in patients with hematologic malignancies, particularly in HSCT recipients. The most common complications are diffuse alveolar damage (DAD) and diffuse alveolar hemorrhage (DAH) [8].
3.1 Diffuse Alveolar Damage
Diffuse alveolar damage (DAD) is a nonspecific finding at autopsy often in association with various infectious and noninfectious etiologies, such as shock, aspiration, alveolar hemorrhage, peri-engraftment respiratory distress syndrome, drug toxicity, and radiation therapy. It is characterized by the presence of alveolar injury and the absence of active lower respiratory tract infection. DAD has been reported at autopsy in 63.5% of patients with treated leukemia and lymphoma and close to 50% among HSCT patients [7, 8]. Infections as the cause of DAD are identified on autopsy in only a third of HSCT patients, while approximately 20% have DAH. In over 50% of patients with DAD, no etiology is determined, and these patients are considered as having idiopathic pneumonia syndrome (IPS). It is possible that empirically treated previous infections could have caused the histological changes noted in patients classified as having IPS. Only one third of the cases of DAD are diagnosed antemortem [8]. Given that almost half of the cases of DAD may be secondary to IPS, the role of corticosteroids may need to be furthered studied.
3.2 Diffuse Alveolar Hemorrhage
Diffuse alveolar hemorrhage (DAH) is a clinical syndrome characterized by the acute onset of alveolar infiltrates, bloody bronchoalveolar lavage, and hypoxemia in the absence of infection [1, 40]. The incidence of DAH ranges from 1–5% to 3–7% in autologous and allogeneic HSCT recipients, respectively [41–43]. A few case reports have been described in patients with acute leukemia more commonly in association with chemotherapy [44–46]. DAH has also been described in patients undergoing an umbilical cord HSCT [47, 48]. The majority of patients with DAH develop severe respiratory failure with high mortality rates. Vascular damage and inflammation from chemotherapy and radiation therapy used in the conditioning regimen and immune-mediated events including GVHD have been implicated in the pathogenesis of DAH [41, 43, 49]. Wojno et al. reported that 41% of 37 allogeneic HSCT patients who underwent autopsies had extensive pulmonary hemorrhage, which was thought to have led to severe respiratory failure and death [49]. These patients were subdivided into those with significant acute GVHD and those without. Of the patients with acute GVHD, 59% died of acute respiratory failure secondary to DAH compared with 25% of those without GVHD. Pulmonary hemorrhage was also independently found to be associated with pre-transplant total body irradiation. Although pulmonary and systemic infections cause alveolar damage through similar mechanisms [50]. infection-associated alveolar damage has traditionally been excluded from analyses of DAH. Autopsy studies have shown that pulmonary infections are frequently underdiagnosed in HSCT recipients; thus, patients with alveolar hemorrhage and underlying undetected infections can be misclassified as having DAH [7, 8, 51].
Because inflammation is thought to play a role in the pathogenesis of post HSCT-DAH, high-dose steroids have been used for its treatment, based on anecdotal case reports and small retrospective series [52, 53]. Other treatment modalities that have been used for DAH in HSCT recipients include epsilon aminocaproic acid and recombinant factor VIIa [54, 55]. Unfortunately, the mortality from DAH in HSCT recipients remains high because of misdiagnosis and lack of effective treatments.
3.3 Lymphomatous or Leukemic Infiltration
Primary pulmonary lymphomas are very uncommon, especially those arising from bronchus-associated lymphoid tissue (BALT) and have a low mortality. They represent 4% of the extranodal non-Hodgkin’s lymphomas (NHLs) and only 0.5% of all primary pulmonary malignant neoplasms and less than 1% of lymphomas. Eighty percent of the cases are low-grade B-cell lymphomas, which are slow growing and respond well to therapy. Autopsy case reports suggest that pulmonary BALT lymphoma can remain restrictive to the thorax for long periods before dissemination, but tend to relapse frequently.
Lymphomatous involvement of the lung is common and occurs in 24% and 38%, respectively, of patients with Hodgkin’s lymphomas (HL) and NHL [56]. Typical findings in the lung include peribronchial-perivascular, nodular, alveolar, interstitial, and pleural involvement. Peripheral T-cell lymphomas also involve the lung frequently, 20% at diagnosis and a further 20% during the course of the disease. The nodular pattern is a characteristic of lung infiltration in HL, but no differences could be detected in the subtypes.
Pulmonary parenchymal involvement by multiple myeloma cells is very rare and described on autopsy in few case reports. The antemortem diagnosis of lung involvement by myeloma is difficult to make as infections and alveolar hemorrhage can have the same radiologic features.
Leukemic infiltration of the lungs may occur in 20–30% of hyperleucocytic patients with acute myeloid leukemia (AML). Pulmonary infiltrates are usually microscopic and invariably associated with hyperleukocytosis. There are autopsy case reports of pulmonary leukemia as a cause of pulmonary infiltrates, even in non-hyperleukocytosis AML patients with low blast counts. Radiographically, patients present with an air-space disease with a diffuse interstitial reticular pattern in cases of hyperleukocytosis similar to cases of infectious pneumonia.
Pulmonary leukostasis syndrome involves the occlusion of small blood vessels in the lungs and typically occurs with a WBC count of greater than 100,000 per mL. The increased number of WBCs causes blood viscosity to rise due to the decreased deformability of the abnormal leukocytes, resulting in cell clumping and stasis in the microvasculature, leading to severe hypoxemic respiratory failure. Autopsy studies reveal extensive infiltration by leukemic cells in the pulmonary vasculature; pulmonary infarction with hemorrhage is also noted. [57]
Rarely, lung involvement by intravascular large B-cell lymphoma (IVLBCL) is noted on autopsy [58]. Early diagnosis is difficult as neither computed tomography nor 67-gallium scintigraphy can detect lung involvement. However, 18-fluro-deoxyglucose positron tomography (FDG-PET) may be a powerful tool for the early diagnosis of IVLBCL with pulmonary involvement [59].
3.4 Pulmonary Thromboembolism
Autopsy studies show that pulmonary thromboembolism (PTE) infrequently complicates the course of patients with acute leukemia and severe thrombocytopenia, and HSCT recipients with an incidence rate ranging from 1% to 6.3% [8]. [60] Patients with acute leukemias commonly have clinically silent haemostatic abnormalities, but some may show clinical manifestations, including venous thromboembolism, pulmonary embolism, disseminated intravascular coagulation, and life-threatening thrombohemorrhagic syndrome. The pathogenesis of PTE is complex and multifactorial and may involve tumor cell-derived procoagulant, fibrinolytic or proteolytic factors, and inflammatory cytokines, which affect clotting activation. Chemotherapy and anti-angiogenic drugs also increase the thrombotic risk in patients with lymphoma, acute leukemia, and multiple myeloma. Infectious complications are another important factor: endotoxins from gram-negative bacteria induce the release of tissue factor (TF), tumor necrosis factor (TNF), and interleukin-1 (IL-1), and gram-positive organisms can release bacterial mucopolysaccharides that directly activate factor XII. Needleman et al. reviewed 80 consecutive autopsies in leukemia patients and found three patients with previously undiagnosed PTE, all of whom had been severely thrombocytopenic. However, Candida forms were abundant in the thromboemboli in all three patients, with some containing septate hyphal forms consistent with Mucor or aspergillosis. No vessel wall invasion or necrosis was noted, and fungus was not shown to be present in pulmonary vessels in segments of the lung not involved with thromboembolism [60]. Leukemic patients may also be affected by other prothrombotic factors, including hyperleukocytosis, increased TF expression and activation, and the prothrombotic properties of therapeutic agents, such as all-trans retinoic acid and L-asparaginase, which can induce thrombosis involving multiple organs. A higher index of suspicion may lead to the diagnosis, but the signs and symptoms of PTE in patients with hematologic malignancy are variable and nonspecific as with PTE in other populations.
3.5 Bronchiolitis Obliterans with Organizing Pneumonia and Bronchiolitis Obliterans
The majority of patients with hematological malignancies who develop organizing pneumonia (BOOP) have been exposed to various chemotherapeutic agents, including cytarabine and anthracyclines as well as radiation therapy. [61, 62] In one autopsy series, Sharma et al. reported on 71 patients who had undergone HSCT, of whom 3% had BO and 1% had BOOP [8]. Unusual histological variants have also been described, including a case report of acute fibrinous and organizing pneumonia following HSCT in a patient with AML [63] characterized by prominent intraalveolar fibrin deposition and organizing pneumonia. The radiographic presentation revealed patchy consolidation in the lower lobes and a diffuse miliary pattern. Clinically, these cases can have subacute presentations similar to cryptogenic organizing pneumonia or have more rapid progression with clinical features similar to ARDS. BOOP and BO are rare autopsy findings, which may be because infections are being treated aggressively, and often patients not responding to antibiotics and with no clinical evidence of infections are given a trial of corticosteroids.
Yokoi et al. reported bronchiolitis obliterans (BO) on autopsy in 8 of 81 patients who underwent allogeneic BMT with AML or ALL. All patients received conditioning regimens with total body irradiation and cyclophosphamide with or without busulfan or cytosine arabinoside. Immunosuppressive therapies were administered to all patients after BMT, including methotrexate with or without cyclosporine. The onset of respiratory symptoms was 110–430 days after BMT, and the symptoms were non-productive cough, dyspnea, fever, chest pain, and pneumothorax. Seven patients died of progressive respiratory failure and one of relapsed leukemia. Coexistent infections included CMV, varicella zoster, Mycobacterium tuberculosis, and Aspergillus [ 21]. Paz et al. also described two patients who underwent autologous BMT for lymphoma and developed rapidly progressive respiratory insufficiency on post-transplant day 90 and 273. Despite aggressive immunosuppressive therapy, both patients died of respiratory failure. Autopsy studies revealed histological evidence of bronchiolitis obliterans [64].
3.6 Pulmonary Veno-occlusive Disease
Pulmonary veno-occlusive disease (PVOD) is a rare cause of pulmonary hypertension that is characterized histopathologically by intimal proliferation and fibrosis of the pulmonary venules and small veins leading to progressive vascular obstruction [65]. The etiology of PVOD remains unclear. It has been reported as an unusual complication of both myeloablative allogeneic, autologous and cord HSCT, suggesting that it might be regimen-related toxicity [65–70]. Surgical lung biopsy provides definitive diagnosis [71]. PVOD carries a poor prognosis, with most reported patients experiencing progressive disease and death within 2 years of diagnosis [72]. Autopsy findings reveal intimal fibrosis of most of the pulmonary veins, with no significant intraluminal thrombi or arterial changes [69]. Treatment recommendations are anecdotal. Steroids and heparin have been reported to possibly improve outcomes [66].
3.7 Pulmonary Alveolar Proteinosis
Autopsy studies in patients with hematologic malignancy (particularly with myelodysplastic syndrome) and following HSCT have revealed rare cases of secondary pulmonary alveolar proteinosis (PAP) characterized by intra-alveolar accumulation of surfactant components and cellular debris, with minimal interstitial inflammation or fibrosis [73–75]. Secondary PAP is frequently noted among patients with hematologic malignancies who develop fungal infection, especially pulmonary aspergillosis. KL-6 protein is produced by type II alveolar pneumocytes and can be helpful in establishing an early diagnosis of PAP [74, 76]. The standard therapy for PAP with hematological malignancy has not yet been firmly established. The administration of GM-CSF has been suggested to activate the alveolar macrophages and increase the rate of surfactant clearance [73]. Case reports indicate that the prognosis of PAP with leukemia is very poor because of the high frequency of superinfections in the affected alveoli [73, 75].
4 Discrepancies Between Clinical and Postmortem Autopsy Findings
Several autopsy series have reported diagnostic discrepancies between premortem clinical diagnosis and postmortem autopsy findings ranging from 5% to 64% in patients with hematologic malignancy and HSCT recipients (Table 20.2) [15, 77–83]. The Goldman criteria are commonly used to categorize discrepancies between clinical and pathological diagnoses or causes of death [84]. Class 1 discrepancies are defined as missed major diagnoses with potential adverse impact on survival and would have changed management. Class II discrepancies are missed major diagnoses with no potential impact on survival and that would have not changed therapy. Class III discrepancies are defined as missed minor diagnoses related to terminal disease, but not related to the cause of death, and Class IV are other missed minor diagnoses.
Gerain et al. reported a 59% major discrepancy rate in 34 cancer patients who were admitted to a medical oncological ICU over an 11-month period. [77] The majority of major discrepancies were due to complications of the cancer itself or its treatment (such as non-cardiogenic pulmonary edema, acute hemorrhage, and pulmonary embolism) rather than infection. Pastores et al. reported a major missed diagnosis rate of 26% in 86 autopsies performed on cancer patients who died in a medical-surgical ICU [78]. Of the 86 patients, 25 (40%) had undergone HSCT, 18 (29%) had either leukemias or lymphomas, 19 (31%) had solid tumors, and 24 (28%) were surgical cancer patients. Among the patients with discrepancies 54% had class I discrepancies, 32% had class II discrepancies, and 14% had both class I and class II discrepancies. Of the 22 discordant cases, 6 had hematological malignancies and 4 underwent HSCT. Opportunistic infections due to viral, fungal, bacterial, and parasitic organisms and cardiac complications were the most common class I discrepancies. The majority of Class II discrepancies were accounted for by cardiopulmonary complications due to pulmonary embolism and thrombotic endocarditis. The study was limited by the retrospective study design and selection bias that may have occurred as physicians and family members of patients with premortem diagnostic uncertainty would have been more likely to pursue an autopsy. Xavier et al. reported a class I discrepancy rate of 31.3% in 118 autopsies of patients with hematological malignancies or severe aplastic anemia [79]. The most common diagnoses causing these discrepancies were hematological disease, pneumonia, and gastrointestinal hemorrhage. Class I discrepancies were more common in elderly patients (>64 years) and in patients who had not received previous specific treatment for the hematological malignancy, had not been treated with bone marrow or peripheral blood HSCT, or had not been treated in a specialized hematology unit. Seftel et al. reported a discrepancy rate of 64% (34% major, 30% minor) in 48 autopsies of patients who underwent HSCT (blood and bone marrow) [82]. Infectious complications, including pulmonary aspergillosis, candidiasis, and infective endocarditis, accounted for the majority of the major discrepancies. Hoffmeister et al. found a 26% discrepancy rate (4% major, 23% minor) in 111 autopsies of patients who had undergone HSCT [83]. In contrast, Al Saidi et al. found a significant concordance between the clinical and postmortem diagnoses in 28 critically ill HSCT patients [15]. Ten (36%) of the twenty eight patients had discrepancies uncovered on autopsy; only two discrepancies would have influenced patient management, and none would have altered patient outcome. Most of the unexpected diagnoses were infections, and the rest included non-infective endocarditis, GVHD, and gastrointestinal and neurologic diagnoses. The authors concluded that clinical diagnosis alone might be appropriate for withdrawal of care decision-making in these patients.
5 Summary
Infectious and noninfectious pulmonary diseases are commonly found on postmortem autopsy studies in patients with hematological malignancy and HSCT recipients. Despite the technological advances in diagnostic testing and imaging modalities, obtaining an accurate clinical diagnosis remains difficult and is often not possible until autopsy. Major diagnostic discrepancies between clinical premortem diagnoses and postmortem autopsy findings have been reported in patients with hematologic malignancy. The most common missed diagnoses are due to opportunistic infections and cardiopulmonary complications. These findings underscore the importance of enhanced surveillance, monitoring, and treatment of infections and cardiopulmonary disorders in these patients. Autopsies remain important in determining an accurate cause of death and for improved understanding of diagnostic deficiencies, as well as for medical education and quality assurance.
References
Yen K, Lee A, Krowka M, Burger C (2004) Pulmonary complications in bone marrow transplantation: a practical approach to diagnosis and treatment. Clin Chest Med 25:189–201
Huaringa AJ, Leyva FJ, Giralt SA et al (2000) Outcome of bone marrow transplantation patients requiring mechanical ventilation. Crit Care Med 28:1014–1017
Soubani A, Kseibi E, Bander J et al (2004) Outcome and prognostic factors of hematopoietic stem cell transplantation recipients admitted to a medical ICU. Chest 126: 1604–1611
Pene F, Aubron C, Azoulay E et al (2006) Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol 24:643–649
Bach PB, Schrag D, Nierman DM et al (2001) Identification of poor prognostic features among patients requiring mechanical ventilation after hematopoietic stem cell transplantation. Blood 98:3234–3240
Jules-Elysee K, Stover DE, Yahalom J et al (1992) Pulmonary complications in lymphoma patients treated with high-dose therapy autologous bone marrow transplantation. Am Rev Respir Dis 146:485–491
Roychowdhury M, Pambuccian SE, Aslan DL et al (2005) Pulmonary complications after bone marrow transplantation: an autopsy study from a large transplantation center. Arch Pathol Lab Med 129:366–371
Sharma S, Nadrous H, Peters S et al (2005) Pulmonary complications in adult blood and marrow transplant recipients: autopsy findings. Chest 128:1385–1392
Kefford RF, Cooney NJ, Woods RL et al (1981) Causes of deaths in an oncology unit. Eur J Cancer Clin Oncol 17: 1117–1124
Marwick C (1995) Pathologists request autopsy revival. JAMA 273:1889, 1891
Donhuijsen K, Petersen P, Schmid W (2008) Trend reversal in the frequency of mycoses in hematological neoplasias: autopsy results from 1976 to 2005. Deutsches Ärzteblatt Int 105:501–506
Chamilos G, Luna M, Lewis R et al (2006) Invasive fungal infections in patients with hematologic malignancies in a tertiary care cancer center: an autopsy study over a 15-year period (1989–2003). Haematologica 91: 986–989
Marr K, Carter R, Crippa F et al (2002) Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 34:909–917
Barth PJ, Rossberg C, Koch S, Ramaswamy A (2000) Pulmonary aspergillosis in an unselected autopsy series. Pathol Res Pract 196:73–80
Al-Saidi F, Diaz-Granados N, Messner H et al (2002) Relationship between premortem and postmortem diagnosis in critically ill bone marrow transplantation patients. Crit Care Med 30:570–573
Bodey G, Bueltmann B, Duguid W et al (1992) Fungal infections in cancer patients: an international autopsy survey. Eur J Clin Microbiol Infect Dis 11:99–109
Chandrasekar PH, Weinmann A, Shearer C (1995) Autopsy-identified infections among bone marrow transplant recipients: a clinico-pathologic study of 56 patients. Bone Marrow Transplantation Team. Bone Marrow Transplant 16: 675–681
Groll AH, Shah PM, Mentzel C et al (1996) Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J Infect 33:23–32
Hachem R, Sumoza D, Hanna H et al (2006) Clinical and radiologic predictors of invasive pulmonary aspergillosis in cancer patients: should the European Organization for Research and Treatment of Cancer/Mycosis Study Group (EORTC/MSG) criteria be revised? Cancer 106:1581–1586
Subir M, Martino R, Rovira M et al (2003) Clinical applicability of the new EORTC/MSG classification for invasive pulmonary aspergillosis in patients with hematological malignancies and autopsy-confirmed invasive aspergillosis. Ann Hematol 82:80–82
Yokoi T, Hirabayashi N, Ito M et al (1997) Broncho-bronchiolitis obliterans as a complication of bone marrow transplantation: a clinicopathological study of eight autopsy cases. Nagoya BMT Group. Virchows Arch 431:275–282
Herbrecht R, Denning D, Patterson T et al (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347:408–415
Pagano L, Fianchi L, Mele L et al (2002) Pneumocystis carinii pneumonia in patients with malignant haematological diseases: 10 years’ experience of infection in GIMEMA centres. Br J Haematol 117:379–386
Buxhofer V, Ruckser R, Kier P et al (2001) Successful treatment of invasive mould infection affecting lung and brain in an adult suffering from acute leukaemia. Eur J Haematol 67:128–132
Kami M, Machida U, Okuzumi K et al (2002) Effect of fluconazole prophylaxis on fungal blood cultures: an autopsy-based study involving 720 patients with haematological malignancy. Br J Haematol 117:40–46
Barron MA, Sutton DA, Veve R et al (2003) Invasive mycotic infections caused by Chaetomium perlucidum, a new agent of cerebral phaeohyphomycosis. J Clin Microbiol 41: 5302–5307
Bethge WA, Schmalzing M, Stuhler G et al (2005) Mucormycoses in patients with hematologic malignancies: an emerging fungal infection. Haematologica 90(Suppl): ECR22
Koyanagi T, Nishida N, Osabe S et al (2006) Autopsy case of disseminated Trichosporon inkin infection identified with molecular biological and biochemical methods. Pathol Int 56:738–743
Lagrou K, Massonet C, Theunissen K et al (2005) Fatal pulmonary infection in a leukaemic patient caused by Hormographiella aspergillata. J Med Microbiol 54: 685–688
Nosari A, Oreste P, Montillo M et al (2000) Mucormycosis in hematologic malignancies: an emerging fungal infection. Haematologica 85:1068–1071
Salonen JH (2006) Successful management of cerebral and pulmonary mucormycosis with liposomal amphotericin B in a 28-year-old woman with acute lymphoblastic leukemia. Acta Biomed 77(Suppl 2):28–31
Rüping MJGT, Vehreschild J, Cornely O (2008) Patients at high risk of invasive fungal infections: when and how to treat. Drugs 68:1941–1962
Ewig S, Torres A, Riquelme R et al (1998) Pulmonary complications in patients with haematological malignancies treated at a respiratory ICU. Eur Respir J 12:116–122
Inai K, Iwasaki H, Noriki S et al (2007) Frequent detection of multidrug-resistant pneumonia-causing bacteria in the pneumonia lung tissues of patients with hematological malignancies. Int J Hematol 86:225–232
Rousseau A, Morcos M, Amrouche L et al (2004) Lethal pulmonary hemorrhage caused by a fulminant Stenotrophomonas maltophilia respiratory infection in an acute myeloid leukemia patient. Leuk Lymphoma 45: 1293–1296
Torres HA, Aguilera E, Safdar A et al (2008) Fatal cytomegalovirus pneumonia in patients with haematological malignancies: an autopsy-based case-control study. Clin Microbiol Infect 14:1160–1166
Zaman SS, Seykora JT, Hodinka RL et al (1996) Cytologic manifestations of respiratory syncytial virus pneumonia in bronchoalveolar lavage fluid: a case report. Acta Cytol 40: 546–551
Mori S, Maruyama H, Ito I et al (1998) Diagnosis of measles viral pneumonia in a patient with Hodgkin’s disease by reverse transcription-polymerase chain reaction of serum. Int J Hematol 68:327–331
Duband S, Cornillon J, Tavernier E et al (2008) Toxoplasmosis with hemophagocytic syndrome after bone marrow transplantation: diagnosis at autopsy. Transpl Infect Dis 10: 372–374
Specks U (2001) Diffuse alveolar hemorrhage syndromes. Curr Opin Rheumatol 13:12–17
Afessa B, Tefferi A, Litzow M et al (2002) Diffuse alveolar hemorrhage in hematopoietic stem cell transplant recipients. Am J Respir Crit Care Med 166:641–645
Lewis ID, DeFor T, Weisdorf DJ (2000) Increasing incidence of diffuse alveolar hemorrhage following allogeneic bone marrow transplantation: cryptic etiology and uncertain therapy. Bone Marrow Transplant 26:539–543
Weisdorf DJ (2003) Diffuse alveolar hemorrhage: an evolving problem? Leukemia 17:1049–1050
Smith LJ, Katzenstein AL (1982) Pathogenesis of massive pulmonary hemorrhage in acute leukemia. Arch Intern Med 142:2149–2152
Grigoriyan A, Rishi A, Molina J et al (2007) Diffuse alveolar damage and hemorrhage in acute myelogenous leukemia treated with corticosteroids. Conn Med 71: 201–204
Jiang Q, Yang S-M, Jiang B et al (2007) Diffuse alveolar hemorrhage as a complication in patients with hematologic malignancies after chemotherapy: report of two cases and literature review. Zhonghua Xue Ye Xue Za Zhi 28: 230–234
Uchiyama M, Ikeda T (2010). Diffuse alveolar hemorrhage after unrelated cord blood transplantation. Bone Marrow Transplant 45(4):789-90. Epub 2009 Aug 31
Nuckols JD (1999) Autopsy findings in umbilical cord blood transplant recipients. Am J Clin Pathol 112:335–342
Wojno KJ, Vogelsang GB, Beschorner WE et al (1994) Pulmonary hemorrhage as a cause of death in allogeneic bone marrow recipients with severe acute graft-versus-host disease. Transplantation 57:88–92
Delclaux C, Azoulay E (2003) Inflammatory response to infectious pulmonary injury. Eur Respir J Suppl 42:10s–14s
Agust C, Ramirez J, Picado C et al (1995) Diffuse alveolar hemorrhage in allogeneic bone marrow transplantation. A postmortem study. Am J Respir Crit Care Med 151: 1006–1010
Chao NJ, Duncan SR, Long GD et al (1991) Corticosteroid therapy for diffuse alveolar hemorrhage in autologous bone marrow transplant recipients. Ann Intern Med 114: 145–146
Metcalf JP, Rennard SI, Reed EC et al (1994) Corticosteroids as adjunctive therapy for diffuse alveolar hemorrhage associated with bone marrow transplantation. University of Nebraska Medical Center Bone Marrow Transplant Group. Am J Med 96:327–334
Pastores S, Papadopoulos E, Voigt L et al (2003) Diffuse alveolar hemorrhage after allogeneic hematopoietic stem-cell transplantation: treatment with recombinant factor VIIa. Chest 124:2400–2403
Wanko S, Broadwater G, Folz R et al (2006) Diffuse alveolar hemorrhage: retrospective review of clinical outcome in allogeneic transplant recipients treated with aminocaproic acid. Biol Blood Marrow Transplant 12: 949–953
Costa MBG, Siqueira SAC, Saldiva PHN et al (2004) Histologic patterns of lung infiltration of B-cell, T-cell, and Hodgkin lymphomas. Am J Clin Pathol 121:718–726
Kaminsky DA, Hurwitz CG, Olmstead JI (2000) Pulmonary leukostasis mimicking pulmonary embolism. Leuk Res 24:175–178
Murase T, Yamaguchi M, Suzuki R et al (2007) Intravascular large B-cell lymphoma (IVLBCL): a clinicopathologic study of 96 cases with special reference to the immunophenotypic heterogeneity of CD5. Blood 109:478–485
Kitanaka A, Kubota Y, Imataki O et al (2009) Intravascular large B-cell lymphoma with FDG accumulation in the lung lacking CT/(67)gallium scintigraphy abnormality. Hematol Oncol 27:46–49
Needleman SW, Stein MN, Hoak JC (1981) Pulmonary embolism in patients with acute leukemia and severe thrombocytopenia. Western J Med 135:9–13
Daniels C, Myers J, Utz J et al (2007) Organizing pneumonia in patients with hematologic malignancies: a steroid-responsive lesion. Respir Med 101:162–168
Mokhtari M, Bach PB, Tietjen PA et al (2002) Bronchiolitis obliterans organizing pneumonia in cancer: a case series. Respir Med 96:280–286
Lee S, Park J-J, Sung S et al (2009) Acute fibrinous and organizing pneumonia following hematopoietic stem cell transplantation. Korean J Intern Med 24:156–159
Paz HL, Crilley P, Patchefsky A et al (1992) Bronchiolitis obliterans after autologous bone marrow transplantation. Chest 101:775–778
Gutman JA, Allen CT, Madtes DK et al (2008) Pulmonary veno-occlusive disease following reduced-intensity cord blood transplantation. Bone Marrow Transplant 42: 559–561
Hackman RC, Madtes DK, Petersen FB et al (1989) Pulmonary venoocclusive disease following bone marrow transplantation. Transplantation 47:989–992
Kuga T, Kohda K, Hirayama Y et al (1996) Pulmonary veno-occlusive disease accompanied by microangiopathic hemolytic anemia 1 year after a second bone marrow transplantation for acute lymphoblastic leukemia. Int J Hematol 64: 143–150
Mukai M, Kondo M, Bohgaki T et al (2003) Pulmonary veno-occlusive disease following allogeneic peripheral blood stem cell transplantation for chronic myeloid leukaemia. Br J Haematol 123:1
Troussard X, Bernaudin JF, Cordonnier C et al (1984) Pulmonary veno-occlusive disease after bone marrow transplantation. Thorax 39:956–957
Williams LM, Fussell S, Veith RW et al (1996) Pulmonary veno-occlusive disease in an adult following bone marrow transplantation. Case report and review of the literature. Chest 109:1388–1391
Mandel J, Mark EJ, Hales CA (2000) Pulmonary veno-occlusive disease. Am J Respir Crit Care Med 162: 1964–1973
Bunte MC, Patnaik MM, Pritzker MR et al (2008) Pulmonary veno-occlusive disease following hematopoietic stem cell transplantation: a rare model of endothelial dysfunction. Bone Marrow Transplant 41:677–686
Cordonnier C, Fleury-Feith J, Escudier E et al (1994) Secondary alveolar proteinosis is a reversible cause of respiratory failure in leukemic patients. Am J Respir Crit Care Med 149:788–794
Kajiume T, Yoshimi S, Nagita A et al (1999) A case of myelodysplastic syndrome complicated by pulmonary alveolar proteinosis with a high serum KL-6 level. Pediatr Hematol Oncol 16:367–371
Watanabe K, Sueishi K, Tanaka K et al (1990) Pulmonary alveolar proteinosis and disseminated atypical mycobacteriosis in a patient with busulfan lung. Acta Pathol Jpn 40: 63–66
Kohno N, Inoue Y, Hamada H et al (1994) Difference in sero-diagnostic values among KL-6-associated mucins classified as cluster 9. Int J Cancer Suppl 8:81–83
Gerain J, Sculier JP, Malengreaux A et al (1990) Causes of deaths in an oncologic intensive care unit: a clinical and pathological study of 34 autopsies. Eur J Cancer 26: 377–381
Pastores SM, Dulu A, Voigt L et al (2007) Premortem clinical diagnoses and postmortem autopsy findings: discrepancies in critically ill cancer patients. Crit Care 11:R48
Xavier AC, Siqueira SA, Costa LJ et al (2005) Missed diagnosis in hematological patients – an autopsy study. Virchows Arch 446:225–231
Burton EC, Troxclair DA, Newman W III et al (1998) Autopsy diagnoses of malignant neoplasms. How often are clinical diagnoses incorrect? JAMA 280:1245–1248
Provencio M, Espana P, Salas C et al (2000) Hodgkin’s disease: correlation between causes of death at autopsy and clinical diagnosis. Ann Oncol 11:59–64
Seftel MD, Ho M, Pruthi D et al (2007) High rate of discordance between clinical and autopsy diagnoses in blood and marrow transplantation. Bone Marrow Transplant 40: 1049–1053
Hofmeister CC, Marinier DE, Czerlanis C et al (2007) Clinical utility of autopsy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 13: 26–30
Goldman L, Sayson R, Robbins S et al (1983) The value of the autopsy in three medical eras. N Engl J Med 308: 1000–1005
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Pastores, S.M., Dulu, A.O., DeSouza, S.A. (2011). What Has Been Learned from Postmortem Studies?. In: Azoulay, E. (eds) Pulmonary Involvement in Patients with Hematological Malignancies. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-15742-4_20
Download citation
DOI: https://doi.org/10.1007/978-3-642-15742-4_20
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-15741-7
Online ISBN: 978-3-642-15742-4
eBook Packages: MedicineMedicine (R0)