Abstract
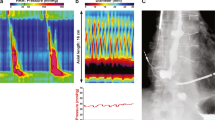
Functional lumen imaging probe (FLIP) is a device that measures luminal parameters in the esophagus including cross-sectional area, pressure, diameter, and distensibility index using impedance planimetry. FLIP may also help identify anterograde and retrograde contractile activity in the esophageal body analyzed by the FLIP 2.0 system. This relatively new technology brings additional information to the more conventional esophagram and high-resolution impedance manometry. Despite accumulating data on the clinical utility of FLIP, current quality of available evidence is low.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Carlson DA, Kahrilas PJ, Lin Z, et al. Evaluation of esophageal motility utilizing the functional lumen imaging probe. Am J Gastroenterol. 2016;111:1726–35.
Bianca A, Schindler V, Schnurre L, et al. Endoscope presence during endoluminal functional lumen imaging probe (FLIP) influences FLIP metrics in the evaluation of esophageal dysmotility. Neurogastroenterol Motil. 2020;32:e13823.
Kwiatek MA, Hirano I, Kahrilas PJ, et al. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology. 2011;140:82–90.
Hirano I, Pandolfino JE, Boeckxstaens GE. Functional lumen imaging probe for the Management of Esophageal Disorders: expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15:325–34.
Carlson DA, Kou W, Lin Z, et al. Normal values of esophageal Distensibility and distension-induced contractility measured by functional luminal imaging probe Panometry. Clin Gastroenterol Hepatol. 2019;17:674–681.e1, 674.
Rohof WO, Hirsch DP, Kessing BF, et al. Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology. 2012;143:328–35.
Kwiatek MA, Kahrilas K, Soper NJ, et al. Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg. 2010;14:268–76.
Tucker E, Sweis R, Anggiansah A, et al. Measurement of esophago-gastric junction cross-sectional area and distensibility by an endolumenal functional lumen imaging probe for the diagnosis of gastro-esophageal reflux disease. Neurogastroenterol Motil. 2013;25:904–10.
Rieder E, Swanstrom LL, Perretta S, et al. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc. 2013;27:400–5.
Pandolfino JE, de Ruigh A, Nicodeme F, et al. Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil. 2013;25:496–501.
Rooney KP, Baumann AJ, Donnan E, et al. Esophagogastric junction opening parameters are consistently abnormal in untreated achalasia. Clin Gastroenterol Hepatol. 2021;19:1058–1060.e1, 1058.
Savarino E, di Pietro M, Bredenoord AJ, et al. Use of the functional lumen imaging probe in clinical Esophagology. Am J Gastroenterol. 2020;115:1786–96.
Benitez AJ, Budhu S, Burger C, et al. Use of the functional luminal imaging probe in pediatrics: a comparison study of patients with achalasia before and after endoscopic dilation and non-achalasia controls. Neurogastroenterol Motil. 2021;33:e14133.
Courbette O, Deslandres C, Drouin E, et al. Functional luminal imaging probe (FLIP) in the management of pediatric esophageal disorders. J Pediatr Gastroenterol Nutr. 2021;74:516.
Holmstrom AL, Campagna RAJ, Alhalel J, et al. Intraoperative FLIP distensibility during POEM varies according to achalasia subtype. Surg Endosc. 2021;35:3097–103.
Jain AS, Carlson DA, Triggs J, et al. Esophagogastric junction Distensibility on functional lumen imaging probe topography predicts treatment response in achalasia-anatomy matters! Am J Gastroenterol. 2019;114:1455–63.
Wu PI, Szczesniak MM, Craig PI, et al. Novel intra-procedural Distensibility measurement accurately predicts immediate outcome of pneumatic dilatation for idiopathic achalasia. Am J Gastroenterol. 2018;113:205–12.
Holmstrom AL, Campagna RAJ, Cirera A, et al. Intraoperative use of FLIP is associated with clinical success following POEM for achalasia. Surg Endosc. 2021;35:3090–6.
Goong HJ, Hong SJ, Kim SH. Intraoperative use of a functional lumen imaging probe during peroral endoscopic myotomy in patients with achalasia: a single-institute experience and systematic review. PLoS One. 2020;15:e0234295.
Holmstrom AL, Campagna RJ, Carlson DA, et al. Comparison of preoperative, intraoperative, and follow-up functional luminal imaging probe measurements in patients undergoing myotomy for achalasia. Gastrointest Endosc. 2021;94:509.
Kethman WC, Thorson CM, Sinclair TJ, et al. Initial experience with peroral endoscopic myotomy for treatment of achalasia in children. J Pediatr Surg. 2018;53:1532–6.
Su B, Callahan ZM, Novak S, et al. Using impedance Planimetry (EndoFLIP) to evaluate Myotomy and predict outcomes after surgery for achalasia. J Gastrointest Surg. 2020;24:964–71.
Teitelbaum EN, Soper NJ, Pandolfino JE, et al. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc. 2015;29:522–8.
Reddy AT, Shimpi RA, Parish A, et al. Predictors of abnormal functional luminal impedance Planimetry findings in nonmechanical Esophagogastric junction outflow obstruction. Dig Dis Sci. 2020;66:3968.
Verlaan T, Rohof WO, Bredenoord AJ, et al. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc. 2013;78(1):39–44. https://doi.org/10.1016/j.gie.2013.01.006. Epub 2013 Feb 26.
Triggs JR, Carlson DA, Beveridge C, et al. Functional luminal imaging probe Panometry identifies achalasia-type Esophagogastric junction outflow obstruction. Clin Gastroenterol Hepatol. 2020;18:2209–17.
Murray FR, Fischbach LM, Schindler V, et al. Solid swallow examination during high resolution manometry and EGJ-distensibility help identify esophageal outflow obstruction in non-obstructive dysphagia. Dysphagia. 2022;37(1):168–76.
Yoo IK, Choi SA, Kim WH, et al. Assessment of clinical outcomes after peroral endoscopic myotomy via esophageal distensibility measurements with the endoluminal functional lumen imaging probe. Gut Liver. 2019;13(1):32–9. https://doi.org/10.5009/gnl18233. PMID: 30400727.
Pandolfino JE, Shi G, Curry J, et al. Esophagogastric junction distensibility: a factor contributing to sphincter incompetence. Am J Physiol Gastrointest Liver Physiol. 2002;282:G1052–8.
Ghosh SK, Kahrilas PJ, Brasseur JG. Liquid in the gastroesophageal segment promotes reflux, but compliance does not: a mathematical modeling study. Am J Physiol Gastrointest Liver Physiol. 2008;295:G920–33.
DeHaan RK, Davila D, Frelich MJ, et al. Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc. 2017;31:193–8.
Ilczyszyn A, Botha AJ. Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus. 2014;27:637–44.
Turner B, Helm M, Hetzel E, et al. Is that ‘floppy’ fundoplication tight enough? Surg Endosc. 2020;34:1823–8.
Su B, Novak S, Callahan ZM, et al. Using impedance planimetry (EndoFLIP) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc. 2020;34:1761–8.
Smeets FG, Keszthelyi D, Bouvy ND, et al. Does measurement of Esophagogastric junction Distensibility by EndoFLIP predict therapy- responsiveness to Endoluminal fundoplication in patients with gastroesophageal reflux disease? J Neurogastroenterol Motil. 2015;21:255–64.
Samo S, Mulki R, Godiers ML, et al. Utilizing functional lumen imaging probe in directing treatment for post-fundoplication dysphagia. Surg Endosc. 2020;35:4418.
Rosen R, Garza JM, Nurko S. Functional luminal imaging probe assessment in Postfundoplication patients changes management beyond manometry. J Pediatr Gastroenterol Nutr. 2020;70:e119–23.
Kwiatek MA, Pandolfino JE, Hirano I, et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010;72:272–8.
Carlson DA, Kathpalia P, Craft J, et al. The relationship between esophageal acid exposure and the esophageal response to volumetric distention. Neurogastroenterol Motil. 2018;30:e13240.
Nicodeme F, Hirano I, Chen J, et al. Esophageal distensibility as a measure of disease severity in patients with eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2013;11:1101–1107.e1, 1101.
Menard-Katcher C, Benitez AJ, Pan Z, et al. Influence of age and eosinophilic esophagitis on esophageal Distensibility in a pediatric cohort. Am J Gastroenterol. 2017;112:1466–73.
Hassan M, Aceves S, Dohil R, et al. Esophageal compliance quantifies epithelial remodeling in pediatric patients with eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2019;68:559–65.
Ng K, Mogul D, Hollier J, et al. Utility of functional lumen imaging probe in esophageal measurements and dilations: a single pediatric center experience. Surg Endosc. 2020;34:1294–9.
Carlson DA, Gyawali CP, Kahrilas PJ, et al. Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc. 2019;90:915–923.e1, 915.
Carlson DA, Kou W, Pandolfino JE. The rhythm and rate of distension-induced esophageal contractility: a physiomarker of esophageal function. Neurogastroenterol Motil. 2020;32:e13794.
Baumann AJ, Donnan EN, Triggs JR, et al. Normal functional luminal imaging probe Panometry findings associate with lack of major esophageal motility disorder on high-resolution manometry. Clin Gastroenterol Hepatol. 2021;19:259–268.e1, 259.
Carlson DA, Kou W, Rooney KP, et al. Achalasia subtypes can be identified with functional luminal imaging probe (FLIP) panometry using a supervised machine learning process. Neurogastroenterol Motil. 2021;33:e13932.
Jagtap N, Kalapala R, Reddy DN. Assessment of pyloric sphincter physiology using functional luminal imaging probe in healthy volunteers. J Neurogastroenterol Motil. 2020;26:391–6.
Malik Z, Sankineni A, Parkman HP. Assessing pyloric sphincter pathophysiology using EndoFLIP in patients with gastroparesis. Neurogastroenterol Motil. 2015;27:524–31.
Snape WJ, Lin MS, Agarwal N, et al. Evaluation of the pylorus with concurrent intraluminal pressure and EndoFLIP in patients with nausea and vomiting. Neurogastroenterol Motil. 2016;28:758–64.
Gourcerol G, Tissier F, Melchior C, et al. Impaired fasting pyloric compliance in gastroparesis and the therapeutic response to pyloric dilatation. Aliment Pharmacol Ther. 2015;41:360–7.
Ata-Lawenko RM, Lee YY. Emerging roles of the Endolumenal functional lumen imaging probe in gastrointestinal motility disorders. J Neurogastroenterol Motil. 2017;23:164–70.
Jacques J, Pagnon L, Hure F, et al. Peroral endoscopic pyloromyotomy is efficacious and safe for refractory gastroparesis: prospective trial with assessment of pyloric function. Endoscopy. 2019;51:40–9.
Jehangir A, Malik Z, Petrov RV, et al. EndoFLIP and pyloric dilation for gastroparesis symptoms refractory to Pyloromyotomy/Pyloroplasty. Dig Dis Sci. 2020;66:2682.
Zifan A, Mittal RK, Kunkel DC, et al. Loop analysis of the anal sphincter complex in fecal incontinent patients using functional luminal imaging probe. Am J Physiol Gastrointest Liver Physiol. 2020;318:G66–76.
Fynne L, Luft F, Gregersen H, et al. Distensibility of the anal canal in patients with systemic sclerosis: a study with the functional lumen imaging probe. Color Dis. 2013;15:e40–7.
Haas S, Liao D, Gregersen H, et al. Increased yield pressure in the anal canal during sacral nerve stimulation: a pilot study with the functional lumen imaging probe. Neurogastroenterol Motil. 2017;29
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Courbette, O., Faure, C. (2022). Functional Lumen Imaging Probe. In: Faure, C., Thapar, N., Di Lorenzo, C. (eds) Pediatric Neurogastroenterology. Springer, Cham. https://doi.org/10.1007/978-3-031-15229-0_14
Download citation
DOI: https://doi.org/10.1007/978-3-031-15229-0_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-15228-3
Online ISBN: 978-3-031-15229-0
eBook Packages: MedicineMedicine (R0)