Abstract
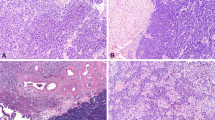
Primary neuroendocrine tumors of the urinary bladder are relatively rare and are comprised of a heterogeneous group of neoplasms. These include well-differentiated neuroendocrine tumors (WDNETs) or carcinoid tumors; poorly differentiated neuroendocrine carcinomas (NEC), including small cell neuroendocrine carcinoma (SCNEC) and large cell neuroendocrine carcinoma (LCNEC); and paraganglioma. These tumors are believed to arise from native neuroendocrine cells in the urothelial lining in the case of WDNETs, transdifferentiation of urothelial carcinoma cells in the case of poorly differentiated NECs, and chromaffin cells in autonomic ganglia in the case of paraganglioma. These tumors have different treatment protocols and clinical outcomes than conventional urothelial carcinoma, with SCNEC and LCNEC having a more aggressive course and worse outcomes and WDNET and paraganglioma having a more indolent course and better outcomes. Therefore, the proper recognition of these tumors is important. The epidemiological data; clinical information; histopathologic, immunohistochemical, and molecular features; prognostic factors; and therapeutic approaches of these entities are discussed in this chapter.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO classification of tumours of the urinary system and male genital organs-part a: renal, penile, and testicular tumours. Eur Urol. 2016;70(1):93–105. https://doi.org/10.1016/j.eururo.2016.02.029.
Kouba E, Cheng L. Neuroendocrine tumors of the urinary bladder according to the 2016 World Health Organization classification: molecular and clinical characteristics. Endocr Pathol. 2016;27(3):188–99. https://doi.org/10.1007/s12022-016-9444-5.
Purnell S, Sidana A, Maruf M, Grant C, Agarwal PK. Genitourinary paraganglioma: demographic, pathologic, and clinical characteristics in the surveillance, epidemiology, and end results database (2000–2012). Urol Oncol. 2017;35(7):457.e9–457.e14. https://doi.org/10.1016/j.urolonc.2017.02.006.
Posfai B, Kuthi L, Varga L, et al. The colorful palette of neuroendocrine neoplasms in the genitourinary tract. Anticancer Res. 2018;38(6):3243–54. https://doi.org/10.21873/anticancers.12589.
Chen Y, Epstein JI. Primary carcinoid tumors of the urinary bladder and prostatic urethra: a clinicopathologic study of 6 cases. Am J Surg Pathol. 2011;35(3):442–6. https://doi.org/10.1097/PAS.0b013e318208f96a.
Mascolo M, Altieri V, Mignogna C, Napodano G, De Rosa G, Insabato L. Calcitonin-producing well-differentiated neuroendocrine carcinoma (carcinoid tumor) of the urinary bladder: case report. BMC Cancer. 2005;5:88. https://doi.org/10.1186/1471-2407-5-88.
Hemal AK, Singh I, Pawar R, Kumar M, Taneja P. Primary malignant bladder carcinoid— a diagnostic and management dilemma. Urology. 2000;55(6):949. https://doi.org/10.1016/S0090-4295(00)00470-2.
Sugihara A, Kajio K, Yoshimoto T, et al. Primary carcinoid tumor of the urinary bladder. Int Urol Nephrol. 2002;33(1):53–7. https://doi.org/10.1023/a:1014400818905.
Baydar DE, Tasar C. Carcinoid tumor in the urinary bladder: unreported features. Am J Surg Pathol. 2011;35(11):1754–7. https://doi.org/10.1097/PAS.0b013e31823455eb.
Zozumi M, Nakai M, Matsuda I, et al. Primary carcinoid tumor of the urinary bladder with prominent subnuclear eosinophilic granules. Pathol Res Pract. 2012;208(2):109–12. https://doi.org/10.1016/j.prp.2011.10.008.
Erdem GU, Özdemir NY, Demirci NS, Şahin S, Bozkaya Y, Zengin N. Small cell carcinoma of the urinary bladder: changing trends in the current literature. Curr Med Res Opin. 2016;32(6):1013–21. https://doi.org/10.1185/03007995.2016.1155982.
Sroussi M, Elaidi R, Fléchon A, et al. Neuroendocrine carcinoma of the urinary bladder: a large, Retrospective Study From the French Genito-Urinary Tumor Group. Clin Genitourin Cancer. Published online December 5, 2019. https://doi.org/10.1016/j.clgc.2019.11.014.
Sacco E, Pinto F, Sasso F, et al. Paraneoplastic syndromes in patients with urological malignancies. Urol Int. 2009;83(1):1–11. https://doi.org/10.1159/000224860.
Schneider NI, Zigeuner R, Langner C. Small cell carcinoma of the urinary bladder: a rare tumor with propensity for hepatic involvement. Am J Med Sci. 2013;345(2):155–7. https://doi.org/10.1097/MAJ.0b013e3182648759.
Perán Teruel M, Giménez Bachs JM, Martínez Ruiz J, et al. Neuroendocrine carcinoma of the urinary bladder. 15-year retrospective analysis. Arch Esp Urol. 2012;65(2):237–43.
Wang G, Xiao L, Zhang M, et al. Small cell carcinoma of the urinary bladder: a clinicopathologic and immunohistochemical analysis of 81 cases. Hum Pathol. 2018;79:57–65. https://doi.org/10.1016/j.humpath.2018.05.005.
Cheng L, Pan C-X, Yang XJ, et al. Small cell carcinoma of the urinary bladder: a clinicopathologic analysis of 64 patients. Cancer. 2004;101(5):957–62. https://doi.org/10.1002/cncr.20456.
Choong NWW, Quevedo JF, Kaur JS. Small cell carcinoma of the urinary bladder. The Mayo Clinic experience. Cancer. 2005;103(6):1172–8. https://doi.org/10.1002/cncr.20903.
Fine SW. Neuroendocrine lesions of the genitourinary tract. Adv Anat Pathol. 2007;14(4):286–96. https://doi.org/10.1097/PAP.0b013e3180ca8a89.
Smith J, Reidy-Lagunes D. The management of extrapulmonary poorly differentiated (high-grade) neuroendocrine carcinomas. Semin Oncol. 2013;40(1):100–8. https://doi.org/10.1053/j.seminoncol.2012.11.011.
Thompson S, Cioffi-Lavina M, Chapman-Fredricks J, Gomez-Fernandez C, Fernandez-Castro G, Jorda M. Distinction of high-grade neuroendocrine carcinoma/small cell carcinoma from conventional urothelial carcinoma of urinary bladder: an immunohistochemical approach. Appl Immunohistochem Mol Morphol. 2011;19(5):395–9. https://doi.org/10.1097/PAI.0b013e31820eca9a.
Pant-Purohit M, Lopez-Beltran A, Montironi R, MacLennan GT, Cheng L. Small cell carcinoma of the urinary bladder. Histol Histopathol. 2010;25(2):217–21. https://doi.org/10.14670/HH-25.217.
Vetterlein MW, Wankowicz SAM, Seisen T, et al. Neoadjuvant chemotherapy prior to radical cystectomy for muscle-invasive bladder cancer with variant histology. Cancer. 2017;123(22):4346–55. https://doi.org/10.1002/cncr.30907.
Niu Q, Lu Y, Xu S, et al. Clinicopathological characteristics and survival outcomes of bladder neuroendocrine carcinomas: a population-based study. Cancer Manag Res. 2018;10:4479–89. https://doi.org/10.2147/CMAR.S175286.
Kanagarajah P, Ayyathurai R, Saleem U, Manoharan M. Small cell carcinoma arising from the bulbar urethra: a case report and literature review. Urol Int. 2012;88(4):477–9. https://doi.org/10.1159/000332154.
Acosta AM, Kajdacsy-Balla A. Primary neuroendocrine tumors of the ureter: a short review. Arch Pathol Lab Med. 2016;140(7):714–7. https://doi.org/10.5858/arpa.2015-0106-RS.
Kim TS, Seong DH, Ro JY. Small cell carcinoma of the ureter with squamous cell and transitional cell carcinomatous components associated with ureteral stone. J Korean Med Sci. 2001;16(6):796–800. https://doi.org/10.3346/jkms.2001.16.6.796.
Pompas-Veganzones N, Gonzalez-Peramato P, Sanchez-Carbayo M. The neuroendocrine component in bladder tumors. Curr Med Chem. 2014;21(9):1117–28.
Ploeg M, Aben KK, Hulsbergen-van de Kaa CA, Schoenberg MP, Witjes JA, Kiemeney LA. Clinical epidemiology of nonurothelial bladder cancer: analysis of the Netherlands Cancer registry. J Urol. 2010;183(3):915–20. https://doi.org/10.1016/j.juro.2009.11.018.
Grignon DJ, Ro JY, Ayala AG, et al. Small cell carcinoma of the urinary bladder. A clinicopathologic analysis of 22 cases. Cancer. 1992;69(2):527–36.
Abrahams NA, Moran C, Reyes AO, Siefker-Radtke A, Ayala AG. Small cell carcinoma of the bladder: a contemporary clinicopathological study of 51 cases. Histopathology. 2005;46(1):57–63. https://doi.org/10.1111/j.1365-2559.2004.01980.x.
Terracciano L, Richter J, Tornillo L, et al. Chromosomal imbalances in small cell carcinomas of the urinary bladder. J Pathol. 1999;189(2):230–5. https://doi.org/10.1002/(SICI)1096-9896(199910)189:2<230::AID-PATH407>3.0.CO;2-8.
Cheng L, Jones TD, McCarthy RP, et al. Molecular genetic evidence for a common clonal origin of urinary bladder small cell carcinoma and coexisting urothelial carcinoma. Am J Pathol. 2005;166(5):1533–9.
Chang MT, Penson A, Desai NB, et al. Small-cell carcinomas of the bladder and lung are characterized by a convergent but distinct pathogenesis. Clin Cancer Res. 2018;24(8):1965–73. https://doi.org/10.1158/1078-0432.CCR-17-2655.
Wang Y, Li Q, Wang J, et al. Small cell carcinoma of the bladder: the characteristics of molecular alterations, treatment, and follow-up. Med Oncol. 2019;36(12):98. https://doi.org/10.1007/s12032-019-1321-x.
Zheng X, Zhuge J, Bezerra SM, et al. High frequency of TERT promoter mutation in small cell carcinoma of bladder, but not in small cell carcinoma of other origins. J Hematol Oncol. 2014;7(1):47. https://doi.org/10.1186/s13045-014-0047-7.
Sjödahl G. Molecular subtype profiling of urothelial carcinoma using a subtype-specific immunohistochemistry panel. Methods Mol Biol. 1655;2018:53–64. https://doi.org/10.1007/978-1-4939-7234-0_5.
Kim IE, Amin A, Wang LJ, Cheng L, Perrino CM. Insulinoma-associated protein 1 (INSM1) expression in small cell neuroendocrine carcinoma of the urinary tract. Appl Immunohistochem Mol Morphol. Published online December 23, 2019. https://doi.org/10.1097/PAI.0000000000000824.
Lan MS, Breslin MB. Structure, expression, and biological function of INSM1 transcription factor in neuroendocrine differentiation. FASEB J. 2009;23:2024–33.
Soriano P, Navarro S, Gil M, Llombart-Bosch A. Small-cell carcinoma of the urinary bladder. A clinico-pathological study of ten cases. Virchows Arch. 2004;445(3):292–7. https://doi.org/10.1007/s00428-004-1041-1.
Blomjous CE, Vos W, Schipper NW, De Voogt HJ, Baak JP, Meijer CJ. Morphometric and flow cytometric analysis of small cell undifferentiated carcinoma of the bladder. J Clin Pathol. 1989;42(10):1032–9. https://doi.org/10.1136/jcp.42.10.1032.
Blomjous CE, Vos W, De Voogt HJ, Van der Valk P, Meijer CJ. Small cell carcinoma of the urinary bladder. A clinicopathologic, morphometric, immunohistochemical, and ultrastructural study of 18 cases. Cancer. 1989;64(6):1347–57. https://doi.org/10.1002/1097-0142(19890915)64:6<1347::aid-cncr2820640629>3.0.co;2-q.
Bezerra SM, Lotan TL, Faraj SF, et al. GATA3 expression in small cell carcinoma of bladder and prostate and its potential role in determining primary tumor origin. Hum Pathol. 2014;45(8):1682–7. https://doi.org/10.1016/j.humpath.2014.04.011.
Li W, Liang Y, Deavers MT, et al. Uroplakin II is a more sensitive immunohistochemical marker than uroplakin III in urothelial carcinoma and its variants. Am J Clin Pathol. 2014;142(6):864–71. https://doi.org/10.1309/AJCP1J0JPJBPSUXF.
Paner GP, Lopez-Beltran A, Sirohi D, Amin MB. Updates in the pathologic diagnosis and classification of epithelial neoplasms of urachal origin. Adv Anat Pathol. 2016;23(2):71–83. https://doi.org/10.1097/PAP.0000000000000110.
Fernández-Aceñero MJ, Córdova S, Manzarbeitia F, Medina C. Immunohistochemical profile of urothelial and small cell carcinomas of the bladder. Pathol Oncol Res. 2011;17(3):519–23. https://doi.org/10.1007/s12253-010-9341-z.
Iczkowski KA, Shanks JH, Bostwick DG. Loss of CD44 variant 6 expression differentiates small cell carcinoma of urinary bladder from urothelial (transitional cell) carcinoma. Histopathology. 1998;32(4):322–7. https://doi.org/10.1046/j.1365-2559.1998.00398.x.
Neşe N, Kumbaraci BS, Baydar DE, et al. Small cell carcinomas of the bladder highly express somatostatin receptor type 2A: impact on prognosis and treatment—a multicenter study of Urooncology society, Turkey. Appl Immunohistochem Mol Morphol. 2016;24(4):253–60. https://doi.org/10.1097/PAI.0000000000000188.
Gurel B, Ali TZ, Montgomery EA, et al. NKX3.1 as a marker of prostatic origin in metastatic tumors. Am J Surg Pathol. 2010;34(8):1097–105. https://doi.org/10.1097/PAS.0b013e3181e6cbf3.
Varinot J, Cussenot O, Roupret M, et al. HOXB13 is a sensitive and specific marker of prostate cells, useful in distinguishing between carcinomas of prostatic and urothelial origin. Virchows Arch. 2013;463(6):803–9. https://doi.org/10.1007/s00428-013-1495-0.
Akdeniz E, Bakirtas M, Bolat MS, Akdeniz S, Özer I. Pure large cell neuroendocrine carcinoma of the bladder without urological symptoms. Pan Afr Med J. 2018;30:134. https://doi.org/10.11604/pamj.2018.30.134.13437.
Martín IJP, Vilar DG, Aguado JM, et al. Large cell neuroendocrine carcinoma of the urinary bladder. Bibliographic review. Arch Esp Urol. 2011;64(2):105–13.
Watson GA, Ahmed Y, Picardo S, et al. Unusual Sites of High-Grade Neuroendocrine Carcinomas: A Case Series and Review of the Literature. Am J Case Rep. 2018;19:710–23. https://doi.org/10.12659/AJCR.908953.
Sari A, Ermete M, Sadullahoğlu C, Bal K, Bolükbaşi A. Large cell neuroendocrine carcinoma of urinary bladder; case presentation. Turk Patoloji Derg. 2013;29(2):138–42. https://doi.org/10.5146/tjpath.2013.01165.
Radović N, Turner R, Bacalja J. Primary “Pure” Large Cell Neuroendocrine Carcinoma of the Urinary Bladder: A Case Report and Review of the Literature. Clinical Genitourinary Cancer. 2015;13(5):e375–e377. https://doi.org/10.1016/j.clgc.2015.03.005.
Colarossi C, Pino P, Giuffrida D, et al. Large cell neuroendocrine carcinoma (LCNEC) of the urinary bladder: a case report. Diagn Pathol. 2013;8:19. https://doi.org/10.1186/1746-1596-8-19.
Liu C, Mo C-Q, Jiang S-J, Pan J-C, Qiu S-P, Wang D-H. Primary paraganglioma of seminal vesicle. Chin Med J. 2016;129(13):1627–8. https://doi.org/10.4103/0366-6999.184471.
Liu H-W, Liu L-R, Cao D-H, Wei Q. Paraganglioma in the renal pelvis. Kaohsiung J Med Sci. 2014;30(6):319–20. https://doi.org/10.1016/j.kjms.2013.04.007.
Awasthi NP, Kumari N, Krishnani N, Goel A. “Functional” paraganglioma of ureter: an unusual case. Indian J Pathol Microbiol. 2011;54(2):405–6. https://doi.org/10.4103/0377-4929.81631.
Alataki D, Triantafyllidis A, Gaal J, et al. A non-catecholamine-producing sympathetic paraganglioma of the spermatic cord: the importance of performing candidate gene mutation analysis. Virchows Arch. 2010;457(5):619–22. https://doi.org/10.1007/s00428-010-0966-9.
Yi C, Han L, Yang R, Yu J. Paraganglioma of the renal pelvis: a case report and review of literature. Tumori. 2017;103(Suppl. 1):e47–9. https://doi.org/10.5301/tj.5000677.
Kwon A-Y, Kang H, An HJ, et al. Spermatic cord paraganglioma with histologically malignant features. Urology. 2016;93:e7–8. https://doi.org/10.1016/j.urology.2016.03.014.
Alvarenga CA, Lopes JM, Vinagre J, et al. Paraganglioma of seminal vesicle and chromophobe renal cell carcinoma: a case report and literature review. Sao Paulo Med J. 2012;130(1):57–60.
Alberti C. Urology pertinent neuroendocrine tumors: focusing on renal pelvis, bladder, prostate located sympathetic functional paragangliomas. G Chir. 2016;37(2):55–60.
Cheng L, Leibovich BC, Cheville JC, et al. Paraganglioma of the urinary bladder: can biologic potential be predicted? Cancer. 2000;88(4):844–52. https://doi.org/10.1002/(sici)1097-0142(20000215)88:4<844::aid-cncr15>3.0.co;2-i.
Adraktas D, Caserta M, Tchelepi H. Paraganglioma of the urinary bladder. Ultrasound Q. 2014;30(3):233–5. https://doi.org/10.1097/RUQ.0000000000000113.
Liang J, Li H, Gao L, Yin L, Yin L, Zhang J. Bladder paraganglioma: clinicopathology and magnetic resonance imaging study of five patients. Urol J. 2016;13(2):2605–11.
Feng N, Li X, Gao H-D, Liu Z-L, Shi L-J, Liu W-Z. Urinary bladder malignant paraganglioma with vertebral metastasis: a case report with literature review. Chin J Cancer. 2013;32(11):624–8. https://doi.org/10.5732/cjc.012.10317.
Pichler R, Heidegger I, Klinglmair G, et al. Unrecognized paraganglioma of the urinary bladder as a cause for basilar-type migraine. Urol Int. 2014;92(4):482–7. https://doi.org/10.1159/000348829.
Hanji AM, Rohan VS, Patel JJ, Tankshali RA. Pheochromocytoma of the urinary bladder: a rare cause of severe hypertension. Saudi J Kidney Dis Transpl. 2012;23(4):813–6. https://doi.org/10.4103/1319-2442.98167.
Bagchi A, Dushaj K, Shrestha A, et al. Urinary bladder paraganglioma presenting as micturition-induced palpitations, dyspnea, and angina. Am J Case Rep. 2015;16:283–6. https://doi.org/10.12659/AJCR.891388.
She HL, Chan PH, Cheung SCW. Urinary bladder paraganglioma in a post-heart transplant patient. Ann Acad Med Singap. 2012;41(8):362–3.
Martucci VL, Lorenzo ZG, Weintraub M, et al. Association of urinary bladder paragangliomas with germline mutations in the SDHB and VHL genes. Urol Oncol. 2015;33(4):167.e13–20. https://doi.org/10.1016/j.urolonc.2014.11.017.
Ranaweera M, Chung E. Bladder paraganglioma: A report of case series and critical review of current literature. World J Clinic Cases. 2014;2(10):591. https://doi.org/10.12998/wjcc.v2.i10.591.
Rednam SP, Erez A, Druker H, et al. Von Hippel-Lindau and hereditary pheochromocytoma/paraganglioma syndromes: clinical features, genetics, and surveillance recommendations in childhood. Clin Cancer Res. 2017;23(12):e68–75. https://doi.org/10.1158/1078-0432.CCR-17-0547.
Raygada M, Pasini B, Stratakis CA. Hereditary paragangliomas. Adv Otorhinolaryngol. 2011;70:99–106. https://doi.org/10.1159/000322484.
Wang H, Ye H, Guo A, et al. Bladder paraganglioma in adults: MR appearance in four patients. Eur J Radiol. 2011;80(3):e217–20. https://doi.org/10.1016/j.ejrad.2010.09.020.
Bosserman AJ, Dai D, Lu Y. Imaging characteristics of a bladder wall paraganglioma. Clin Nucl Med. 2019;44(1):66–7. https://doi.org/10.1097/RLU.0000000000002324.
Bishnoi K, Bora GS, Mavuduru RS, Devana SK, Singh SK, Mandal AK. Bladder paraganglioma: safe and feasible management with robot assisted surgery. J Robot Surg. 2016;10(3):275–8. https://doi.org/10.1007/s11701-016-0573-0.
Stigliano A, Lardo P, Cerquetti L, et al. Treatment responses to antiangiogenetic therapy and chemotherapy in nonsecreting paraganglioma (PGL4) of urinary bladder with SDHB mutation: a case report. Medicine (Baltimore). 2018;97(30):e10904. https://doi.org/10.1097/MD.0000000000010904.
Nayyar R, Singh P, Gupta NP. Robotic management of pheochromocytoma of the vesicoureteric junction. JSLS. 2010;14(2):309–12. https://doi.org/10.4293/108680810X12785289145042.
Park S, Kang SY, Kwon GY, et al. Clinicopathologic characteristics and mutational status of succinate dehydrogenase genes in paraganglioma of the urinary bladder: a multi-institutional Korean study. Arch Pathol Lab Med. 2017;141(5):671–7. https://doi.org/10.5858/arpa.2016-0403-OA.
Papathomas TG, de Krijger RR, Tischler AS. Paragangliomas: update on differential diagnostic considerations, composite tumors, and recent genetic developments. Semin Diagn Pathol. 2013;30(3):207–23. https://doi.org/10.1053/j.semdp.2013.06.006.
Maeda M, Funahashi Y, Katoh M, Fujita T, Tsuruta K, Gotoh M. Malignant bladder pheochromocytoma with SDHB genetic mutation. Aktuelle Urol. 2013;44(5):381–2. https://doi.org/10.1055/s-0033-1345147.
Beilan J, Lawton A, Hajdenberg J, Rosser CJ. Locally advanced paraganglioma of the urinary bladder: a case report. BMC Res Notes. 2013;6:156. https://doi.org/10.1186/1756-0500-6-156.
Iwamoto G, Kawahara T, Tanabe M, et al. Paraganglioma in the bladder: a case report. J Med Case Rep. 2017;11(1):306. https://doi.org/10.1186/s13256-017-1473-2.
Menon S, Goyal P, Suryawanshi P, et al. Paraganglioma of the urinary bladder: a clinicopathologic spectrum of a series of 14 cases emphasizing diagnostic dilemmas. Indian J Pathol Microbiol. 2014;57(1):19–23. https://doi.org/10.4103/0377-4929.130873.
Miettinen M, McCue PA, Sarlomo-Rikala M, et al. GATA3: a multispecific but potentially useful marker in surgical pathology: a systematic analysis of 2500 epithelial and nonepithelial tumors. Am J Surg Pathol. 2014;38(1):13–22. https://doi.org/10.1097/PAS.0b013e3182a0218f.
Nonaka D, Wang BY, Edmondson D, Beckett E, Sun C-CJ. A study of gata3 and phox2b expression in tumors of the autonomic nervous system. Am J Surg Pathol. 2013;37(8):1236–41. https://doi.org/10.1097/PAS.0b013e318289c765.
So JS, Epstein JI. GATA3 expression in paragangliomas: a pitfall potentially leading to misdiagnosis of urothelial carcinoma. Mod Pathol. 2013;26(10):1365–70. https://doi.org/10.1038/modpathol.2013.76.
Ghafoor A-U-R, Yousaf I, Pervez R, Khan RU, Mir K. Paraganglioma of urinary bladder: an unusual presentation. Pitfalls in diagnosis and treatment. J Pak Med Assoc. 2012;62(1):63–5.
Grignon DJ, Ro JY, Mackay B, et al. Paraganglioma of the urinary bladder: immunohistochemical, ultrastructural, and DNA flow cytometric studies. Hum Pathol. 1991;22(11):1162–9.
Ranaweera M, Chung E. Bladder paraganglioma: a report of case series and critical review of current literature. World J Clin Cases. 2014;2(10):591–5. https://doi.org/10.12998/wjcc.v2.i10.591.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Shehabeldin, A.N., Ro, J.Y. (2021). Neuroendocrine Tumors of the Urinary Bladder. In: Zhou, H., Guo, C.C., Ro, J.Y. (eds) Urinary Bladder Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-71509-0_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-71509-0_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71508-3
Online ISBN: 978-3-030-71509-0
eBook Packages: MedicineMedicine (R0)