Abstract
Supportive care during curative treatment of head and neck cancer patients has different scopes: reducing the burden of acute toxicities and limiting the risk of developing late adverse effects; increasing the quality of life of the patients; allowing to perform optimal curative therapy, maintaining treatment dose intensity; preventing higher grade toxicities so to reduce also the costs associated with hospitalization, examinations, visits and use of drugs. At the same time, it is necessary to give uniformity in the supportive care protocols, as these preventive and therapeutic measures may influence the results of oncological treatments and their efficacy should be evaluated in a consistent manner. Several preventive and therapeutic interventions are available, particularly in the context of chemoradiotherapy, where the adverse events are more prominent. An accurate evaluation of the patient and a tailored approach with preventative indications and therapeutic interventions represent key factors. This approach could be easily identified within a “simultaneous care” strategy, as the optimal supportive measures are provided concurrently to the best therapeutic approach since the beginning of the treatment.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others

Keywords
Introduction
Supportive care given during cancer treatment has several aims. Reducing the burden of toxicities and anticipating their appearance by adopting adequate preventative measures; improving quality of life by relieving symptoms induced by the treatment or the disease itself and allowing to maintain a correct dose intensity, therefore, giving the patient the optimal chance to be cured [1].
According to the principles of Multinational Association of Supportive Care in Cancer (MASCC), “supportive care makes excellent cancer care possible”. Oncological treatments of head and neck cancer (HNC) performed with curative intent represent one of the most intensive therapies in terms of adverse events and of psychological distress [2]. Therefore, it is essential to accompany the curative treatment with all the measures that could relief patient’s symptoms.
Reasons to Implement Supportive Care during Curative Treatment in Head and Neck Cancer
The importance of supportive care in HNC during curative approaches could be grouped into 6 main reasons:
-
1.
Reduction of acute toxicity
-
2.
Reduction of late effects
-
3.
Increase of compliance—maintain dose intensity
-
4.
Improvement of quality of life
-
5.
Reduction of costs
-
6.
Homogeneity and consistency in clinical trials
First, the possible reduction of acute toxicities. The burden of acute toxicities during radiotherapy with or without chemotherapy, performed either in the definitive or the adjuvant setting is well-known [3]. The most frequent acute toxicities reported are represented by mucositis, dysphagia, weight loss, anorexia, infections, dermatitis, nausea and vomiting. The adoption of preventative actions to reduce the severity and duration of these toxicities may be beneficial. However, another way to indicate the consequences of the burden of toxicities induced by treatment in HNC is considering the rate of toxic deaths. Mortality due to therapies mirrors the toxicity of the treatment itself and it could be considered both in the acute (occurring during treatment) or in subacute period (in the period of 30 days after treatment completion). In Table 15.1, the rate of toxic death occurring in some clinical trials in HNC patients is depicted. It should be considered that clinical trials are often offered to the most “fit” patients, without severe comorbidities; therefore, the rate of death due to cancer treatment toxicities could be also higher in the real-life setting. Moreover, elderly cancer patients, even if treated with less intensive treatments, frequently avoiding chemotherapy or substituting cisplatin with less toxic carboplatin, are at a higher risk of acute toxicities and treatment-induced death. In a recent analysis, patients ≥70 years showed a higher rate of hospitalization, greater adverse events and a lower 3-month overall survival than their younger counterparts [4].
When assessing acute, as well as late toxicities, it should be acknowledged that while locoregional relapse, distant recurrence and second primary tumors are quite frequent events in advanced cancer stages, patients with HNC are at the same time at risk for mortality due to adverse treatment effects or comorbid diseases [8, 16]. Mell et al. were able to identify several risk factors for competing mortality in advanced HNC: age, comorbid disease, BMI, sex and the distance that needs to be traveled to the treating center [16]. Interestingly, they observed large subsets of patients with similar disease-free survival, but at a markedly different risk for competing events. Moreover, they confirmed that older patients and patients with comorbidities were more prone to suffer from toxicities and not obtaining benefit from intensive treatments. This would translate into the need of tailoring the intensity of treatment according to patient’s functionality and frailty and, in parallel, activate personalized supportive care according to the identified needs.
The same group evaluated a large sample of patients from three randomized trials who were treated with radiation with or without systemic therapy [17]. They developed a nomogram to predict the group of patients who could selectively benefit from an intensive treatment. Factors involved in this definition were younger age, improved performance status, higher body mass index, node-positive status, p16-negative status, and oral cavity primary. These are the patients with a higher relative hazard for recurrence versus competing mortality (ω score positive ratio). On the flip side, we need to evaluate the best supportive intervention according to the patient’s risk of complication. Further applications of this nomogram in this regard are strongly awaited.
Supportive care strategies are also useful in increasing patient’s compliance to treatment and in allowing treatment dose intensity to be maintained. It is well known that interruptions in radiation therapy may jeopardize the outcome of the treatment itself. As the intensity of treatment escalates, adverse events also increase and along with the possibility of unplanned radiation treatment breaks and prolongationof the radiation treatment time [18]. These factors are associated with lower locoregional control rates. It has been estimated that tumor control rate is approximately 1% lower for every day of missed treatment [19, 20]. Similarly, dose intensity of concomitant chemotherapy is also of importance, as shown in several reports [21]. Cumulative cisplatin dose higher than 200 mg/m2 concurrently with radiation has been shown to offer higher probability of disease control and overall survival, at least in the population of HPV-negative cancers [21]. In this regard, optimal supportive care may ensure treatment continuity and allow for the best chance of cure.
Concurrent treatments profoundly impact on quality of life (QoL) of HNC patients during the acute phase of treatment. The score of several domains and patient-reported outcomes worsen throughout the course of treatment and slowly recover in the weeks that follow [22]. All the measures able to contain and limit QoL worsening and to potentially allow quick recovery to baseline or even to increase overall QoL represent an important help for patients. Often, patients’ burden of symptoms corresponds also to caregivers’ psychological issues [23]. In addition, caregivers should be offered specific support and stressful conditions should be identified early.
Sometimes, costs also represent a leverage to be used in discussing the importance of supportive care. It is true that reimbursement of new drugs represents a challenge for healthcare systems, but it should be considered that adverse events, due to treatment, may also lead to complications impacting on overall treatment costs. For instance, mucositis toxicity is associated with the adoption of preventive/therapeutic measures possibly increasing the overall treatment costs. The use of opioids to relieve mucositis-associated pain, the preventative or therapeutic placing of gastrostomy or nasogastric feeding tubes, and the increased risk of infections and the consequent need of antibiotics, antimycotic or antiviral drugs and resorting to hospitalization represent some of the interventions required to approach mucositis complications, all impacting on costs. When comparing patients experiencing severe (grade ≥ 3) vs non-severe (grade < 3) mucositis, costs of laboratory diagnostic tests, use of medications, imaging procedures, visits and inpatient hospitalizations were shown to be significantly higher for patients suffering of severe mucositis [24]. Therefore, cost–effectiveness of any new supportive care intervention should be an outcome that should be included in new clinical trials (see an example in [25] and in Fig. 15.1).
Design of a new trial with photobiomodulation, which considers cost-effectiveness parameters. Reproduced with permission from Springer Nature [26], under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium
Lastly, supportive care needs to be standardized as much as possible to offer homogeneity and consistency into clinical trials. Zafar et al. reported the importance of defining what the best supportive care is when performing randomized trials in advanced disease patients, also considering no active oncological treatment [27]. This could easily be transposed to randomized clinical trials in the setting of HNC curative treatments. In fact, if we want to perform trials with the aim to evaluate new compounds to be integrated with radiation therapy for HNC patients, we should be able to strictly ensure that supportive care employed in the intervention and in the experimental arm are the same. If they are different, this could constitute a bias that could preclude the analysis of results.
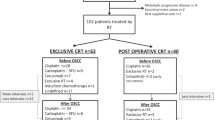
We advocate that in each trial in HNC, the supportive care measures would be clear, well defined and documented (Fig. 15.2).
Multiple Interventions for Different Aspects of Support
It is difficult to limit the interventions for supportive care to specific domains or signs and symptoms, as the process of care of the patient is comprehensive and considers the person as a whole. However, a list of the most frequent issues related to the treatment of HNC which could be object of a supportive approach is presented in Table 15.2.
Supportive care needs of patients with HNC profoundly differ between the period of curative treatment, the subacute phase and the period of follow-up in long-term survivorship. Patients immediately post-treatment show larger number of unmet needs compared with those in extended survivorship [28]. Psychological issues represent the most prevalent unmet needs, followed by pain and other physical symptoms. Patients in longer-term survivorship need more support regarding anxiety, changes in sexual relationships, and fear of death and dying.
As a detailed description of all the interventions available to support the patients during HNC treatment is out of the scope of this chapter, we will provide hereafter the last information about mucositis prevention and treatment, as an example of how to implement the care of the patient according to the latest literature data.
The Example of Mucositis: An Early and up-to-Date Supportive Care Intervention
Mucositis is one of the most distressing symptoms the patients are complaining about during curative treatment with radiation with or without systemic therapy. MASCC/ISOO developed the Clinical Practice Guidelines for the management of mucositis, with the first edition published in 2004 and periodically updated [29]. This represents the result of a systematic review of the literature, with studies rated according to the presence of major and minor flaws; the final guidelines are then developed into different levels of evidence [30]. We will present hereafter the changes in the guidelines, derived from the accurate revision of the literature; the other recommendations or suggestions remained unchanged since the previous version [29].
Basic oral care has been considered a key strategy in preventing mucositis. Specifically, implementation of multi-agent combination of oral care protocols has been shown to prevent mucositis in different settings of treatment, namely, with chemotherapy, radiation and hematopoietic stem cell transplantation [31]. Bland rinses should be employed, as they allow to increase oral clearance of debris, promote oral hygiene, and improve patient comfort during cancer therapy. The use of saline or sodium bicarbonate rinses may help improving oral clearance. Even if no guideline was possible to consistently suggest professional oral care due to lack of solid data, a dental evaluation and treatment is indicated prior to cancer therapy. In fact, the professional intervention may increase dental and oral cavity hygiene, removing possible causes of infections from odontogenic sources, which could be the door to systemic spread. In the process of oral care, patient (and caregivers) education has an important role, as it could ensure compliance to preventative and therapeutic suggestions.
In patients undergoing radiation or chemoradiation for HNC, the use of benzydamine mouthwashes is suggested, based on the results of several randomized clinical trials; at the moment, benzydamine is the only anti-inflammatory mouthwash with sufficient evidence in the guidelines [32]. On the contrary, the panel who evaluated the literature suggested not to use chlorhexidine as prevention of oral mucositis during radiotherapy for HNC.
The use of photobiomodulation (low-level laser therapy) has increased over the last few years and several studies have been reported with this tool with both preventive and therapeutic aims. Guidelines has recommended the use of intra-oral photobiomodulation in the prevention of mucositis during HNC radiation with or without chemotherapy [33]. The anti-inflammatory properties of low-level laser therapy may support its use, even if some concerns regarding facility requirements, trained personnel, and local regulatory requirements may limit its application. Moreover, standardization of protocols is required to expand the use of this tool. However, this approach may represent another weapon in the therapeutic armamentarium for prevention and treatment of mucositis and pain associated with mucositis.
Concerning treatment of pain due to mucositis, topical morphine 0.2% mouthwash is suggested as per indications coming from randomized clinical trials [34]. It has been shown that opioid receptors are present at the surface of injured mucosa and topical morphine could directly act on them. In this regard, further trials are needed to evaluate how to integrate topical and systemic opioid therapy and the impact of morphine mouthwashes in reducing the need of systemic administration of the same class of drugs.
There is also a suggestion in favor of the use of per os glutamine for the prevention of oral mucositis in patients with HNC treated with concurrent chemoradiation [35, 36]. Only a caution has been given, as the use of parenteral glutamine in another setting (hematopoietic stem cell transplantation) showed a higher mortality rate.
Guidelines also report negative suggestions and recommendations, as the results of clinical trials do not always support the use of a specific medication or treatment. For a complete picture of the new guidelines we refer to the full paper that has just been approved [37].
Conclusion
Supportive care needs to be integrated early in the course of treatment for HNC patients. Implementation of specific protocols is strongly recommended, therefore giving a comprehensive view on all the aspects of patient’s care. A tailored assessment of patient’s needs could help in identifying the aspects that should be sustained the most and the actions to be taken before starting the treatment itself. In this regard, the model of “simultaneous care” advocated at the beginning of the pathway of care of advanced cancer patients could also be used in the approach to HNC patients before starting curative treatment with radiation (with or without systemic therapy), in both the definitive and the adjuvant setting.However, the logistical organization and the possible benefit of simultaneous care embedded in HNC treatment have not been investigated yet and deserve to be assessed in well-conducted clinical trials.
References
Bonomo P, Paderno A, Mattavelli D, Zenda S, Cavalieri S, Bossi P. Quality assessment in supportive care in head and neck cancer. Front Oncol. 2019;9:926.
Haman KL. Psychologic distress and head and neck cancer: part 1--review of the literature. J Support Oncol. 2008;6(4):155–63.
Trotti A. Toxicity in head and neck cancer: a review of trends and issues. Int J Radiat Oncol Biol Phys. 2000;47(1):1–12. https://doi.org/10.1016/s0360-3016(99)00558-1.
Strom TJ, Naghavi AO, Trotti AM, Russell J, Kish JA, McCaffrey J, Otto KJ, Harrison LB, Caudell JJ. Increased acute mortality with chemoradiotherapy for locally advanced head and neck cancer in patients ≥70years. J Geriatr Oncol. 2017;8(1):50–5.
Brizel DM, Albers ME, Fisher SR, et al. Hyperfractionated irradiation with or without concurrent chemotherapy for locally advanced head and neck cancer. N Engl J Med. 1998;338(25):1798–804.
Calais G, Alfonsi M, Bardet E, et al. Randomized trial of radiation therapy versus concomitant chemotherapy and radiation therapy for advanced-stage oropharynx carcinoma. J Natl Cancer Inst. 1999;91(24):2081–6.
Adelstein DJ, Li Y, Adams GL, et al. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol. 2003;21(1):92–8.
Argiris A, Brockstein BE, Haraf DJ, et al. Competing causes of death and second primary tumors in patients with locoregionally advanced head and neck cancer treated with chemoradiotherapy. Clin Cancer Res. 2004;10:1956–62.
Adelstein DJ, Saxton JP, Rybicki LA, et al. Multiagent concurrent chemoradiotherapy for locoregionally advanced squamous cell head and neck cancer: mature results from a single institution. J Clin Oncol. 2006;24(7):1064–71.
Pfister DG, Su YB, Kraus DH, et al. Concurrent cetuximab, cisplatin, and concomitant boost radiotherapy for locoregionally advanced, squamous cell head and neck cancer: a pilot phase II study of a new combined-modality paradigm. J Clin Oncol. 2006;24(7):1072–8.
Bonner JA, Harari PM, Giralt J, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2006;354(6):567–78.
Givens DJ, Karnell LH, Gupta AK, et al. Adverse events associated with concurrent chemoradiation therapy in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 2009;135(12):1209–17.
Lefebvre JL, Rolland F, Tesselaar M, et al. Phase 3 randomized trial on larynx preservation comparing sequential vs alternating chemotherapy and radiotherapy. J Natl Cancer Inst. 2009;101(3):142–52.
Bourhis J, Sire C, Graff P, et al. Concomitant chemoradiotherapy versus acceleration of radiotherapy with or without concomitant chemotherapy in locally advanced head and neck carcinoma (GORTEC 99-02): an open-label phase 3 randomised trial. Lancet Oncol. 2012;13(2):145–53.
Ang KK, Zhang Q, Rosenthal DI, et al. Randomized phase III trial of concurrent accelerated radiation plus cisplatin with or without cetuximab for stage III to IV head and neck carcinoma: RTOG 0522. J Clin Oncol. 2014;32(27):2940–50.
Mell LK, Dignam JJ, Salama JK, et al. Predictors of competing mortality in advanced head and neck cancer. J Clin Oncol. 2010;28:15–20.
Mell LK, Shen H, Nguyen-Tân PF, et al. Nomogram to predict the benefit of intensive treatment for Locoregionally advanced head and neck cancer. Clin Cancer Res. 2019;25(23):7078–88.
Russo G, Haddad R, Posner M, Machtay M. Radiation treatment breaks and ulcerative mucositis in head and neck cancer. Oncologist. 2008;13:886–98.
Robertson AG, Robertson C, Perone C, et al. Effect of gap length and position on results of treatment of cancer of the larynx in Scotland by radiotherapy: a linear quadratic analysis. Radiother Oncol. 1998;48:165–73.
Suwinski R, Sowa A, Rutkowski T, et al. Time factor in postoperative radiotherapy: a multivariate locoregional control analysis in 868 patients. Int J Radiat Oncol Biol Phys. 2003;56:399–412.
Spreafico A, Huang SH, Xu W, et al. Impact of cisplatin dose intensity on human papillomavirus-related and -unrelated locally advanced head and neck squamous cell carcinoma. Eur J Canc. 2016;67:174e82.
Hanna EY, Mendoza TR, Rosenthal DI, et al. The symptom burden of treatment-naive patients with head and neck cancer. Cancer. 2015;121(5):766–73.
Karlsson T, Johansson M, Finizia C. Well-being of caregivers of patients with laryngeal cancer treated by radiotherapy. Int Arch Otorhinolaryngol. 2020;24(2):e170–4.
Nonzee NJ, Dandade NA, Patel U, et al. Evaluating the supportive care costs of severe radiochemotherapy-induced mucositis and pharyngitis: results from a Northwestern University costs of cancer program pilot study with head and neck and nonsmall cell lung cancer patients who received Care at a County Hospital, a veterans administration hospital, or a comprehensive cancer care center. Cancer. 2008;113:1446–52.
Antunes HS, Schluckebier LF, Herchenhorn D, et al. Cost-effectiveness of low-level laser therapy (LLLT) in head and neck cancer patients receiving concurrent chemoradiation. Oral Oncol. 2016;52:85–90.
Martins AFL, Nogueira TE, Morais MO, et al. Effect of photobiomodulation on the severity of oral mucositis and molecular changes in head and neck cancer patients undergoing radiotherapy: a study protocol for a cost-effectiveness randomized clinical trial. Trials. 2019;20:97.
Zafar SY, Currow DC, Cherny N, et al. Consensus-based standards for best supportive care in clinical trials in advanced cancer. Lancet Oncol. 2012;13:e77–82.
Henry M, Alias A, Cherba M et al. Immediate post-treatment supportive care needs of patients newly diagnosed with head and neck cancer. Support Care Cancer 2020 Mar 18.
Lalla RV, Bowen J, Barasch A, et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. 2014;120:1453–61.
Ranna V, Cheng KKF, Castillo DA, et al. Development of the MASCC/ISOO clinical practice guidelines for mucositis: an overview of the methods. Support Care Cancer. 2019;27:3933–48.
Hong CHL, Gueiros LA, Fulton JS, et al. Systematic review of basic oral care for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2019;27:3949–67.
Ariyawardana A, Cheng KKF, Kandwal A, et al. Systematic review of anti-inflammatory agents for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2019;27:3985–95.
Zadik Y, Arany PR, Fregnani ER, et al. Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2019;27:3969–83.
Saunders DP, Rouleau T, Cheng K, et al. Systematic review of antimicrobials, mucosal coating agents, anesthetics, and analgesics for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2020;28:2473–84.
Yarom N, Hovan A, Bossi P, et al. Systematic review of natural and miscellaneous agents for the management of oral mucositis in cancer patients and clinical practice guidelines-part 1: vitamins, minerals, and nutritional supplements. Support Care Cancer. 2019;27:3997–4010.
Yarom N, Hovan A, Bossi P, et al. Systematic review of natural and miscellaneous agents, for the management of oral mucositis in cancer patients and clinical practice guidelines – part 2: honey, herbal compounds, saliva stimulants, probiotics, and miscellaneous agents. Support Care Cancer. 2020;28:2457–72.
Elad S, Cheng KKF, Lalla RV et al. The MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 2020, submitted.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this paper
Cite this paper
Bossi, P., Lorini, L. (2021). Optimal Supportive Measures during Primary Treatment. In: Vermorken, J.B., Budach, V., Leemans, C.R., Machiels, JP., Nicolai, P., O’Sullivan, B. (eds) Critical Issues in Head and Neck Oncology. Springer, Cham. https://doi.org/10.1007/978-3-030-63234-2_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-63234-2_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-63233-5
Online ISBN: 978-3-030-63234-2
eBook Packages: MedicineMedicine (R0)