Abstract
Paroxysmal exercise-induced dyskinesia (PED) is a clinical syndrome manifesting with recurrent attacks of dystonia usually lasting between 15 and 40 min, although exceptions are possible, and that are brought on by sustained exercise. Over the last years, the etiological spectrum of PED has been increasingly expanding to include a number of genetic disorders, some of which are treatable conditions.
In the current chapter, we will provide an overview of the different conditions associated with PED and propose a workup to reach a definitive diagnosis, upon which treatment options heavily rely.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Lance JW. Familial paroxysmal dystonic choreoathetosis and its differentiation from related syndromes. Ann Neurol. 1977;2:285–93.
Suls A, Dedeken P, Goffin K, et al. Paroxysmal exercise-induced dyskinesia and epilepsy is due to mutations in SLC2A1, encoding the glucose transporter GLUT1. Brain. 2008;131(Pt 7):1831–44.
Weber YG, Storch A, Wuttke TV, et al. GLUT1 mutations are cause of paroxysmal exertion-induced dyskinesias and induce hemolytic anemia by a cation leak. J Clin Invest. 2008;118(6):2157–68.
Schneider SA, Paisan-ruiz C, Garcia-gorostiaga I, et al. GLUT1 gene mutations cause sporadic paroxysmal exercise-induced dyskinesias. Mov Disord. 2009;24:1684–96.
Erro R, Stamelou M, Ganos C, et al. The clinical syndrome of paroxysmal exercise-induced dystonia: diagnostic outcomes and an algorithm. Mov Disord Clin Pract. 2014;1:57–61.
Yang H, Wang D, Engelstad K, et al. Glut1 deficiency syndrome and erythrocyte glucose uptake assay. Ann Neurol. 2011;70:996–1005.
Leen WG, Klepper J, Verbeek MM, et al. Glucose transporter-1 deficiency syndrome: the expanding clinical and genetic spectrum of a treatable disorder. Brain. 2010;133:655–70.
Erro R, Sheerin UM, Bhatia KP. Paroxysmal dyskinesias revisited: a review of 500 genetically proven cases and a new classification. Mov Disord. 2014;29(9):1108–16.
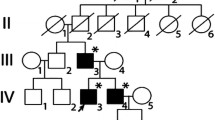
Rotstein M, Engelstad K, Yang H, et al. Glut1 deficiency: inheritance pattern determined by haploinsufficiency. Ann Neurol. 2010;68:955–8.
Gardiner AR, Jaffer F, Dale RC, et al. The clinical and genetic heterogeneity of paroxysmal dyskinesias. Brain. 2015;138:3567–80.
Ohshiro-Sasaki A, Shimbo H, Takano K, et al. A three-year-old boy with glucose transporter type 1 deficiency syndrome presenting with episodic ataxia. Pediatr Neurol. 2014;50:99–100.
Reis S, Matias J, Machado R, et al. Paroxysmal ocular movements – an early sign in Glut1 deficiency syndrome. Metab Brain Dis. 2018;33:1381–83.
Klepper J, Leiendecker B, Eltze C, et al. Paroxysmal nonepileptic events in Glut1 deficiency. Mov Disord Clin Pract. 2016;3(6):607–10.
Ramm-Pettersen A, Nakken KO, Skogseid IM, et al. Good outcome in patients with early dietary treatment of GLUT-1 deficiency syndrome: results from a retrospective Norwegian study. Dev Med Child Neurol. 2013;55(5):440–7.
Leen WG, Mewasingh L, Verbeek MM, et al. Movement disorders in GLUT1 deficiency syndrome respond to the modified Atkins diet. Mov Disord. 2013;28(10):1439–42.
Guimaraes J, Vale SJ. Paroxysmal dystonia induced by exercise and acetazolamide. Eur J Neurol. 2000;7(2):237–40.
Baschieri F, Batla A, Erro R, et al. Paroxysmal exercise-induced dystonia due to GLUT1 mutation can be responsive to levodopa: a case report. J Neurol. 2014;261(3):615–6.
Wijemanne S, Jankovic J. Dopa-responsive dystonia--clinical and genetic heterogeneity. Nat Rev Neurol. 2015;11:414–24.
Dale RC, Melchers A, Fung VS, et al. Familial paroxysmal exercise-induced dystonia: atypical presentation of autosomal dominant GTP-cyclohydrolase 1 deficiency. Dev Med Child Neurol. 2010;52:583–6.
Peters H, Buck N, Wanders R, et al. ECHS1 mutations in Leigh disease: a new inborn error of metabolism affecting valine metabolism. Brain. 2014;137:2903–8.
Haack TB, Jackson CB, Murayama K, et al. Deficiency of ECHS1 causes mitochondrial encephalopathy with cardiac involvement. Ann Clin Transl Neurol. 2015;2:492–509.
Korenke GC, Nuoffer J-M, Alhaddad B, et al. Paroxysmal dyskinesia in ECHS1 defect with globus pallidus lesions. Neuropediatrics. 2016;47.
Olgiati S, Skorvanek M, Quadri M, et al. Paroxysmal exercise-induced dystonia within the phenotypic spectrum of ECHS1 deficiency. Mov Disord. 2016;31:1041–8.
Mahajan A, Constantinou J, Sidiropoulos C. ECHS1 deficiency-associated paroxysmal exercise-induced dyskinesias: case presentation and initial benefit of intervention. J Neurol. 2017;264:185–7.
Patel KP, O’Brien TW, Subramony SH, et al. The spectrum of pyruvate dehydrogenase complex deficiency: clinical, biochemical and genetic features in 371 patients. Mol Genet Metab. 2012;106:385–94.
Friedman J, Feigenbaum A, Chuang N, et al. Pyruvate dehydrogenase complex-E2 deficiency causes paroxysmal exercise-induced dyskinesia. Neurology. 2017;89(22):2297–8.
McWilliam CA, Ridout CK, Brown RM, et al. Pyruvate dehydrogenase E2 deficiency: a potentially treatable cause of episodic dystonia. Eur J Paediatr Neurol. 2010;14:349–53.
Castiglioni C, Verrigni D, Okuma C, et al. Pyruvate dehydrogenase deficiency presenting as isolated paroxysmal exercise induced dystonia successfully reversed with thiamine supplementation. Case report and mini-review. Eur J Paediatr Neurol. 2015;19:497–503.
Barnerias C, Saudubray JM, Touati G, et al. Pyruvate dehydrogenase complex deficiency: four neurological phenotypes with differing pathogenesis. Dev Med Child Neurol. 2010;52:e1–9.
Bruno M, Ravina B, Garraux G, et al. Exercise-induced dystonia as a preceding symptom of familial Parkinson’s disease. Mov Disord. 2004;19:228–30.
Bozi M, Bhatia KP. Paroxysmal exercise-induced dystonia as a presenting feature of young-onset Parkinson’s disease. Mov Disord. 2003;18:1545–7.
Yoshimura K, Kanki R. Child-onset paroxysmal exercise-induced dystonia as the initial manifestation of hereditary Parkinson’s disease. Parkinsonism Relat Disord. 2018;49:108–9.
Leen WG, Wevers RA, Kamsteeg E-J, et al. Cerebrospinal fluid analysis in the workup of GLUT1 deficiency syndrome: a systematic review. JAMA Neurol. 2013;70:1440–4.
Di Fonzo A, Monfrini E, Erro R. Genetics of movement disorders and the practicing clinician; who and what to test for? Curr Neurol Neurosci Rep. 2018;18(7):37.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic Supplementary Material
A 19-year-old girl with SLC2A1 mutations, whose baseline gait demonstrates mild spasticity of her right leg. An attack of PED is shown. (Originally appeared in Erro et al. [5])
There are no abnormalities when initiating cycling, while after 10 min a unilateral PED attack in the left foot occurs in a patient with early-onset PD. (Originally appeared in Erro et al. [5]) (MOV 9470 kb)
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Scannapieco, S., Erro, R. (2021). Paroxysmal Exercise-Induced Dyskinesia. In: Sethi, K.D., Erro, R., Bhatia, K.P. (eds) Paroxysmal Movement Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-53721-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-53721-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53720-3
Online ISBN: 978-3-030-53721-0
eBook Packages: MedicineMedicine (R0)